In December 2019, an outbreak of a novel coronavirus (severe acute respiratory syndrome coronavirus 2 [SARS-CoV-2]) was reported, having originated in Wuhan, Hubei province, China.
Most studies on the subject performed to date have focused on adult patients, and the current evidence on the pediatric population is scarce, especially when it comes to newborns.1,2 In Spain, one of the epicenters of the pandemic, as many as 146,690 cases have been reported.
We present a case of horizontal transmission of infection by SARS-CoV-2 in a male neonate aged 10 days confirmed by a positive real-time reverse transcriptase polymerase chain reaction (RT-PCR) test for SARS-CoV-2, describing the clinical presentation, diagnosis, treatment and outcome of the patient.
Clinical case: male neonate aged 10 days brought to the primary care center with fever, with a rectal temperature of 38.5°C and no other symptoms, with good tolerance of formula feeding. The neonate was referred to the emergency department and admitted to hospital to evaluate the fever without a source. The mother, aged 26 years, had received prenatal care, with normal antenatal ultrasounds and a spontaneous vaginal delivery at 392+ weeks of gestation, in the absence of perinatal risk factors for infection (negative for β-haemolytic streptococcus and a total duration of ruptured of membranes of 4h), a birth weight of 3220g and Apgar scores of 10/10.
The relevant history consisted of a household environment with the father, mother and paternal grandfather experiencing cold symptoms, cough and nasal discharge in the absence of fever.
The evaluation included blood tests, blood culture, urinalysis, lumbar puncture, collection of nasopharyngeal aspirate to test for the presence of adenovirus, influenza A and B, respiratory syncytial virus and SARS-CoV-2 with the RT-PCR test. Empiric antibiotherapy was initiated while awaiting the results of culture and viral testing.
The results of the tests performed at admission were as follows: complete blood count with normal red blood cell indices, a white blood cell count of 7.4×109/L with 40.5% lymphocytes and 21.6% monocytes; procalcitonin, 0.20ng/mL; C-reactive protein <5mg/L; normal findings of examination of cerebrospinal fluid and normal findings of urinalysis. The RT-PCR test was positive for SARS-CoV-2 and negative for all other viruses. Given this result, both parents underwent the RT-PCR test for SARS-CoV-2, which turned out positive.
At admission, the infant presented with a temperature of 36.9°C, a heart rate (HR) of 144bpm, a respiratory rate (RR) of 42bpm and an oxygen saturation of 100% in room air, well-appearing, with good peripheral perfusion and good bilateral inspiration without no abnormal breath sounds.
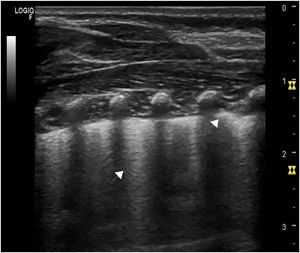
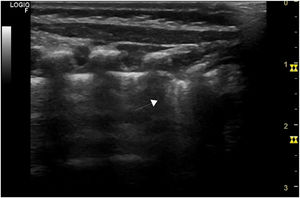
At 24h from admission, the RR increased to 60bpm and the HR in the 160–180bpm range, which prompted performance of a chest X-ray and echocardiography, both with normal findings, and a chest ultrasound that revealed pleural thickening, converging B-lines in the posterior chest and subpleural consolidation at the lung base level of the right hemithorax (Figs. 1 and 2). Subsequently, the patient developed apnoea, and capillary blood gas analysis detected mild carbon dioxide retention (pH, 7.38; pCO2, 48.4, bicarbonate, 26.4; lactate, 1.2), leading to initiation of treatment with caffeine and administration of supplemental oxygen in the incubator with a peak FiO2 of 0.3. On day 3 from admission, antibiotherapy was discontinued on account of the negative culture results, and the patient showed clinical improvement with a gradual decrease in oxygen requirements and resolution of apnoea, and he was discharged at 9 days from admission. Serological tests conducted at admission were IgM− and IgG−, with evidence of seroconversion at day 16 from onset (IgM−, IgG+).
The case presented here was a case of horizontal transmission, as the patient lived with other 8 individuals in the household, of who 3 reported cold symptoms, which led to testing of household members despite the absence of fever.
We ought to highlight the importance of the chest ultrasound, an aspect that has not been described in previously published pediatric cases, as it detects abnormalities at an earlier stage compared to the X-ray. In our patient, it revealed abnormalities before the development of apnoeic episodes and need for supplemental oxygen, abnormalities that were undetectable in the plain radiograph, and it is the method currently used in the triage of adult patients with suspected coronavirus disease 2019 (COVID-19).3 We did not find evidence of the gastrointestinal symptoms described in other cases.4
Further research is required to establish the lung ultrasound features found in patients with COVID-19 and the course of the disease in the neonatal population, and any household members with mild cold symptoms should be tested to prevent transmission in this age group. In the context of the current pandemic, it is important to include the RT-PCR test for detection of SARS-CoV-2 infection in the assessment of the febrile neonate, as indicated by current protocols,5 taking into account the role of the viral load in this age group as it is done in adults.6
Please cite this article as: Pineda Caplliure A, Porcar Almela M, Navarro Albert A, Muñoz Vicente E, Mansilla Roig B. Utilidad de la ecografía torácica en infección neonatal por SARS-CoV-2. An Pediatr (Barc). 2021;94:412–413.