Henna tattoos are a very common practice in the adolescent population. Henna is very often admixed with para-phenylenediamine (PPDA) to improve the appearance of the tattoo. PPDA is a potent allergen, and is a frequent cause of allergic contact dermatitis (ACD).
Material and methodA study was conducted on the results of 726 consecutive children who had been patch tested in the University General Hospital Consortium of Valencia between 1980 and 2015.
ResultsAlmost half (49.7%; (361 cases) of the children had one or more positive patch test findings, with 4.7% (34) being allergic to PPDA. Mean age of patients allergic to PPDA was 12.4 years, and 44.2% were male. There were 2 cases (5.9%) of atopic dermatitis. Of the positive reactions, 73.5% were considered to be current clinically relevant. The sensitisation origin was a Henna tattoo in 50% of cases.
ConclusionPPDA sensitisation is relatively common in the child and adolescent population. The most frequent origin is the performing of Henna tattoos adulterated with PPDA. Adolescents are at the higher risk of developing ACD due to Henna tattoos. Henna tattooing should be strongly discouraged in children.
Los tatuajes con henna son una práctica común en la población adolescente. En la mayoría de las ocasiones, la henna se mezcla con parafenilendiamina (PPDA) para mejorar las características del tatuaje. La PPDA es un potente alérgeno que causa con frecuencia dermatitis alérgica de contacto.
Material y métodoSe recogió a 726 niños parcheados en la Unidad de Alergia del Hospital General Universitario de Valencia entre 1980 y 2015, identificándose los casos y revisando los resultados de las pruebas, así como datos clínicos y epidemiológicos.
ResultadosTrescientos sesenta y un niños (49,7%) demostraron sensibilización a al menos un alérgeno y 34 fueron alérgicos a la PPDA (4,68%). La edad media de los pacientes alérgicos a PPDA fue de 12,4 años. El 44,2% de los niños alérgicos eran varones. Dos pacientes (5,9%) presentaron antecedentes personales de atopia. El 73,5% de reacciones positivas a PPDA se consideraron de relevancia presente. El origen de la sensibilización fue la realización de un tatuaje con henna en el 50% de los pacientes.
ConclusiónLa sensibilización a PPDA es relativamente frecuente en la población pediátrica. El origen más frecuente es la realización de tatuajes con henna adulterada. Los adolescentes son la población con mayor riesgo de presentar este tipo de reacciones. Se debe desaconsejar activamente la práctica de tatuajes con henna negra en la población pediátrica.
Henna is a pigment extracted from the Lawsonia inermis plant. Because of its ochre hue, it has been used for centuries in different cultures to dye skin, nails or hair.1 It has a low reactogenicity and reports of cases of allergic contact dermatitis caused by henna are extremely rare.2,3
In recent years, temporary tattoos with henna have become very popular among children and adolescents. However, the brownish hue, low contrast and short duration of staining make the results obtained with the pigment unsatisfactory. As a result, para-phenylenediamine (PPD) is commonly added to the henna mixture to speed up drying, improve contrast and darken the hue, so that designs look more like permanent tattoos. The resulting product from this mixture is known as black henna.4–6
Para-phenylenediamine is a disperse dye with a deep black hue. Its oxidised form is innocuous, but in everyday use it is never fully oxidised. Under these circumstances, it is a potent contact allergen, included in the “Top 5” list of strong sensitisers of the Food and Drug Administration.6
At present, the use of PPD in topical products is banned in the European Union (with the exception of PPD in hair dyes at a concentration of 6%).7 In spite of this, there are still frequent cases of allergic contact dermatitis produced by tattoos made with henna adulterated with PPD.
The most frequent presentation of sensitisation to PPD is contact allergic dermatitis (CAD),8–10 usually manifesting with erythema, vesicles and blisters at the site of henna application (Fig. 1). In some cases, it can lead to very severe or even fatal systemic allergic reactions.11–13
Many cases of sensitisation to PPD have been reported2,9,10,14,15; however, it would be useful to conduct a cross-sectional study to determine the prevalence of sensitisation to PPD in the paediatric population, and to establish its association with black henna tattoos.
Materials and methodsThe aim of this study was to determine the prevalence of sensitisation to PPD in the population of paediatric patients referred to a skin allergy clinic, its epidemiological characteristics, and its association with black henna tattoos.
We collected data on all patients aged 0–16 years referred to the skin allergy clinic of the Hospital General Universitario de Valencia between 1980 and 2015 in an electronic database.
All referred patients underwent a structured history-taking and a basic physical examination, followed by patch testing.
The method used to perform patch tests was the one described in the recommendations of the Spanish Group on the Research of Contact Dermatitis and Skin Allergy (Grupo Español en Investigación de Dermatitis de Contacto y Alergia Cutánea [GEIDAC]).16
All patients received the standard series of patch tests recommended for adults by the GEIDAC, which includes PPD in the list of most frequent allergens.
The tests were first read 48h following the patch test and once more at 96h. The reactions were categorised based on clinical criteria into: negative reaction, 1+ (erythema), 2+ (papular erythema), 3+ (vesicle formation) and 4+ (blister formation). For the purpose of our analysis, we defined a positive reaction as a reaction of 2+ or above.
For positive cases, we established the clinical relevance of sensitisation as current (based on the current presenting complaint), past (potential association with a past skin reaction) or unknown (with no apparent association with the presenting complaint).
In cases of current clinical relevance, we documented the most likely source of sensitisation.
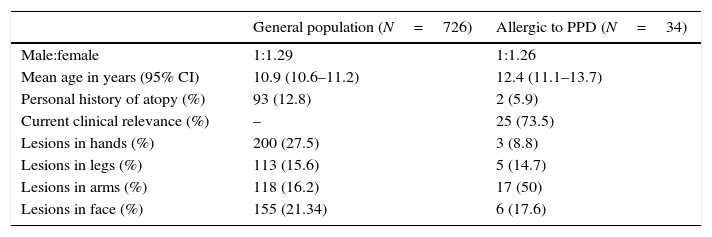
ResultsTable 1 summarises the main findings of the study.
Main findings of the study.
| General population (N=726) | Allergic to PPD (N=34) | |
|---|---|---|
| Male:female | 1:1.29 | 1:1.26 |
| Mean age in years (95% CI) | 10.9 (10.6–11.2) | 12.4 (11.1–13.7) |
| Personal history of atopy (%) | 93 (12.8) | 2 (5.9) |
| Current clinical relevance (%) | – | 25 (73.5) |
| Lesions in hands (%) | 200 (27.5) | 3 (8.8) |
| Lesions in legs (%) | 113 (15.6) | 5 (14.7) |
| Lesions in arms (%) | 118 (16.2) | 17 (50) |
| Lesions in face (%) | 155 (21.34) | 6 (17.6) |
We studied a total of 726 children aged 0–16 years referred to the skin allergy clinic between 1980 and 2015, of who 361 (49.7%) were sensitised to at least one allergen. The mean age of the patients under study was 10.9 years. Fifty-six percent of the patients were male and 44% female. Ninety-three patients (12.8%) had a personal history of atopy.
All of the patients in the study underwent a PPD patch test, and 34 were found to be sensitised (4.68% of referred children and 9.41% of children sensitised to at least one allergen).
The mean age of the children allergic to PPD was 12.4 years. Of all patients with PPD allergy, 44.2% were male and 55.8% female. Two patients (5.9%) had a personal history of atopy.
Of the 34 positive reactions to PPD, 25 (73.5%) were considered to be relevant to the current clinical concern. The most frequent sites of reaction to PPD were the arms (32%) and abdomen (13%).
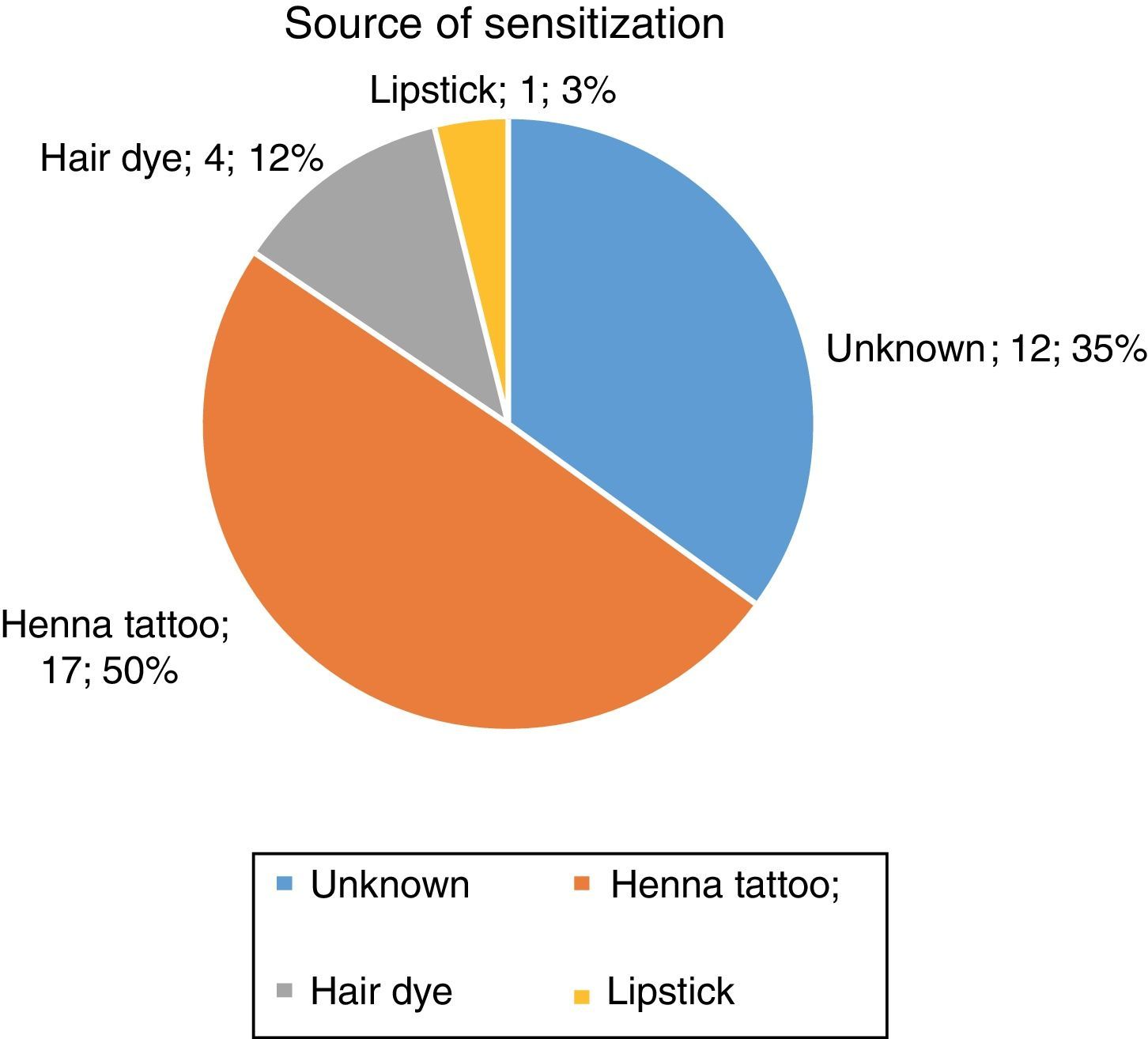
The documented source of sensitisation was a henna tattoo in 17 patients (50%), hair dye in four patients (11.7%), lipstick in one patient (2.9%) and unknown in 12 patients (35.2%) (Fig. 2).
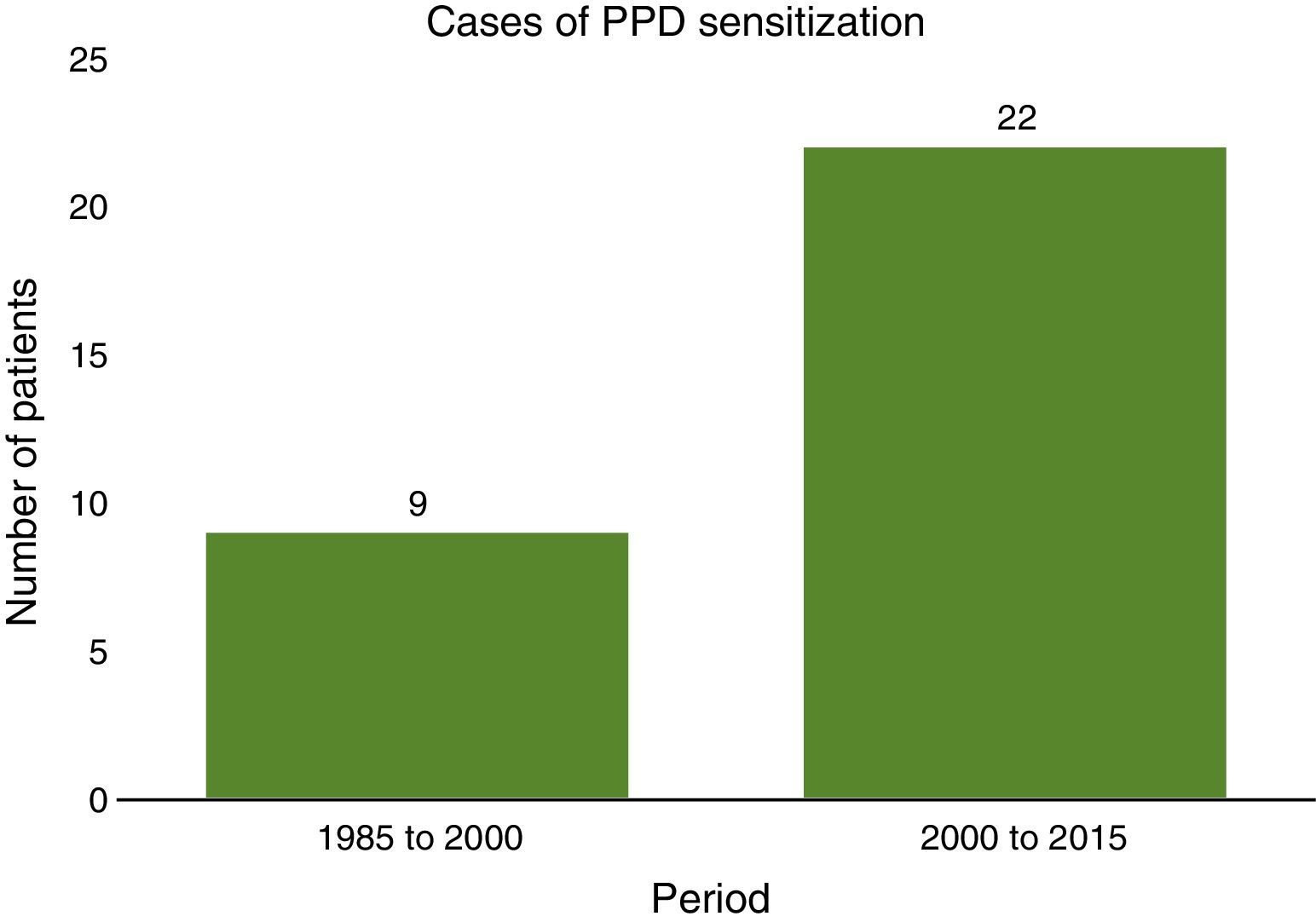
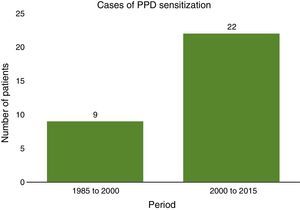
While the duration of both periods was the same, nine cases of allergy to PPD were identified between 1985 and 2000, compared to 22 between 2000 and 2015 (Fig. 3).
DiscussionPara-phenylenediamine is a potent allergen that may cause reactions ranging from local allergic responses to systemic involvement and risk of death.11–13 Skin lesions are usually eczematous, but reactions may also be lichenoid or resemble erythema multiforme.
The current legislation of the European Economic Community on the composition of cosmetic products specifies that PPD cannot be used in the skin, eyebrows or lashes under any circumstances. In hair products, it cannot exceed a concentration of 6%.7 The inclusion of hydrogen peroxide in hair dyes accelerates the oxidation of PPD, which decreases its reactogenicity. However, PPD is a common component in temporary henna tattoos,4,5 causing a significant number of allergic reactions.6,17 It does not undergo oxidation in tattoos, and thus has a high potential for producing an allergic reaction.
In our study, we found a high prevalence of ACD caused by PPD, as it occurred in approximately one out of every twenty children referred to the skin allergy clinic. Para-phenylenediamine is one of the most common allergens involved in children with ACD, and produces reactions in nearly one out of ten children that are sensitised to at least one allergen.18
Most of the positive reactions to PPD were considered to have current clinical significance, suggesting that allergy to PPD frequently leads to clinically significant ACD. The source of sensitisation in half of the cases was henna tattoos, which are the main source of allergic reactions to PPD in the paediatric population. The second most common source was hair dyes, as PPD is frequently found in these products.
The prevalence of sensitisation to PPD was similar in male and female patients, and much higher in older patients. This finding fits with the use of henna in tattoos, which adolescents get much more frequently. Similarly, the frequent localisation of the reaction in the arms or abdomen is also consistent with the choice of these sites for tattoos.
Despite the ban of the use of PPD in topical products, the prevalence of sensitisation to PPD has doubled in the past 10 years, which calls for a campaign to raise public awareness of the risks of PPD and of tattoos made with adulterated henna.
The concentrations of PPD in black henna reported in the literature range between 0.4% and 29.5%,4,5 and in most cases they were much higher than the concentrations found in hair dyes. This makes black henna a substance with a high potential for reactogenicity.
Atopic contact dermatitis secondary to exposure to PPD usually has a favourable prognosis. However, the allergic reactions it produces can sometimes be very serious, threatening the life of the patient.11–13 The literature also includes descriptions of allergic reactions to PPD resulting in necrotic lesions and unsightly scars (Fig. 4), post-inflammatory hypopigmentation and keloid formation.11 In patients sensitised to PPD from a tattoo, the use of hair colouring products can produce very serious allergic reactions for a lifetime due to the usual presence of PPD in these substances.19 It is a frequent occurrence, and patients must be warned of this risk.
ConclusionSensitisation to PPD is fairly common in the paediatric population. The most frequent source of sensitisation to this substance are temporary tattoos made with henna adulterated with PPD. The inclusion of PPD in any product applied topically to the skin is banned due to the high risk of sensitisation. The general population should be made aware of the risks associated with getting tattoos made with adulterated henna, and temporary tattoos should be discouraged in the paediatric population given the high risk of severe allergic reactions that could lead to death or future sequelae.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Ortiz Salvador JM, Esteve Martínez A, Subiabre Ferrer D, Victoria Martínez AM, de la Cuadra Oyanguren J, Zaragoza Ninet V. Dermatitis alérgica de contacto a parafenilendiamina por tatuajes con henna en población pediátrica. An Pediatr (Barc). 2017;86:122–126.