Pre-term delivery is one of the leading causes of foetal and perinatal mortality. However, perinatal risk factors associated with intra-partum foetal death in preterm deliveries have not been well studied.
ObjectiveTo analyse foetal mortality and perinatal risk factors associated with intra-partum foetal mortality in pregnancies of less than 32 weeks gestational age.
Material and methodsThe study included all preterm deliveries between 22 and 31 +1 weeks gestational age (WGA), born in a tertiary-referral hospital, over a period of 7 years (2008–2014). A logistic regression model was used to identify perinatal risk factors associated with intra-partum foetal mortality (foetal malformations and chromosomal abnormalities were excluded).
ResultsDuring the study period, the overall foetal mortality was 63.1% (106/168) (≥22 weeks of gestation) and occurred in pregnancies of less than 32 WGA. A total of 882 deliveries between 22 and 31+6 weeks of gestation were included for analysis. The rate of foetal mortality was 11.3% (100/882). The rate of intra-partum foetal death was 2.6% (23/882), with 78.2% (18/23) of these cases occurring in hospitalised pregnancies. It was found that Assisted Reproductive Techniques, abnormal foetal ultrasound, no administration of antenatal steroids, lower gestational age, and small for gestational age, were independent risk factors associated with intra-partum foetal mortality.
ConclusionThis study showed that there is a significant percentage intra-partum foetal mortality in infants between 22 and 31+6 WGA. The analysis of intrapartum mortality and risk factors associated with this mortality is of clinical and epidemiological interest to optimise perinatal care and improve survival of preterm infants.
El parto prematuro es una de las principales causas de mortalidad perinatal y fetal. Sin embargo, los factores de riesgo perinatales asociados a mortalidad fetal intraparto en partos pretérmino no han sido bien analizados.
ObjetivoAnalizar la mortalidad fetal y los factores de riesgo perinatales asociados a mortalidad fetal intraparto en gestaciones de menos de 32 semanas.
Material y métodosSe incluyeron en el análisis todos los partos pretérmino entre las semanas 22 y 31+6 días, nacidos en un hospital terciario durante un periodo de 7 años (2008-2014). Se realizó un análisis de regresión logística para identificar factores de riesgo perinatales asociados a mortalidad fetal intraparto (excluidos malformaciones y cromosomopatías severas).
ResultadosEn este período el 63,1% (106/168) de la mortalidad fetal (≥22 semanas) se produjo en gestaciones menores de 32 semanas. Ochocientos ochenta y dos nacimientos entre las semanas 22 y 31+6 días fueron incluidos en el análisis. La mortalidad fetal fue del 11,3% (100/882). La mortalidad fetal intraparto fue del 2,6% (23/882), afectando en el 78,2% de los casos (18/23) a gestantes hospitalizadas. Encontramos que las técnicas de reproducción asistida, la ecografía fetal patológica, la no administración de corticoides antenatales, la menor edad gestacional y el bajo peso para la edad gestacional fueron factores de riesgo independientes asociados a mortalidad fetal intraparto.
ConclusiónLa mortalidad fetal intraparto afectó a un porcentaje importante de nacimientos entre las semanas 22 y 31+6 días. El análisis de la mortalidad fetal intraparto y los factores de riesgo asociados a esta resulta de gran interés clínico y epidemiológico para optimizar el cuidado perinatal y aumentar la supervivencia del recién nacido pretérmino.
Foetal mortality is a key indicator of perinatal care, and it accounts to up to 50% of perinatal mortality in countries such as the United States.1 Preterm birth is one of the of the factors most strongly associated with foetal mortality, so that its analysis is recommended in preterm newborn studies.2,3 National registers do not always analyse this mortality, and comparisons between countries are hindered not only by differences in perinatal management practices, but also in the gestational ages included in the analysis.4,5 This may lead to the underestimation of foetal mortality, especially inpregnancies at the limit of viability.6
The foetal mortality rate in developed countries is estimated at five to six per 1000 births,7 and based on data from large-scale registers worldwide, the antepartum foetal mortality rate in the developed world is 5.2 per 1000 births and the intrapartum foetal mortality rate is 0.9 per 1000 births. In recent years there has been a decrease in intrapartum mortality, which may be due to more intensive antenatal care, improved monitoring during labour and an increased caesarean delivery rate.4,8 Numerous studies have analysed potential causes of foetal death in developed countries.9 Foetal death seems to be a multifactorial phenomenon that is sometimes difficult to explain and with multiple aetiologies.7 Several studies demonstrate that the risk factors associated with foetal death vary by gestational age and the timing of death, that is, whether it occurred before or during delivery.7,10–15 Since in developed countries intrapartum foetal death in preterm deliveries usually takes place in hospital settings, the detection of potential risk factors associated with it is of particular clinical relevance. However, we did not find any studies that specifically addressed perinatal factors that could potentially increase the risk of intrapartum foetal death in preterm births.
The aim of this study was to analyse foetal mortality between 22 and 31+6 weeks’ gestation and to identify potential perinatal risk factors associated with intrapartum foetal death.
Population and methodsPopulationWe conducted a study of pregnant women that gave birth preterm between 22 and 31+6 weeks’ gestation at the Hospital General Universitario Gregorio Marañón de Madrid (level IIIc referral hospital for high-risk pregnancies and congenital neonatal diseases).
MethodsWe conducted a retrospective observational study over a period of seven years (January 2008 to December 2014). We collected the data recorded in the SEN 1.500 morbidity and mortality register prospectively. We collected data for the factors under study that are not recorded in this register prospectively between 2012 and 2014 and retrospectively for the 2008–2011 period. The study was approved by the Ethics and Clinical Research Committee of the Hospital General Universitario Gregorio Marañón.
We applied the definitions of foetal death proposed by the WHO16: foetal death as death prior to the complete expulsion or extraction from its mother of a product of conception, irrespective of the duration of pregnancy, with no evidence of life (absence of breathing, heart beat, umbilical cord pulsation or movement of voluntary muscles); antepartum foetal death occurring prior to the onset of labour, and intrapartum foetal death as one in which the foetus was alive at the onset of labour. We completed the definition of intrapartum foetal death as absence of signs of life at minutes 1, 5 and 10 from birth (Apgar 0/0/0).
We analysed the foetal mortality rate at 22 or fewer weeks’ gestation and between 23 and 31+6 weeks’ gestation (number of foetal deaths per 1000 births). Our centre is a level IIIc hospital that does not perform legal voluntary terminations of pregnancy, so cases of severe chromosomal disorders or malformations were included in the calculation of this rate.
To analyse the cumulative incidence of foetal mortality between 23 and 31+6 weeks’ gestation (number of foetuses that died during this period compared to the total births in the same weeks of gestation) and the perinatal risk factors associated with intrapartum foetal death, we excluded cases with congenital anomalies and/or chromosomal disorders associated with poor survival rates (due to the increased risk of intrauterine death).
The perinatal factors analysed in our study were: maternal age, prenatal care (from the beginning of pregnancy, that is, the full programme); disease preceding or during pregnancy, including preeclampsia, gestational diabetes, antepartum haemorrhage, unfavourable obstetric history (>2 previous miscarriages or cervical incompetence requiring cervical cerclage in the current pregnancy) and chronic disease (hypertension, diabetes mellitus type1, obesity, substance use, renal, hepatic, cardiovascular or autoimmune disease, or cancer); assisted reproductive technology (ART); multiple pregnancy; abnormal foetal ultrasound (intrauterine growth restriction [IUGR], abnormal Doppler, oligohydramniosorpolyhydramnios)17,18; premature rupture of membranes and latency period in hours; antenatal administration of antibiotics; suspicion of chorioamnionitis19; antenatal administration of corticosteroids (number of doses and timing of administration relative to delivery); mode of delivery (vaginal or caesarean); gestational age (calculated on the basis of foetal ultrasound in the first trimester and date of last menstrual period, and in cases with no prenatal care, based on the physical examination of the newborn); birth weight, small for gestational age (birth weight<10th percentile)20 and sex.
Statistical analysisWe present the results of continuous variables as mean and standard deviation, and categorical variables as absolute frequencies and percentages. We have expressed quantitative variables that did not follow a normal distribution as median and interquartile range (25th–75th percentile).
To compare the means of two groups, we used a parametric test (Student's t test) or nonparametric test (Mann–Whitney U test) as appropriate.
We studied the association of mortality with qualitative variables by means of the chi square test or Fisher's exact test, and the association between quantitative variables by means of Pearson's correlation coefficient or Spearman's rho. We conducted a multivariate logistic regression analysis to identify potential factors associated with intrapartum death with a 95% confidence interval (CI). The statistical analysis was performed using SPSS® version 21.0 and EPIDAT 3.1. Results with a p-value of less than 0.05 were considered statistically significant.
ResultsFoetal mortality (Tables 1 and 2)The mean foetal mortality rate at 22 to 31+6 weeks’ gestation was 2.3‰ (1.1–3.1‰). During this period, 63.1% (106/168) of foetal deaths took place in gestations of less than 32 weeks. (Tables 1 and 2).
Foetal mortality in births at 22 or fewer weeks’ gestation and between 22 and 31+6 weeks’ gestation (without taking into account the exclusion criteria).
| Year | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | Total |
|---|---|---|---|---|---|---|---|---|
| Total births, n | 8177 | 6375 | 7707 | 6245 | 5479 | 5416 | 5365 | 44,764 |
| Foetal deaths at ≥22 weeks, n | 29 | 30 | 22 | 24 | 22 | 22 | 19 | 168 |
| Foetal deaths at 22–31+6 weeks, n (%) | 24 (82.7) | 20 (66.6) | 15 (68.2) | 17 (70.8) | 14 (63.6) | 7 (35.3) | 9 (47.3) | 106 (63.1) |
| Foetal mortality ratea at ≥22weeks | 3.5‰ | 4.7‰ | 2.8‰ | 3.8‰ | 4‰ | 3.1‰ | 3.5‰ | 3.7‰ |
| Foetal mortality rate at 22–31+6 weeks | 2.9‰ | 3.1‰ | 1.9‰ | 2.7‰ | 2.5‰ | 1.1‰ | 1.6‰ | 2.3‰ |
n, total number of cases per year; (%): percentage of foetal deaths in gestations of 22 or fewer weeks.
Foetal mortality (antepartum and intrapartum) and live births by gestational age.
| Gestational age (weeks) | 22 w n (%) (95% CI) | 23 w n (%) (95% CI) | 24 w n (%) (95% CI) | 25 w n (%) (95% CI) | 26 w n (%) (95% CI) | 27 w n (%) (95% CI) | 28 w n (%) (95% CI) | 29 w n (%) (95% CI) | 30 w n (%) (95% CI) | 31 w n (%) (95% CI) | Total n (%) (95% CI) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Total births | 8 | 36 | 61 | 88 | 74 | 98 | 117 | 107 | 130 | 163 | 882 |
| Foetal deaths | 5 (62.5) (24.5–91.5) | 10 (27.7) (11.8–43.8) | 12 (19.6) (8.9–30.5) | 11 (12.5) (5–20) | 9 (12.1) (4–20.3) | 12 (12.2) (5.2–19.2) | 13 (11.1) (5–17.2) | 7 (6.5) (1.4–11.7) | 8 (6.1) (1.6–10.7) | 13 (8) (3.5–12.4) | 100 (11.3) (9.2–13.8) |
| Antepartum foetal deaths | 2 (25) (3.2–65.1) | 6 (16.6) (3.1–30.2) | 3 (4.9) (1–13.7) | 9 (10.2) (3.3–17.1) | 9 (12.1) (4–20.3) | 10 (10.2) (3.7–16.7) | 13 (11.1) (5–17.2) | 6 (5.6) (0.8–10.4) | 7 (5.4) (1.1–9.6) | 12 (7.4) (3–11.7) | 77 (8.7) (6.8–10.6) |
| Intrapartum foetal deaths | 3 (37.5) (8.5–75.5) | 4 (11.1) (3.1–26.1) | 9 (14.7) (5–24.5) | 2 (2.2) (0.3–8) | 0 (0) (0–4.9) | 2 (2) (0.2–7.2) | 0 (0) (0–3.1) | 1 (0.9) (0.1–5.1) | 1 (0.7) (0.02–4.2) | 1 (0.6) (0.02–3.4) | 23 (2.6) (1.5–3.7) |
| Hospitalised mothersa | 3 | 3 | 7 | 1 | 0 | 2 | 0 | 1 | 1 | 0 | 18 |
| Live births | 3 (37.5) (8.5–75.5) | 26 (72.2) (56.2–88.2) | 49 (80.3) (69.5–91) | 77 (87.5) (80.5–95) | 65 (87.8) (79.7–96) | 86 (87.7) (80.7–94.7) | 104 (88.8) (82.8–95) | 100 (93.4) (88.3–98.6) | 122 (93.9) (89.3–98.4) | 150 (92) (87.6–96.5) | 782 (88.7) (86.5–90.8) |
CI, confidence interval; n, total number of cases per year; w, weeks; (%): percentage of foetal deaths and 95% confidence interval by gestational age.
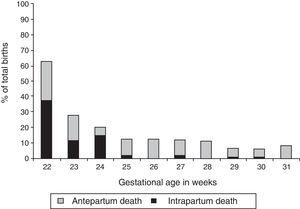
In gestations of 22 to 31+6 weeks, the cumulative incidence of foetal mortality (excluding six foetuses with malformations and/or chromosomal disorders) was 11.3% (100/882; 95%CI, 9.2–13.8), with considerable variation based on gestational age (62.5% at 22 weeks’ gestation, compared to <10% at 29 or more weeks’ gestation). Intrapartum foetal death amounted to 2.6% of the total births (23/882; 95% CI, 1.5–3.7) and 23% of foetal deaths (23/100). Intrapartum foetal mortality was higher in gestations of less than 25 weeks, and reached 37.5% (3/8), 11.1% (4/36) and 14.7% (9/61) of the total births at 22, 23 and 24 weeks’ gestation (Fig. 1). Of all intrapartum deaths, 78.2% (18/23) occurred in women that were already hospitalised (minimum of 9h and maximum of 15 days).
Resuscitation efforts were made at birth in 11 of the 23 patients that died during delivery (in five, advanced resuscitation was performed with chest compressions with or without epinephrine administration).
Risk factors associated with intrapartum foetal death (Tables 3 and 4)Table 3 shows the perinatal factors under study, comparing the preterm live birth group with the intrapartum death group. We found statistically significant differences in the use of assisted reproductive technology (20.8% vs 41.6%; P=0.01), abnormal foetal ultrasound findings (32.7% vs 65.2%; P=0.001;with a greater percentage of abnormal Doppler findings and oligohydramnios in the preterm intrapartum death group), administration of antenatal corticosteroids (91.1% vs 34.7%; P<0.001), indication of caesarean delivery (62.7% vs 30.4%; P=0.002), gestational age (weeks’ gestation, 28+5 vs 24+4; P<0.001), birth weight (1100g vs 650g; P<0.001) and small for gestational age (8.8% vs 26%; P=0.005) (Tables 3 and 4).
Comparison of the perinatal risk factors under study between live births and intrapartum foetal deaths at fewer than 32 weeks’ gestation.
| Prenatal variables under study | Live births | Intrapartum foetal deaths | P |
|---|---|---|---|
| Total births, n | 782 | 23 | |
| Maternal age in years, mean±SDa | 32.1±6.5 | 33.5±5.9 | 0.24 |
| Prenatal care, n (%) | 749 (95.7) | 23 (100) | 0.092 |
| Maternal disease during gestationc, n (%) | 317 (41) | 12 (52.1) | 0.30 |
| Preeclampsia | 113 (14.6) | 4 (17.4) | 0.70 |
| Gestational diabetes | 59 (7.7) | 1 (4.3) | 0.55 |
| Obstetric haemorrhage | 69 (9) | 4 (17.4) | 0.06 |
| Unfavourable obstetric history | 97 (12.5) | 3 (13) | 0.94 |
| Chronic disease | 78 (10.1) | 5 (21.7) | 0.07 |
| Assisted reproductive technology (ART), n (%) | 163 (20.8) | 10 (41.6) | 0.01* |
| Multiple pregnancy, n (%) | 296 (37.8) | 11 (47.8) | 0.33 |
| Abnormal foetal ultrasoundc, n (%) | 254 (32.7) | 15 (65.2) | 0.001* |
| IUGR with normal Doppler | 39 (5) | 2 (8.7) | 0.75 |
| IUGR with abnormal Dopplerd | 77 (9.9) | 4 (17.4) | 0.4 |
| Abnormal Doppler d | 25 (3.2) | 4 (17.4) | 0.04* |
| Oligohydramnios | 140 (18.3) | 10 (43.4) | 0.002* |
| Polyhydramnios | 10 (1.3) | 1 (4.3) | 0.60 |
| Caesarean delivery, n (%) | 491 (62.7) | 7 (30.4) | 0.002* |
| ROM latency>1h, n (%) | 285 (36.4) | 11 (47.8) | 0.26 |
| ROM latency, median (Q1–Q3)b | 72 (13–220) | 144 (12–270) | 0.47 |
| Maternal antibiotherapy, n (%) | 464 (59.3) | 15 (65.2) | 0.57 |
| Suspectedchorioamnionitis, n (%) | 192 (24.5) | 9 (39.1) | 0.11 |
| Antenatal corticosteroids (at least one dose), n (%) | 713 (91.1) | 8 (34.7) | <0.001* |
| Full course | 393 (50.3) | 5 (21.7) | 0.011* |
| Partial course (one dose) | 160 (20.4) | 1 (4.3) | 0.10 |
| Corticosteroids>7 days | 160 (20.4) | 2 (8.6) | 0.21 |
| No dose | 69 (8.9) | 15 (65.2) | <0.001* |
| Gestational age (weeks+days), median (Q1–Q3) | 28+5 (26+3; 30+3) | 24+4 (24; 27) | <0.001* |
| Birth weight (g), mean±SD | 1100±379g | 650±210g | <0.001* |
| Small for gestational age, n (%) | 69 (8.8) | 6 (26) | 0.005* |
| Male sex, n (%) | 416 (53.2) | 13 (56.5) | 0.75 |
IUGR, intrauterine growth restriction; n, total number of patients in each group; ROM, rupture of membranes; (%), percentage of the total of live births or intrapartum foetal deaths, by column.
Cases in which the value of the analysed factor was unknown in the column of live births. Percentage based on the denominator adjusted for these missing data: maternal disease during pregnancy (10 cases), gestational diabetes (16 cases), preeclampsia (10 cases), and abnormal foetal ultrasound (6 cases).
Independent risk factors associated with intrapartum foetal death between 22 and 31+6 weeks’ gestation (multivariate analysis).
| Perinatal risk factors | P | OR | 95% CI |
|---|---|---|---|
| Assisted reproductive technologies | 0.048* | 2.6 | (1.02–7.55) |
| Abnormal foetal echocardiogram | 0.005* | 4.8 | (1.6–15.1) |
| No antenatal corticosteroids | <0.001* | 8.27 | (2.52–27.15) |
| Caesarean delivery | 0.55 | 0.7 | (0.21–2.3) |
| 22–25 weeks’ gestationa | 0.026* | 5.37 | (1.21–23.7) |
| 26–28 weeks’ gestationa | 0.98 | 0.98 | (0.16–6.11) |
| Small for gestational age | 0.042* | 3.67 | (1.05–12.9) |
The multivariate analysis showed that the use of assisted reproductive technology (OR, 2.6; 95% CI, 1.02–7.55), abnormal foetal ultrasound findings (OR, 4.8; 95% CI, 1.6–15.1), lack of administration of antenatal corticosteroids (OR, 8.27; 95% CI, 2.52–27.15), low gestational age (22–25 weeks’ gestation; OR, 5.37; 95% CI, 1.21–23.7) and low birth weight (OR, 3.67; 95% CI, 1.05–12.9) were independent risk factors associated with intrapartum foetal death.
DiscussionTo our knowledge, this is the first study that analyses the risk factors specifically associated with intrapartum foetal death in gestations of less than 32 weeks.
Foetal mortality is a key indicator in perinatal care, and it remains high even today.21 In our hospital, the cumulative foetal mortality rate in gestations of less than 32 weeks during the period under study was of 2.3‰. Out of all cases of foetal death, 63.1% took place between 22 and 31+6 weeks’ gestation, with a mortality rate of 11.3% and a rate of intrapartum foetal death of 2.6%. These percentages are similar to others reported in the literature, although there is significant variability in the reported rates, as evinced by the MOSAIC study (foetal mortality ranging between 12.8% and 22.3% and intrapartum mortality between 1.2% and 4.8%).5 But large-scale national studies on the survival of preterm newborns do not always analyse this particular rate.22,23 In Spain, a study published recently analysed the mortality of preterm newborns of 23 to 26 weeks of gestational age,24 but did not include foetal mortality. However, foetal mortality reaches the highest percentages precisely in this group of the most premature,5,15,25 which in our review was as high as 16.2%.
Various factors may hinder the analysis of foetal mortality, including the variability in the gestational age starting from which cases are reported to registers9,26 or the occasional difficulty of differentiating between antepartum and intrapartum foetal death.27 Although intrapartum foetal mortality has decreased in recent years, it still represents a significant percentage of the total births,5,25,28 and amounted to 2.6% of the total in our study, with a significantly increased percentage in preterm births before 25 weeks’ gestation (15.2%). Another salient finding of our analysis was that 78.2% of intrapartum deaths (18/23) occurred in mothers that were already hospitalised, and the relevance of this finding may be twofold. First, these cases can be monitored more closely before and during labour; and second, parents may be given information before delivery that would usually include a prediction of survival, which should be estimated as soon as there is a risk of preterm birth, and not only when the baby is born alive. For all the above reasons, intrapartum foetal mortality and the associated risk factors are of considerable clinical and epidemiological relevance.
Numerous authors have analysed maternal and obstetric risk factors associated with foetal mortality.7,29,30 Some studies have found differences in the risk factors associated with foetal mortality in term versus preterm deliveries.10,31 This is also the case with antepartum versus intrapartum foetal mortality, for while they may have similar causes, intrapartum foetal mortality is closely associated with obstetric practices and intrauterine hypoxia.12,17,28 However, we did not find any studies that specifically analysed the potential perinatal risk factors associated with intrapartum foetal death in preterm deliveries.
Some of the risk factors associated to intrapartum foetal mortality are advanced maternal age, multiple pregnancy, lack of prenatal care, premature rupture of membranes or chronic diseases such as obesity.12–14 Other risk factors associated with foetal mortality in preterm deliveries are placental abruption, preeclampsia or intrauterine infection.7,10,11 In our study, we did not find a significant difference in these risk factors, and while we found a greater percentage of obstetric haemorrhage, chronic maternal disease and chorioamnionitis, these differences were not statistically significant. We did find statistically significant associations with TRA, abnormal foetal ultrasound findings (abnormal Doppler and oligohydramnios), lower percentage of caesarean deliveries, lower administration of antenatal corticosteroids, lower gestational age and low birth weight. Although performance of caesarean delivery has been associated with a decreased foetal mortality rate,6,32 our multivariate analysis did not find it to be an independent risk factor for intrapartum foetal death. Lower gestational age,15,21 small for gestational age birth12 and abnormal foetal ultrasound findings are well-known and thoroughly studied risk factors. An abnormal foetal Doppler ultrasound is a predictor of foetal compromise and perinatal mortality, especially in high-risk pregnancies such as those with placental insufficiency or IUGR.30,31,33,34 Both oligohydramnios or polyhydramnios are abnormal and potentially place the foetus at risk, but their impact on foetal mortality remains unclear.33 However, a recent systematic review suggests that oligohydramnios is associated with increased perinatal mortality.35
Assisted reproductive technologies are usually associated with advanced maternal age, maternal chronic disease or multiple pregnancy, all of them factors that increase the risk of foetal death. A recent study found that singleton pregnancies achieved through ART carried a higher risk of foetal mortality at 22–27 weeks’ gestation.36 However, we did not find any studies that specifically assessed the association between ART and intrapartum mortality. A lack of antenatal corticosteroid treatment in preterm newborns is associated with an increased postnatal mortality and worse short-term and long-term outcomes.37,38 But we also found no studies analysing the effect of antenatal corticosteroids on intrapartum foetal mortality, despite the clear association of a lack of exposure with increased foetal mortality. We believe that this is an important aspect, as of all the factors that we identified, this is the only one that can be modified.
One of the limitations of this study is that we did not analyse the risk factors for antenatal foetal death, which may require specific study in this group of patients. Another limitation is that this was a retrospective hospital-based single-centre study conducted in a facility that manages a high percentage of high-risk pregnancies where the number of foetuses that die during delivery is small. Thus, it would be interesting to conduct broader studies to clarify whether these risk factors have a direct effect on intrapartum mortality or rather reflect a less invasive approach in more premature foetuses with poorer prognoses, as clinical decisions influenced by foetal prognosis may have the most significant impact on the survival of these patients.39
ConclusionIntrapartum foetal death occurs in a significant number of preterm births. Its study is of great clinical relevance, first, because estimations of survival for preterm newborns should start being made from the moment that there is risk of preterm birth; and secondly, because analysing the factors potentially associated with it may help optimise perinatal care and thus increase the survival of babies born preterm.
Conflict of interestsThe authors have no conflict of interests to declare.
Previous presentation: This study was presented as Risk factors associated with intrapartum stillbirths in preterm babies at the 4th International Congress of UENPS; December 11–14; Athens, Greece.
Please cite this article as: Zeballos Sarrato S, Villar Castro S, Ramos Navarro C, Zeballos Sarrato G, Sánchez Luna M. Factores de riesgo asociados a mortalidad fetal intraparto en recién nacidos pretérmino. An Pediatr (Barc). 2017;86:127–134.