In Portugal, data on the role of Der p 1 and Der p 2 in patients with house dust mite (HDM) allergy are scarce. Allergen-specific immunotherapy (sIT) is the only treatment that improves symptoms, reduces the need for pharmacological therapy and modifies the natural history of the disease. With this study, the authors aim to understand the local epidemiology and to clarify if the molecular assay of major allergens is advantageous in deciding and/or modifying the decision to initiate sIT in children with clinical indication which are sensitized to Dermatophagoides pteronyssinus.
MethodsRetrospective study with analysis of patients with asthma and/or rhinitis. Study period: January/2013–December/2016. Inclusion criteria: 1) positive prick-test to D. pteronyssinus; and 2) clinically relevant disease under treatment. Assay Der p 1 and Der p 2 values ≥0.35kUA/L were considered positive. Statistical significance was set at p<0.05.
ResultsThe clinical files of 279 patients. Mean ages 9.55 years (min. 4–max. 17). Asthma was present in 199 children (71.3%) and rhinitis in 245 (87.8%). Der p 1 and Der p 2 was <0.35kUA/L in 29 (10.4%) patients. The value of Der p 1/Der p 2 correlated with the size of the prick-test papule, the value of the eosinophils and the total IgE.
ConclusionsDer p 1 and Der p 2 are dominant allergens in our population and there may be benefits in determining these molecular allergen levels in patients with a positive prick-test and a clinical indication for sIT prior to a decision of initiating sIT or not.
En Portugal los datos del papel de Der p 1 y Der p 2 en niños con alergia al ácaro del polvo son escasos. La inmunoterapia específica (IE) con alérgenos es el único tratamiento que mejora los síntomas, reduce la necesidad de terapia farmacológica y modifica la historia natural de la enfermedad. Con este trabajo, los autores estudian la epidemiología local y buscan aclarar si el análisis molecular de los alérgenos principales es una ventaja para decidir y/o modificar la decisión de iniciar IE en niños con indicación clínica y sensibilizados a Dermatophagoides pteronyssinus.
MétodosEstudio retrospectivo de los niños con asma y/o rinitis. Período de estudio: enero de 2013 a diciembre de 2016. Criterios de inclusión: 1) prick-test positivo a Dermatophagoides pteronyssinus; y 2) enfermedad clínicamente relevante bajo tratamiento. Los valores de Der p 1 y Der p 2≥0,35kUA/l fueron considerados positivos. La significación estadística se estableció en p<0,05.
ResultadosSe incluyeron en el estudio 279 pacientes. Edad media 9,55 años (min. 4-máx. 17). El asma estuvo presente en 199 niños (71,3%) y rinitis en 245 (87,8%). Der p 1 y Der p 2 fue<0,35kUA/l en 29 (10,4%) pacientes. Der p 1/Der p 2 se correlacionó con el tamaño de la pápula de prick-test, con el valor de los eosinófilos y la IgE total.
ConclusionesDer p 1 y Der p 2 son alérgenos dominantes en nuestra población y puede haber beneficios en la determinación de estos niveles de alérgenos moleculares en pacientes con un prick-test positivo e indicación clínica para IE.
The prevalence of allergic diseases has increased rapidly over the past few decades in developed countries.1,2 Asthma, rhinoconjunctivitis, and eczema were systematically evaluated in approximately 1.2 million children in 98 countries in the International Study of Asthma and Allergies in Childhood (ISAAC)3 and a Portuguese epidemiological study in adults revealed a prevalence of 16.8% of asthma and 33.6% of rhinitis in central Portugal.4 Inhalant allergens play a crucial role in the development of these diseases, with house dust mites (HDM) considered the most important allergen source worldwide.5,6 HDM, especially Dermatophagoides pteronyssinus, are considered an important source for allergen sensitization and are major risk factors for allergic respiratory diseases in genetically predisposed patients.7 These allergens are divided into groups according to their biochemical composition, homology, and molecular weight. Presently, 20 HDM allergens for D. pteronyssinus have been registered by the World Health Organization and International Union of Immunological Societies Allergen Nomenclature Sub-committee (http://allergen.org/), many of these represent digestive enzymes since HDM feces are the major source of allergen exposure.
Some studies report a dominant prevalence of IgE antibodies against group 1 (Der p 1) and group 2 (Der p 2) HDM allergens in Europe.8–11 In Portugal, data on the role of Der p 1 and Der p 2 are still scarce.
The group 1 (Der p 1, 25kDa cystein proteases) allergens are found in high concentrations in fecal pellets, while those of group 2 (Der p 2, 14kDa) are mostly located in components of the mite body.7,12 Der p 1 and Der p 2 are considered major allergens of D. pteronyssinus, as they are recognized in more than 80% of mite-sensitive patients.11,13
Allergen-specific immunotherapy (sIT) is an important weapon in the treatment of respiratory allergy in selected cases, and provided that the patient has a hypersensitivity reaction mediated by IgE. The procedure requires a gradual administration of increasing amounts of an allergen to which the patient is sensitive, allowing the modulation of the untoward immune response to that allergen and alleviating allergic symptoms. It is the only treatment that improves symptoms, reduces the requirement of pharmacological therapy and modifies the natural history of allergic disease.14–16 The therapeutic effect may be long-lasting and prevents the progression from mild to severe forms of allergic disease.16–18
Since currently marketed vaccines are standardized only for the Der p 1 and Der p 2 allergens, the authors aim to understand the local epidemiology and to clarify if the molecular assay of these two major allergens is advantageous in deciding and/or modifying the decision to initiate sIT in children sensitized to D. pteronyssinus and with clinical indication, similarly to what is described in the literature.
MethodsPatientsThe authors performed a retrospective study with analysis of the clinical files of patients referred to the outpatient Clinic of Pediatric Allergology of Centro Hospitalar de Trás-os-Montes e Alto Douro with asthma and/or rhinitis between January 1st, 2013 and December 31st, 2016.
All patients were evaluated by a physician, using a detailed questionnaire to establish the nature and severity of their clinical manifestations. The diagnosis of allergic rhinitis was based on the international guidelines19 and the diagnosis of asthma followed the Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA), defined by a history of recurrent dyspnea, wheezing and/or coughing episodes, and patients were tested for positive airway reversibility with bronchodilators.
Skin prick-test (SPT)Skin sensitivity to D. pteronyssinus was measured by SPT, according to standard procedure.20 Allergen extracts and control solutions were obtained from Leti (Barcelona, Spain. Sensitization to major inhalant allergens included mites (D. pteronyssinus, Dermatophagoides farinae, Lepidoglyphus destructor), grass pollen mix, weed pollen mix, olive, Parietaria judaica, Alternaria alternata, dog and cat dander. Histamine (10mg/ml) and saline solutions were used as positive and negative controls. SPT was performed on the volar side of the forearm. The parameter for the wheal reaction, measured after 15min, was the value of the longest diameter. A positive skin reaction was defined as a wheal size of 3mm after subtraction of the negative control, according to EAACI criteria.21 The results were also expressed in mm and referred to the value of the largest diameter of the papule.
Serological analysis“Eosinophilia” was considered to be present if eosinophils were ≥4% of the total white blood cells.22
Total IgE levels were measured by Electro-Chemiluminescence Immunoasay (Roche) and were expressed in international units per unit volume (IU/l) and considered to be high according to gender: >230IU/l for males and >170IU/l for females.23
D. pteronyssinus extract, Der p 1 and Der p 2 was measured by ImmunoCAP (ImmunoCAP-100 and 250®, Thermo Fisher Scientific), according to the manufacturer's instructions. Levels of sIgE were expressed in kUA/L, and a value ≥0.35kUA/L was considered positive. Assay results were categorized into 6 classes: low (≥0.35 to <0.70kUA/L), moderate (≥0.70 to <3.50kUA/L), high (≥3.50 to <17.50kUA/L), very high – class 1 (≥17.50 to <50.00kUA/L), very high – class 2 (≥50.00 to <100.00kUA/L), and very high – class 3 (≥100.00kUA/L).
Inclusion criteria were: 1) clinically relevant disease with perennial symptoms or present during most of the year, even under medication; and 2) a positive prick-test to D. pteronyssinus.
Statistical analysisStatistical analysis was performed using SPSS version 24.0 for Windows. Levels of sIgE were expressed as medians and 25%–75% interquartile ranges (IQRs). The normality of the variables age, wheal size in the skin prick-test, Der p 1, Der p 2, total IgE levels and eosinophils were assessed using the Kolmogorov–Smirnov test. Comparisons of the prevalence of sIgE reactivity were performed with the χ2 or Fisher exact tests. Between-group comparisons of numerical data were performed using the Mann–Whitney U-test. Correlation analyses of serological measurements were performed by calculating the Spearman correlation coefficient (rs). To estimate the predicting value of the wheal size in the skin prick-test, total IgE levels and eosinophils and positive Der p 1/Der p 2, we used a receiver-operator characteristics (ROC) analysis. The area under the curve (AUC) was estimated. For each biomarker, we estimated AUC and its 95% confidence interval. p values of less than 0.05 were considered significant.
ResultsThe clinical files of 279 patients were included in the study. One hundred eighty-one (64.9%) were males and 98 (35.1%) were females. Age varied between 4 and 17 years, with a mean age of 9.55 (Table 1). One hundred and ninety-nine children (71.3%) had asthma, 245 (87.8%) rhinitis and 165 (59.1%) of the total had asthma and rhinitis, simultaneously. Some of the children had other atopic clinic associated: conjunctivitis (42.7%), atopic eczema (17.2%) and food allergy (7.9%), with fish, seafood, egg and milk as main responsible foods. A family history of atopy was registered in 202 (72.4%) patients, 54 (19.4%) with a maternal and/or paternal history of asthma. A chi-square test of independence was performed to examine the relation between clinical files and family history of atopy, the relation between asthma (χ2 (1,N=279)=2.124, p=0.145) or rhinitis (χ2 (1,N=279)=3.572, p=0.059) and family history of atopy was non-significant. The test was also performed to examine the relation between clinical files and risk factors such as term and preterm gestation, type of delivery, exclusive breast milk, house features, humidity and contact with animals. The results had no relation with statistical significance (Table 2).
Clinical and demographic characterization of the sample.
| Patients, n | Mean age, years | Der p 1-positive, n (%) | Median (kUA/L) | Der p 2-positive, n (%) | Median (kUA/L) | |
|---|---|---|---|---|---|---|
| All patients | 279 | 9.55 (4–17) | 205 (73.5) | 22.0 | 213 (76.3) | 21.7 |
| Sex | ||||||
| Male | 181 | 9.45 | 133 (73.5) | 22.0 | 136 (75.1) | 22.4 |
| Female | 98 | 9.73 | 72 (73.5) | 26.3 | 77 (78.6) | 21.7 |
| Clinic | ||||||
| Asthma and rhinitis | 165 | 9.45 | 24 (14.6) | 24.4 | 130 (78.8) | 23.9 |
| Only asthma | 34 | 8.88 | 24 (70.6) | 21.0 | 26 (76.5) | 24.0 |
| Only rhinitis | 80 | 10.03 | 24 (30) | 17.9 | 57 (71.3) | 17.9 |
| Conjunctivitis | 119 | 10.45 | 24 (20.2) | 21.3 | 86 (72.3) | 22.4 |
| Eczema | 48 | 8.65 | 24 (50) | 20.6 | 41 (85.4) | 29.0 |
| Food allergy | 22 | 10.32 | 13 (59.1) | 18.9 | 15 (68.2) | 11.4 |
| Family history of allergy | ||||||
| Yes | 202 | 9.50 | 156 (77.2) | 23.0 | 157 (77.7) | 24.4 |
| No | 77 | 9.66 | 49 (63.6) | 19.8 | 56 (72.7) | 16.5 |
| Mother and/or father with asthma | 54 | 9.39 | 41 (75.9) | 31.0 | 47 (87) | 32.5 |
Risk factors for atopy.
| Patients, n | Mean age (years) | Der p 1-positive, n (%) | Median (kUA/L) | Der p 2-positive, n (%) | Median (kUA/L) | Asthma, n (%) | Rhinitis, n (%) | |
|---|---|---|---|---|---|---|---|---|
| Gestation | ||||||||
| Term gestational age | 72 | 10.01 | 48 (66.7) | 48.3 | 50 (69.4) | 37.5 | 52 (72.2) | 64 (88.9) |
| Preterm gestational age | 13 | 7.38 | 11 (84.6) | 14.3 | 13 (100) | 28.9 | 10 (76.9) | 11 (84.6) |
| Unknown | 194 | |||||||
| Delivery | ||||||||
| Cesarean | 85 | 9.38 | 69 (81.2) | 28.5 | 58 (68.2) | 27.6 | 58 (68.2) | 78 (91.8) |
| Vaginal | 117 | 8.93 | 83 (70.9) | 22 | 96 (82.1) | 22.8 | 84 (71.8) | 101 (86.3) |
| Unknown | 77 | |||||||
| Exclusive breast milk | ||||||||
| Yes | 117 | 9.25 | 89 (76.1) | 28.5 | 95 (81.2) | 28.9 | 90 (76.9) | 105 (89.7) |
| No | 22 | 10.05 | 17 (77.3) | 17.9 | 15 (68.2) | 14.8 | 15 (68.2) | 22 (100) |
| Unknown | 140 | |||||||
| Means of housing | ||||||||
| Rural area | 92 | 6.65 | 73 (79.3) | 28.5 | 70 (76.1) | 29.3 | 73 (78.3) | 82 (89.1) |
| Urban area | 59 | 9.66 | 41 (69.5) | 17 | 47 (79.7) | 18.5 | 40 (67.8) | 56 (94.9) |
| Unknown | 128 | |||||||
| Humidity | ||||||||
| Yes | 54 | 9.72 | 41 (75.9) | 23.9 | 45 (83.3) | 8.7 | 40 (74.1) | 49 (90.7) |
| No | 81 | 9.51 | 62 (76.5) | 27.3 | 61 (75.3) | 20 | 61 (75.3) | 74 (91.4) |
| Unknown | 144 | |||||||
| Contact with animals | ||||||||
| Yes | 107 | 9.80 | 83 (77.6) | 28.5 | 86 (80.4) | 28.6 | 80 (74.8) | 97 (90.7) |
| No | 30 | 9.07 | 22 (73.3) | 23.3 | 22 (73.3) | 24.8 | 23 (76.3) | 28 (93.3) |
| Unknown | 142 | |||||||
Eosinophils ≥4% was present in 144 children and 158 had increased total IgE values for age. The positive values for Der p 1 and Der p 2 are shown in Table 3.
Der p 1 and Der p 2 serum levels according to eosinophils levels, total IgE levels and wheal size.
| Patients, n (%) | Mean age (years) | Median (kUA/L) | Der p 1 positive, n (%) | Median (kUA/L) | Der p 2 positive, n (%) | Median (kUA/L) | |
|---|---|---|---|---|---|---|---|
| Eosinophilia (%) | |||||||
| Eosinophils≥4% | 144 (63.7) | 9.5 | 7.2% (±4.1) | 108 (75) | 16.2 | 44 (30.6) | 21.5 |
| Eosinophils<4% | 82 (36.3) | 9.7 | 2.6% (±1.1) | 53 (64.6) | 1.8 | 52 (63.4) | 1.4 |
| unknown | 53 | ||||||
| Total IgE values (UI/mL) | |||||||
| Increased values | 158 (66.4) | 9.7 | 624 UI/mL (±837) | 119 (75.3) | 19.4 | 127 (80.4) | 28.6 |
| Normal values | 80 (33.6) | 8.9 | 102 UI/mL (±66) | 53 (66.3) | 4.7 | 59 (73.8) | 6.6 |
| Unknown | 41 | ||||||
| Wheal size (mm) | |||||||
| Known | 218 (78.1) | 9.6 | 7mm (±4) | 162 (74.3) | 10.3 | 162 (74.3) | 11.9 |
| Positive but unknown size | 61 | ||||||
Der p 1 and Der p 2 was <0.35kUA/L in 29 (10%) patients and positive values of Der p 1, Der p 2 or the larger of the two can be seen in Table 4. In children with rhinitis without asthma, a higher positivity of Der p 2 (71.3%) was observed, compared with Der p 1 (30%), without statistical significance. The positivity of Der p 1 was slightly higher in children with a family history of atopy (77.2%) compared to those without atopy in family (63.6%). No difference was observed in Der p 2 (Table 1).
Prevalence of sensitization to Der p components for different Der p specie IgE (sIgE) levels (n=279).
| Der p sIgE Levels | Der p 1, n (%) | Der p 2, n (%) |
|---|---|---|
| Negative levels (<0.35kUA/L) | 74 (26.5) | 66 (23.7) |
| Low (≥0.35 to <0.70kUA/L) | 12 (4.3) | 11 (3.9) |
| Moderate (≥0.70 to <3.50kUA/L) | 32 (11.5) | 30 (10.8) |
| High (≥3.50 to <17.50kUA/L) | 44 (15.8) | 51 (18.3) |
| Very high – class 1 (≥17.50 to <50.00kUA/L) | 52 (18.6) | 57 (20.4) |
| Very high – class 2 (≥50.00 to <100.00kUA/L) | 37 (13.3) | 29 (10.4) |
| Very high – class 3 (≥100.00kUA/L) | 28 (10) | 35 (12.5) |
| Total | 279 (100) | 279 (100) |
The variables age, wheal size in the skin prick-test, Der p 1, Der p 2, total IgE levels and eosinophils do not follow a normal distribution (p<0.001).
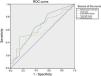
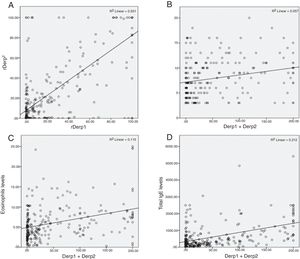
The existence of a correlation between the serological measurements was assessed by computing the corresponding Spearman coefficient and a strong positive correlation was found between the variables Der p 1 and Der p 2 (ρ=0.621, p<0.001). A positive weak correlation was found between the variables Der p 1/Der p 2 and wheal size in the skin prick-test (ρ=0.324, p<0.001; ρ=0.252, p<0.001), between the variables Der p 1/Der p 2 and eosinophils levels (ρ=0.288, p<0.001; ρ=0.371, p<0.001). A positive moderate correlation was found between the variables Der p 1/Der p 2 and total IgE levels (ρ=0.346, p<0.001; ρ=0.449, p<0.001) (Fig. 1).
Correlations between the sIgE levels of HDM extract and single-component Der p 1 and Der p 2 with other serum levels. A) Der p 1 and Der p 2 IgE levels. B) Sum of serum IgE Der p 1 and Der p 2 to wheal size in the skin prick-test. C) Sum of serum IgE Der p 1 and Der p 2 to eosinophils levels. D) Sum of serum IgE Der p 1 and Der p 2 to total IgE levels.
No statistically meaningful correlation was found between the wheal size in the skin prick-test and eosinophils levels (ρ=−0.144, p=0.051) or total IgE levels (ρ=−0.055, p=0.478), nor between Der p 1/Derp 2 and age (ρ=−0.052, p=0.388/0.379).
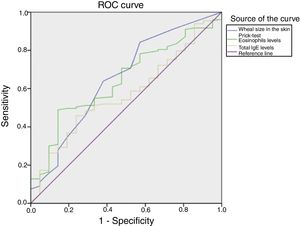
In Fig. 2 we can see the ROC curves illustrating the value of wheal size in the skin prick-test, eosinophils and total IgE levels in predicting positive Der p 1/Der p 2. The risk was estimated by the area under the ROC curve, calculated individually for each parameter and for association of the three variables. The associated analysis of skin prick-test, eosinophils and total IgE levels reveled significant predictive value, with AUC=0.653. Individually, the observed wheal size and eosinophils have significant predictive value which is greater than total IgE levels, with predicted ability of AUC=0.673 and 0.641 versus AUC=0.598. However, all the parameters would be considered to be “poor” at separating positive Der p 1 and Der p 2 levels from negative levels. Using the Youden index, we calculated the optimal cut-off point for the meaningful wheal size (4.5mm), with a sensibility of 80.5% and a specificity of 50% and the same was undertaken for the relative quantity of eosinophils which was 5.55% with a sensibility of 49.8% and a specificity of 82.6%. The predictive ability of IgE total levels was not significant.
DiscussionHDM is a major perennial allergen source and a significant cause of allergic rhinitis and allergic asthma. Sensitization to mite allergens in the first years of life has a significant clinical effect on lung function in pediatric populations, due to wheezing and associates with poorer clinical outcomes in respiratory health in the long term.24 In the same way, a high percentage of patients with a family history of atopy, as can be observed in our sample (72.4%, particularly the children with asthmatic parents), are more prone to suffer from persistent asthma in adulthood.25,26
Prevalence data for HDM allergen sensitization vary from 65 to 130 million persons in the general population worldwide to as many as 50% among asthmatic patients.27 The two-key species of HDM in allergy research are D. pteronyssinus and D. farinae. The Dermatophagoides genus is probably the most researched of all the HDMs, although species dominance varies geographically, suggesting specialized adaptation.27 In Portugal, the high prevalence of acarin fauna is evident in all regions of the country and the importance of the D. pteronyssinus is notorious. According to the acarological map that was performed in our country, D. pteronyssinus is the most prevalent mite in the northern interior area of the country. That is the same area where our study was performed, with a frequency of occurrence of 79.5%. D. pteronyssinus and D. farinae are highly cross-reactive and in some geographical areas D. farinae is more prevalent. It is not the case of our region, because accordingly to the acarological map, the frequency of occurrence of D. farinae is low, about 6.8%.28 In our study, 73.5% and 76.3% of Der p-positive patients were sensitized to Der p 1 and Der p 2, respectively. The rate of Der p sensitization is comparable to rates reported for European cohorts (80%).24
Although at least 20 HDM allergen components have been identified and sequenced, several studies have demonstrated that clinically Der p 1 and Der p 2 are the most important HDM allergens,24,29,30 and this was also observed in our Der p-sensitized individuals. Ten per cent of the tested patients (29/279) were negative to both Der p 1 and Der p 2. Therefore, the present study shows that Der p 1 and Der p 2 are the major allergenic HDM components in our group of Portuguese patients.
The high correlation between serum eosinophil levels and total IgE levels against Der p 1 and Der p 2, further supports the dominant role of both allergens in the human IgE response against HDM in Portugal. The observed wheal size and eosinophils have significant predictive ability to separate positive Der p 1 and Der p 2 levels from negative levels and the optimal cut-off point of 4.5mm of wheal size displays a sensibility of 80.5% and a specificity of 50% and 5.55% eosinophils with a sensibility of 49.8% and a specificity of 82.6% (Fig. 2).
Allergen immunotherapy shows some potential for being disease-modifying by inducing beneficial immunological changes and by completely or partially abrogating the inception of asthma and new allergen sensitizations. It appears to improve clinical symptoms (nasal, ocular, and respiratory), to reduce rescue medication needs, to improve lung function indices and, more importantly, it has the potential to develop intrinsic disease-modifying effects such that the allergic inception of asthma and acquisition of new sensitizations can be completely or partially abrogated.31 In our sample, about 71.3% of the patients were asthmatic, the vast majority had rhinitis (87.8%) and only 28.7% had rhinitis exclusively. The advantages of treatment institution can be relevant, but since vaccines currently marketed for D. pteronyssinus are only standardized for Der p 1 and Der p 2, this means that for our sample only 89.6% of the children were eligible for HDM IT. Knowledge of the molecular allergen profile contributes to the characterization of the patient's risk profile, because it describes the primary sensitization. It also helps in the selection of patients for sIT with allergens and optimizes the choice of immunotherapy composition.
Recently, Der p 23, found in the chitinous membrane of the mite fecal ball, has been discovered to bind IgE with titers similar to Der p 1 and 2 and have high activity in basophil degranulation tests. The titers showed a strong concordance with binding to Der p 1 and 2. But some subjects have high IgE binding to Der p 23 without binding to Der p 1 or 2.11,32 According to these recent findings, it will be important to study in our sample the 10% of patients with Der p 1 and Der p 2 negative values and understand if they have positive Der p 23 values. At the time of this study, Der p 23 was not commercially available, so this will be object of study in the future.
In summary, the present study confirmed that Der p 1 and Der p 2 are major HDM allergen components in our pediatric population of a hospital in the North of Portugal since 73.5% and 76.3% of Dermotophagoide pteronissimus positive patients were sensitized to Der p 1 and Der p 2, respectively. The study also showed that the Der p 1 and Der p 2 assay was negative in 10.4% (29/279) patients. Something similar has been already demonstrated for other relevant aeroallergens.33,34 This, together with our results, proves that the study of allergenic sources by both skin prick-tests or specific IgE constitutes an incomplete approach in order to a right prescription of sIT. As vaccines for D. pteronyssinus that are currently marketed are standardized only for Der p 1 and Der p 2 allergens, the authors conclude that there may be an advantage in determining Der p 1/Der p 2 levels in patients with a positive prick-test and clinical indication for sIT prior to deciding initiation of immunotherapy or not, since 10% of children with clinical features of mite house dust allergy will not benefit with this treatment, with all the personal and economic efforts involved.
Conflict of interestThe authors declare that they do not to have any conflict of interest.
Please cite this article as: Peixoto S, Soares J, Monteiro T, Carvalho M, Santos M, Simões C, et al. Evaluación de la sensibilización a Der p 1 y Der p 2 en una población pediátrica del Norte de Portugal. An Pediatr (Barc). 2018;89:162–169.
This data was presented as poster form at EAACI 2017 – The European Academy of Allergy and Clinical Immunology Annual Congress, in Helsinki.