To determine the prevalence of psychiatric disorders in primary care paediatrics in Atlantic Galicia.
MethodsAn observational, descriptive, cross-sectional prevalence study was carried out in 9 outpatient clinics in A Coruña and Pontevedra with a population of 8,293 children between September and November 2015. A total of 1,286 randomly selected patients from 0 to 14 years of age were included. From the medical history was registered: age, sex, psychiatric diagnosis established by DSM-IV-TR criteria in its five axes, professionals who participated in the diagnosis and treatment of the process and what type of treatment was received. Authorisation was obtained from the Research Ethics Committee of Galicia number 2015/427.
Results148 of 1,286 patients presented psychiatric pathology (11.5% IC 95% 9.73–13.29), 68% male. Between 0 and 5 years, the prevalence was 4.5%; between 6 y and 10 y, 18.5% and between 11 y and 14 y, 22%. Symptoms lasted a median of 25 months. The most frequent pathologies in 1286 patients were ADHD (5.36%), language disorders (3.42%), learning disorders (3.26%), anxiety-depressive disorders (2.4%) and behaviour disorders (1.87%). Of the 148 cases, 47% had comorbidity with another mental disorder. Most of them required attention by multiple social, health and educational professionals; 33% received psychopharmacological treatment.
ConclusionsThe prevalence of psychiatric disorders in paediatric primary care is frequent, chronic and complex, increases with age and requires many health, educational and social resources.
Conocer la prevalencia de patología psiquiátrica en atención primaria en la Galicia atlántica.
MétodosSe realizó un estudio observacional, descriptivo, transversal de prevalencia, en 9 consultas de A Coruña y Pontevedra, con una población de 8.293 niños, entre septiembre y noviembre del 2015. Se incluyó a 1.286 pacientes entre 0 y 14 años que acudieron a las consultas en unos días aleatoriamente seleccionados. Se registraron los siguientes datos de la historia clínica: edad, sexo, diagnóstico psiquiátrico establecido por criterios DSM-IV-TR en sus 5 ejes. Se determinó qué profesionales intervinieron en el diagnóstico y tratamiento del proceso y qué tipo de tratamiento recibían. Se obtuvo la autorización del Comité de Ética de Investigación de Galicia número 2015/427.
ResultadosCiento cuarenta y ocho de los 1.286 pacientes presentaban patología psiquiátrica (11,5%, IC del 95%, 9,73-13,29), 68% varones. Entre los 0 y 5 años la prevalencia fue del 4,5%; entre los 6 y 10 del 18,5% y entre los 11 y 14, del 22%. El tiempo de duración de los síntomas tenía una mediana de 25 meses. Las patologías más frecuentes en los 1.286 pacientes fueron TDAH (5,36%), trastornos del lenguaje (3,42%), trastornos del aprendizaje (3,26%) trastornos ansioso-depresivos (2,4%) y trastornos de la conducta (1,87%). De los 148 casos, el 47% presentaba comorbilidad con otro trastorno mental; la mayoría precisó atención por múltiples profesionales del ámbito social, sanitario y educativo; un 33% recibía tratamiento psicofarmacológico.
ConclusionesLa prevalencia de patología psiquiátrica en pediatría de atención primaria es frecuente, crónica y compleja, aumenta con la edad y precisa muchos recursos sanitarios, educativos y sociales.
It is estimated that 20% of children worldwide have mental disorders, and that these constitute the main cause of disability in young people.1–4
Most mental disorders in adults have onset during childhood or adolescence.5 There is evidence that early detection of these disorders allows early intervention, which could lead to better outcomes.6–8 For this reason, in 2009 the American Academic of Pediatrics published guidelines that recommended that clinicians working in primary care (PC) and other professionals involved in child health monitor the development of children during routine checkups and perform age-appropriate screening tests.9
The most recent data on the prevalence of mental disorders in child and adolescent psychiatric disorders (CAPDs) come from large survey-based studies that use questionnaires based on DSM-IV criteria to collect data from school-aged children and their families. For instance, a study conducted in 2015 in Australia in children aged 4–17 years found an overall prevalence of 13.9% (16.3% in male and 11.5% in female participants), with attention-deficit hyperactivity disorder (ADHD) being the most common disorder (prevalence, 7.4%), followed by anxiety disorders (6.9%), depressive disorders (2.8%) and conduct disorder (2.1%), and psychiatric comorbidities in 30% of affected children.10
Some of the large meta-analyses in the literature have calculated a prevalence of 12% applying DSM criteria and based on health surveys of the general through administration of questionnaires by non-clinical interviewers or self-completion.11
Current evidence suggests that many mental disorders are underdiagnosed in the population aged less than 18 years.12 Some possible reasons are the lack of appropriate education or training of paediatricians on mental disorders, the scarce time paediatricians can devote to each patient, or an unwillingness to recognise the presence of these problems due to the stigma that they carry.
In Spain, as is the case with neighbouring countries, the prevalence of child and adolescent psychiatric disorders is of approximately 20%. In addition, the disorders are severe in 4%–5% of the total cases.13–16
Few prevalence studies have been conducted in the 0–14 years age range, and even fewer have explored neurodevelopmental disorders as well as mood and behavioural disorders and the associated psychiatric and medical comorbidities. The aim of this study was to determine the prevalence of CAPDs in the Galician population that sought care in PC paediatrics clinics for any reason.
MethodsDesign: we conducted a cross-sectional, observational, descriptive prevalence study in 9 PC paediatrics clinics in the provinces of A Coruña and Pontevedra between September and November 2015, which had an overall catchment population of 8,293 children aged 0–14 years.
Sample: we calculated the sample size needed to estimate the prevalence of CAPDs assuming an approximate value of 20%,1–4,12 for a 95% confidence level and a precision of ±2.18%; we included a sample size of n=1286 children. We recruited participants from the 9 participating PC centres: assuming an average of 20 visits per day, we included every child aged 0–14 years that visited the participating clinics during a randomly selected number of days (from 7 to 10 days) proportionally to the size of the caseload of each centre.
Measurements: we interviewed each patient and reviewed their health records to collect the following information: age, sex, presence of active CAPDs, age of onset, psychological diagnosis based on DSM-IV-TR criteria including all 5 axes, presence of Axis I comorbidities, presence of concurrent severe disease or stress, and assessment of symptom severity by means of the global assessment of functioning (GAF). We also investigated which health professionals were involved in the diagnosis and treatment of the disorder, and the type of treatment received by patients.
The criteria we used to diagnose detected CAPDs were those established by the DSM-IV-TR.17 Although a new version is now available (the DSM-V), the new system no longer describes psychiatric disorders in terms of the 5 axes, and we believed that a multiaxial assessment would provide very relevant information to understand the detected disorders in their different dimensions.
The 5 axes under study were:
- -
Axis I: psychological diagnoses.
- -
Axis II: presence or absence of intellectual disability.
- -
Axis III: presence of relevant acute or chronic medical conditions.
- -
Axis IV: contributing stressful factors.
- -
Axis V: global assessment of functioning (GAF).
We ought to note that we updated the now obsolete term “mental retardation” from the DSM-IV-TR to the DSM-V terms “global developmental delay” (in children aged less than 5 years) or “intellectual disability” (in older children). We also chose to include ADHD in the umbrella of neurodevelopmental disorders, even though the latter classification did not exist in the DSM-IV-TR.
The diagnoses were reviewed by a child psychiatrist that works as a consultant for our working group.
Inclusion criteria: to be included in the study as cases of CAPD at the time of data collection, patients had to meet at least one of the following criteria:
- -
Currently followed up by a mental health unit (MHU), rehabilitation unit or paediatric neurology unit, with a documented DSM-IV-TR diagnosis.
- -
Currently receiving chronic pharmacological treatment, documented in the prescriptions database of the electronic health record system of the Galician Health Service (Ianus), with a drug classified in the category of anxiolytics, antipsychotics, antidepressants, stimulants, mood stabilisers or atomoxetine.
- -
Presence of an episode meeting the criteria for a DSM-IV-TR diagnosis documented by the paediatrician in the patient's health record and being treated or evaluated at the time of data collection.
Exclusion criteria:
- -
Psychiatric diagnosis in the absence of active psychiatric symptoms and patient discharge from followup.
- -
The symptoms could be explained by a known general medical condition or a sensory deficit.
We did not analyse patients that returned to the clinic during the period under study.
Statistical analysis: we performed a descriptive analysis of the variables under study. We have summarised qualitative or categorical variables as absolute frequency, percentage and 95% confidence interval (CI), and quantitative variables as mean±standard deviation and median. We analysed the association between qualitative variables with the chi square test.
Ethical and legal aspects: we obtained the authorisation of the Comité Autonómico de Ética de la Investigación de Galicia (Research Ethics Committee of the Autonomous Community of Galicia [CAEIG]) under project number 2015/427. We requested written informed consent from both legal guardians of each patient and/or from mature minors. We accessed health records in adherence with current law, guaranteeing the confidentiality of the data as mandated by Law 15/1999.
ResultsFrom a total population of 8,293 children, we included 1,531 primary care visits in the study. We then excluded repeat visits by patients seen more than once, which resulted in a final sample of 1,286 patients.
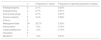
Table 1 shows the frequency distribution of the sample under study by sex, age group, primary care centre and health district. The mean age of the sample under study was 5.85±4.34 years.
Characteristics of the sample under study in terms of sex, age group, primary care centre and health district.
| n | Percentage | |
|---|---|---|
| Sex | ||
| Male | 674 | 52.9 |
| Female | 600 | 47.1 |
| Age | ||
| <5 years | 710 | 55.7 |
| 6–10 years | 349 | 27.4 |
| >11 years | 215 | 16.9 |
| Primary care centre | ||
| CS Val Miñor | 190 | 14.8 |
| CS Calo | 159 | 12.4 |
| CS Casa del Mar Coruña | 144 | 11.2 |
| CS Cerceda-Culleredo | 126 | 9.8 |
| CS Lousame | 140 | 10.9 |
| CS Marín | 145 | 11.3 |
| CS Mos | 125 | 9.7 |
| CS Tomiño | 126 | 9.8 |
| CS Bueu | 131 | 10.2 |
| Health district | ||
| A Coruña | 270 | 21 |
| Santiago | 299 | 23.3 |
| Pontevedra | 276 | 21.5 |
| Vigo | 441 | 34.3 |
CS, Centro de Salud (primary care centre).
Of the 1,286 patients, 11.5% (95% CI, 9.73%–13.29%; n=148 cases), had active CAPDs at the time of the visit, and 68.2% of these patients were male; the prevalence ranged between 16.4% at the Centro de Salud Calo-Teo and 6.2% at the Centro de Salud Marín, and the differences between primary care centres were not statistically significant (P=.185). Table 2 summarises the data by primary care centre.
Presence of psychiatric disorders at the time of consultation by primary care centre.
| n | Percentage | |
|---|---|---|
| CS Val Miñor | 22 | 11.6 |
| CS Calo | 26 | 16.4 |
| CS Casa del Mar Coruña | 13 | 9 |
| CS Cerceda-Culleredo | 15 | 11.9 |
| CS Lousame | 22 | 15.7 |
| CS Marín | 9 | 6.2 |
| CS Mos | 13 | 10.4 |
| CS Tomiño | 13 | 10.3 |
| CS Bueu | 15 | 11.5 |
CS, Centro de Salud (primary care centre).
By age group, the prevalence was 4.5% (77.4% male) in children aged 0–5 years; 18.5% (66.6% male) in children aged 6–10 years, and 22% (65% male) in children aged 11–14 years.
The mean age of cases was 106.16±43.44 months (8.84±3.62 years), while the mean age of the rest of patients was 65.59±51.36 months (5.46±4.28 years). The median duration of symptoms was 25 months (2.08 years).
We proceed to present the results of the psychological diagnosis of cases based on the 5 axes of the DSM-IV-TR.
Axis I: psychological diagnosisTables 3 and 4 present information on the detected cases of CAPDs.
Prevalence of psychiatric disorders based on Axis I, psychological diagnosis, of the DSM-IV-TR in patients with psychiatric disorders and the overall sample of the general population that received primary care services with the corresponding 95% confidence intervals (I).
| Disorder | n | % patients with MH disorders (148) | 95% CI | % general population seeking care (1.286) | 95% CI |
|---|---|---|---|---|---|
| Neurodevelopmental disorders | 121 | 81.70 | 75.2–88.31 | 9.40 | 7.77–11.04 |
| Global developmental delay | 7 | 4.73 | 0.97–8.49 | 0.54 | 0.10–0.98 |
| Learning disorder | 42 | 28.30 | 20.77–35.98 | 3.27 | 2.25–4.27 |
| Dyslexia | 26 | 17.56 | 11.10–24.03 | 2.02 | 1.21–2.83 |
| Mathematics disorder | 3 | 2.02 | 0.42–5.81 | 0.23 | 0.05–0.68 |
| Disorder of written expression | 12 | 8.11 | 3.37–12.84 | 0.93 | 0.37–1.50 |
| Learning disorder NOS | 15 | 10.13 | 4.93–15.93 | 1.66 | 0.54–1.79 |
| Motor skills disorder | 14 | 9.46 | 4.41–14.51 | 1.09 | 0.48–1.69 |
| Language and communication disorders | 44 | 29.73 | 22.03–37.43 | 3.42 | 2.39–4.45 |
| Expressive language disorder | 19 | 12.84 | 7.11–18.56 | 1.48 | 0.78–2.77 |
| Mixed language disorder | 11 | 7.43 | 2.87–11.1 | 0.85 | 0.31–1.34 |
| Phonological disorder | 21 | 14.19 | 8.23–20.15 | 1.63 | 0.90–2.36 |
| Stuttering | 2 | 1.35 | 0.16–4.8 | 0.15 | 0.02–0.56 |
| Pervasive developmental disorder | 11 | 7.43 | 2.87–11.1 | 0.85 | 0.31–1.34 |
| Autism spectrum disorder | 9 | 6.08 | 1.89–10.27 | 0.70 | 0.25–1.94 |
| Asperger's disorder | 2 | 1.35 | 0.16–4.8 | 0.15 | 0.02–0.56 |
| Enuresis | 16 | 10.81 | 5.47–16.15 | 1.24 | 0.59–1.89 |
| Encopresis | 7 | 4.73 | 0.97–8.49 | 0.54 | 0.10–0.98 |
| Tics | 16 | 10.81 | 5.47–16.15 | 1.24 | 0.59–1.89 |
| Tourette's disorder | 0 | ||||
| Vocal tic disorder | 2 | 1.35 | 0.16–4.8 | 0.15 | 0.02–0.56 |
| Transient tic disorder | 14 | 9.46 | 4.41–14.51 | 1.09 | 0.48–1.69 |
| ADHD | 69 | 46.20 | 38.25–54.99 | 5.36 | 4.09–6.64 |
CI, confidence interval; MH, mental health; NOS, not otherwise specified.
Prevalence of psychiatric disorders based on Axis I, psychological diagnosis, of the DSM-IV-TR in patients with psychiatric disorders and the overall sample of the general population that received primary care services with the corresponding 95% confidence intervals (II).
| Disorder | n | % patients with MH disorders (148) | 95% CI | % general population seeking care (1286) | 95% CI |
|---|---|---|---|---|---|
| Disruptive behaviour disorders | 24 | 16.21 | 9.94–22.49 | 1.86 | 1.08–2.64 |
| Conduct disorder | 2 | 1.35 | 0.16–4.8 | 0.16 | 0.02–0.56 |
| Oppositional defiant disorder | 10 | 6.76 | 2.37–11.14 | 0.78 | 0.26–1.30 |
| Disruptive behaviour disorder NOS | 12 | 8.11 | 3.37–12.84 | 0.93 | 0.37–1.5 |
| Anxiety or depressive disorder | 31 | 20.94 | 14.05–7.84 | 2.41 | 1.53–3.29 |
| Major depressive disorder | 0 | ||||
| Dysthymic disorder | 2 | 1.35 | 0.16–4.8 | 0.16 | 0.02–0.56 |
| Specific phobia | 2 | 1.35 | 0.16–4.8 | 0.16 | 0.02–0.56 |
| Social phobia | 0 | ||||
| Obsessive- compulsive disorders | 2 | 1.35 | 0.16–4.8 | 0.16 | 0.02–0.56 |
| Separation anxiety | 5 | 3.38 | 1.10–7.70 | 0.39 | 0.12–0.90 |
| Anxiety disorder NOS | 21 | 14.19 | 8.23–20.15 | 1.63 | 0.9–2.36 |
| Eating disorder | 9 | 6.08 | 1.89–10.27 | 0.7 | 0.25–1.94 |
| Eating disorders of early childhood | 5 | 3.38 | 1.10–7.70 | 0.39 | 0.12–0.90 |
| Anorexia nervosa | 1 | 0.67 | 0.02–3.71 | 0.08 | 0.002–0.43 |
| Bulimia nervosa | 0 | ||||
| Binge eating | 2 | 1.35 | 0.16–4.80 | 0.16 | 0.02–0.56 |
| Sleep disorders | 16 | 10.81 | 5.47–16.51 | 1.24 | 0.6–1.89 |
| Insomnia | 7 | 4.73 | 0.97–8.49 | 0.54 | 0.10–0.98 |
| Sleep terror disorder | 1 | 0.67 | 0.02–3.71 | 0.08 | 0.002–0.43 |
| Nightmare disorder | 3 | 2.02 | 0.42–5.81 | 0.23 | 0.05–0.68 |
| Sleepwalking disorder | 4 | 2.70 | 0.74–6.77 | 0.31 | 0.08–0.79 |
| Sleep disorder NOS | 3 | 2.02 | 0.42–5.81 | 0.23 | 0.05–0.68 |
| Others | |||||
| Psychotic disorder | 1 | 0.67 | 0.02–3.71 | 0.08 | 0.002–0.43 |
| Bipolar disorder | 1 | 0.67 | 0.02–3.71 | 0.08 | 0.002–0.43 |
| Tobacco/alcohol/cannabis abuse/dependency | 0 |
CI, confidence interval; MH, mental health; NOS, not otherwise specified.
The most frequent disorders in the 1,286 patients were neurodevelopmental disorders (9.4%), chief among them ADHD (5.36%), language and communication disorders (3.42%) and learning disorders (3.26%). These were followed by anxiety and depressive disorders (2.4%) and disruptive behaviour disorders (1.87%).
In the 148 cases, 81.7% of the diagnoses corresponded to neurodevelopmental disorders, and ADHD amounted to 46.2% of the total diagnoses in this category, language disorders to 29.7% and learning disorders to 28.3%. We found Axis I comorbidities in 47.3% of the cases (95% CI, 38.25%–54.99%; n=69 patients).
In the analysis by age group, we found that cases in children aged less than 5 years corresponded to language disorders in 45.2% of cases, followed by pervasive developmental disorders and motor still disorders in 22.6%. Between 6 and 10 years, the most frequent disorder, with a 53.7% prevalence, was ADHD, followed by learning disorders in 29.6% and language disorders in 25.9%. In children aged more than 10 years, ADHD amounted to 62.7% of cases, followed by learning and language disorders (25.4% each). Table 5 shows the prevalence of the different disorders in these 3 age groups.
Prevalence of Axis I DSM-IV-TR diagnoses by age range.
| Disorder | n | 0–5 years (31) | 6–10 years (54) | >10 years (59) |
|---|---|---|---|---|
| Neurodevelopmental disorders | 121 | 24 (77.4%) | 50 (92.6%) | 47 (79.7%) |
| Global developmental delay | 7 | 7 (22.6%) | 0 | 0 |
| Learning disorders | 42 | 4 (12.9%) | 16 (29.6%) | 21 (35.6%) |
| Dyslexia | 26 | 1 (3.2%) | 9 (16.7%) | 16 (27.1%) |
| Mathematics disorder | 3 | 0 | 2 (3.7%) | 1 (1.7%) |
| Written expression disorder | 12 | 0 | 5 (9.3%) | 7 (11.9%) |
| Learning disorder NOS | 15 | 3 (9.7%) | 5 (9.3%) | 7 (11.9) |
| Motor skills disorder | 14 | 7 (22.6%) | 5 (9.3%) | 2 (3.4%) |
| Communication/language disorder | 43 | 14 (45.2%) | 14 (25.9%) | 15 (25.4%) |
| Expressive language disorder | 18 | 8 (25.8%) | 4 (7.4%) | 6 (10.2%) |
| Mixed language disorder | 11 | 3 (9.7%) | 4 (7.4%) | 4 (6.8%) |
| Phonological disorder | 21 | 4 (12.9%) | 9 (16.7%) | 8 (13.6%) |
| Stuttering | 2 | 0 | 0 | 2 (3.4%) |
| Pervasive developmental disorders | 11 | 5 (16.1%) | 3 (5.6%) | 3 (5.1%) |
| Autism spectrum disorder | 9 | 5 (16.1%) | 2 (3.7%) | 2 (3.4%) |
| Asperger's disorder | 2 | 0 | 1 (1.9%) | 1 (1.7%) |
| Enuresis | 16 | 1 (3.2%) | 12 (22.2%) | 3 (5.1%) |
| Encopresis | 7 | 1 (3.2%) | 5 (9.3%) | 1 (1.7%) |
| Tic disorders | 16 | 0 | 7 (13%) | 9 (15.3%) |
| Vocal tic disorder | 2 | 0 | 0 | 2 (3.4%) |
| Transient tic disorder | 14 | 0 | 7 (13%) | 7 (11.9%) |
| ADHD | 69 | 3 (10%) | 29 (53.7%) | 37 (62.7%) |
| Disruptive behaviour disorders | 24 | 5 (16.1%) | 7 (13%) | 12 (20.3%) |
| Conduct disorder | 2 | 0 | 1 (1.9%) | 1 (1.7%) |
| Oppositional-defiant disorder | 10 | 3 (9.7%) | 2 (3.7%) | 5 (8.5%) |
| Disruptive behaviour disorder NOS | 12 | 2 (6.5%) | 4 (7.4%) | 6 (12.2%) |
| Anxiety/depressive disorders | 31 | 3 (9.7%) | 12 (22.2%) | 16 (27.1%) |
| Dysthymic disorder | 2 | 0 | 0 | 2 (3.4%) |
| Specific phobia | 2 | 1 (3.2%) | 1 (1.9%) | 0 |
| Obsessive-compulsive disorder | 2 | 1 (3.2%) | 1 (1.9%) | 0 |
| Separation anxiety disorder | 5 | 2 (6.5%) | 1 (1.9%) | 2 (3.4%) |
| Anxiety/depressive disorder NOS | 21 | 0 | 9 (16.7%) | 12 (20.3%) |
| Eating disorders | 9 | 1 (3.2%) | 3 (5.6%) | 5 (8.5%) |
| Eating disorder of childhood | 5 | 1 (3.2%) | 1 (1.9%) | 3 (5.1%) |
| Anorexia nervosa | 1 | 0 | 0 | 1 (1.7%) |
| Binge eating | 2 | 0 | 0 | 2 (3.4%) |
| Eating disorder NOS | 5 | 0 | 3 (5.6%) | 2 (3.4%) |
| Sleep disorders | 16 | 3 (9.7%) | 7 (13%) | 6 (10.2%) |
| Insomnia | 7 | 0 | 3 (5.6%) | 4 (6.8%) |
| Sleep terror disorder | 1 | 1 (3.2%) | 0 | 0 |
| Nightmare disorder | 3 | 0 | 3 (5.6%) | 0 |
| Sleepwalking disorder | 4 | 1 (3.2%) | 2 (3.7%) | 1 (1.7%) |
| Sleep disorder NOS | 3 | 1 (3.2%) | 1 (1.9%) | 1 (1.7%) |
| Psychotic disorder | 1 | 0 | 0 | 1 (1.7%) |
| Bipolar disorder | 1 | 0 | 0 | 1 (1.7%) |
NOS, not otherwise specified.
Intellectual disability (ID) was diagnosed in 10% of cases (13 patients). The severity was not specified in 70%.
Axis III: presence of relevant chronic diseaseOf all cases, 43.2% (63 patients) had a relevant chronic condition, most frequently asthma (in 27 patients, 18.5%), obesity (in 17 patients, 11.6%) and neurologic impairment (16 patients, 11.3%).
Axis IV: relevant sources of stressWe found relevant stressful conditions in 28.8% of cases (42 patients), corresponding most frequently to the family (24%, 35 patients). The source of stress was economic problems in 10% and social problems in 8.2%. Other problems found in our study were parental separation (6 patients), disease or death of a family member (5), school bullying (4), child abuse (3) and neglect (2).
Axis V: global assessment functioning scaleOf all patients, 8.3% had very severe or severe symptoms with global assessment functioning (GAF) scores of less than 50 points, 26.2% had moderate symptoms (GAF, 51–60), 20% mild symptoms (GAF, 61–70) and 15% transient symptoms (GAF, 81–90). At the time of data collection, 9.7% of patients were asymptomatic (91–100). Table 6 presents the frequency distribution of GAF scores.
Frequency distribution of scores in the global assessment of functioning scale.
| Global assessment of functioning scale | n | Frequency in cases (148) | 95% confidence interval |
|---|---|---|---|
| 100–91 | 14 | 9.46% | 4.41–14.51 |
| 90–81 | 22 | 14.86% | 8.79–20.93 |
| 80–71 | 30 | 20.27% | 13.45–27.08 |
| 70–61 | 29 | 19.59% | 12.86–26.32 |
| 60–51 | 38 | 25.67% | 18.30–33.05 |
| 50–41 | 7 | 4.73% | 0.97–8.48 |
| 40–31 | 4 | 2.70% | 0.74–6.77 |
| 30–21 | 1 | 0.67% | 0.02–3.71 |
| 20–11 | 0 | ||
| 10–1 | 0 |
Mental health problems were mostly detected by the family, the paediatrician or the school (90% of cases).
The patients in the study were evaluated by different professionals: 57.5% by a school counselling team, 42% by a MHU, 37% by a paediatric neurologist in the public health system, 33.6% by a school teacher, 27.4% by a hearing/speech therapist and 15% by early intervention services. Of all the patients, 44.59% (66 patients) resorted to professionals in the private sector (27.4% to psychologists, 15.5% to speech therapists, 8.2% to paediatric neurologists and 4.8% to psychiatrists).
Table 7 summarises the treatment of the patients: 33.6% had received academic support, 32.9% psychological treatment, 32% hearing/speech therapy, 17.1% occupational therapy and 32.9% pharmacological treatment (3.73% of the general population sample).
The drugs used most often at the time of the study, as can be seen in Table 8, were methylphenidate (26.7%), anticonvulsants (3.4%), antipsychotics (2.7%) and antidepressants (2.1%). When it came to the number of drugs, 41 patients were using 1 drug, four were using 2 drugs, one patient was using 3 drugs and another patient was using 4 drugs.
Pharmacological treatment.
| n | Frequency in cases | Frequency in general population sample | |
|---|---|---|---|
| Antidepressants | 3 | 2.1% | 0.23% |
| Antipsychotics | 4 | 2.7% | 0.31% |
| Anti-anxiety drugs | 1 | 0.7% | 0.07% |
| Anticonvulsants | 5 | 3.4% | 0.38% |
| Lithium | 0 | ||
| Methylphenidate | 39 | 26.7% | 3.03% |
| Atomoxetine | 2 | 1.4% | 0.15% |
| Lisdexamfetamine | 2 | 1.4% | 0.15% |
| Clonidine | 0 | ||
| Melatonin | 1 | 1.4% | 0.07% |
Unlike previous studies, this is the first conducted in Spain in the population aged 0–14 years and including neurodevelopmental, mood and behaviour disorders. Primary care paediatricians conducted the interviews with the support of consulting psychiatrists, and we reviewed the electronic health records to analyse the involvement of other health professionals.
Although we found differences between centres in the detection of CAPDs, they were not statistically significant, so that the identification of psychiatric disorders was homogeneous throughout the sample. The median duration of symptoms was 25 months, which impairment that they cause. As occurs in most published studies,18 the prevalence of CAPDs in our study was greater in male patients.
The considerable frequency of psychiatric comorbidities, which was as high as 47%, was consistent with most of the literature, and this vulnerability is one of the factors that contribute to greater severity and impairment in these disorders. For instance, ADHD, which is a disorder related to the immaturity of executive functions, is often associated with anxiety-depressive disorders and disruptive behaviour disorders, but also, given the immaturity in neurodevelopment, is also frequently associated with reading disorder, tic disorders, enuresis, language or motor delays, etc. The evidence that demonstrates that early and appropriate treatment in childhood can prevent future comorbidities is encouraging.19–21
In our study, the overall prevalence of ADHD was 5.36%. However, it rose to 8.3% in the 6–10 years age range and 17.2% in the 11–14 years age range. Considering that the mean prevalence of ADHD in the community ranges between 5% and 8%,19 children with ADHD use more paediatric care resources,22 which could have to do with the need of pharmacological treatment, behavioural or emotional problems, or an increased risk of accidental injuries.
When it came to psychiatric morbidity in children aged less than 5 years, the most salient finding was the presence in 45% of the patients of language disorders, which can be an early warning sign of autism spectrum disorder or specific language disorders the outcomes of which depend on early intervention.23 Very few studies on the subject have been conducted in this age group in Spain.
In our study, 32.9% of patients with CAPDs (3.73% of the sample of the general population) received pharmacological treatment, mainly methylphenidate. In our study, we found that the use of drugs such as antidepressants or anti-anxiety agents, which family physicians manage frequently in adults in their everyday practice but paediatricians tend not to prescribe in children, was rare. Paediatricians probably need to increase their knowledge and skills in the management of these drugs.
In Spain, contrary to other countries, public PC paediatric services are available free of charge, including monitoring the development and behaviour of children, MHUs, paediatric neurology care and early intervention programmes. However, the fact that 44% of the Galician patients in our sample had to resort to the private sector is an indication that the public resources currently available for management of these disorders may be insufficient.
It is worth noting that in Galicia there are fewer than 3 child psychiatrists per 100000 youth, which ranks this autonomous community in the 3 that invest the least in this field; the ratio exceeds 3 per 100000 when it comes to child psychologists, but it is still low. Furthermore, Galicia is one of the 7 autonomous communities in Spain that does not have day hospital services for children and adolescents with psychiatric disorders. The optimal provider ratio has been estimated at 14.38 psychiatrists per 100000 youth.24
Chief among the limitations of our study is the fact that the sample only represents the Atlantic side of Galicia and not the entire autonomous community, as it only included the areas of Coruña, Santiago, Pontevedra and Vigo. Furthermore, we calculated the target sample size with the aim of finding the overall prevalence of CAPDs as opposed to the prevalence of specific disorders, and thus finding data for the specific prevalence of each disorder would require further studies with different sample sizes specifically focusing on a single disorder.
ConclusionsThrough the years, there has been a shift in the reasons for consultation in PC paediatrics clinics. At present, the severity of infectious diseases has decreased thanks to the progressive introduction of new vaccination schedules, while the demand related to CAPDs has increased from families, schools and society at large. These disorders have a significant impact on the growth and development of the child and adolescent, academic achievement and family and interpersonal relationships. When these disorders become chronic in adulthood, they may be associated with economic and social problems and future disability: they should be one of our next targets for prevention.
The prevalence obtained in this study of CAPDs in the population seeking care in PC paediatric clinics in Galicia was 11.5% (95% CI, 9.73–13.29). The disorders found most frequently in the population under study were neurodevelopmental disorders, within which ADHD, language disorders and learning disorders amounted for most of the total. Anxiety and depressive disorders and behavioural problems were also common.
Chronic disorders are defined as those with symptoms lasting more than 2 years associated with significant health care use, multiple referrals to different specialists and complex evaluations and treatments. All of this must be coordinated by the PC paediatrician, who must guide patients and their families towards efficient solutions and keep them from “falling through the cracks.”
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Amparo Rodríguez Lombardía (Centro de Salud [CS] Casa del Mar, A Coruña), Cristina Sanchez García-Monge (CS Marín, Pontevedra), Teresa Valls Durán (CS Val Miñor, Vigo), María José Durán (child psychiatrist, Pontevedra), Sonia Pértega Díaz (Teaching and Research Unit of the Complejo Hospitalario de A Coruña).
Please cite this article as: Carballal Mariño M, Gago Ageitos A, Ares Alvarez J, del Rio Garma M, García Cendón C, Goicoechea Castaño A, et al. Prevalencia de trastornos del neurodesarrollo, comportamiento y aprendizaje en Atención Primaria. An Pediatr (Barc). 2018;89:153–161.
Previous presentations: this study was presented as an oral communication at the 67th Congress of the Sociedad Galega de Pediatría, November 12, 2016, Santiago de Compostela, Spain. It was also presented as an oral communication at the 65th Congress of the Asociación Española de Pediatría, June 1–3, 2017, Santiago de Compostela, Spain, and awarded the prize to the best oral communication of the AEPap.