Juvenile laryngeal papillomatosis (JLP) is the second most common cause of dysphonia in children, after true vocal cord nodules. The most frequent causative agent is human papillomavirus (HPV) serotypes 6 and 11. The most widely accepted mode of transmission is vertical, through the birth canal of a mother with an active or latent genital infection.1 The prevalence is 1.11–2.59 per 100,000 children.2 We present 6 cases of JLP, a recurrent disease with non-specific clinical symptoms, which should be taken into account in cases of persistent dysphonia.
We conducted a retrospective study of diagnosed cases of JLP during the period from 1 January 2000 to 31 December 2013. We analysed epidemiological data (age at diagnosis, sex), treatment received, sequelae and number of surgical interventions (Table 1). The male–female ratio found was 1:1. The median age at diagnosis was 18 months, with an interquartile range (IQR) of 26.5 months. The common symptoms were dysphonia, nocturnal breathing difficulty and inspiratory stridor. Patient 1 was an uncontrolled pregnancy with maternal serology compatible with a resolved syphilis and hepatitis B infection, premature at 25 weeks gestation, with a birth weight of 1000g. She had associated malnutrition and laryngomalacia. She needed tracheostomy from 14 to 20 months of age (because of respiratory failure secondary to papillomatosis). Patient 2 was the product of an adolescent pregnancy of a mother vaccinated against HPV (Cervarix® 3 doses) at the age of 14. He was diagnosed with recurrent laryngitis. Patient 3 had been an uncontrolled pregnancy. Patient 4 had a maternal history of papillomas on the hands, and was diagnosed with adenoidal hypertrophy and bronchitis. The mother of patient 5 had had previous genital papillomatosis and patient 6 had language acquisition difficulties.
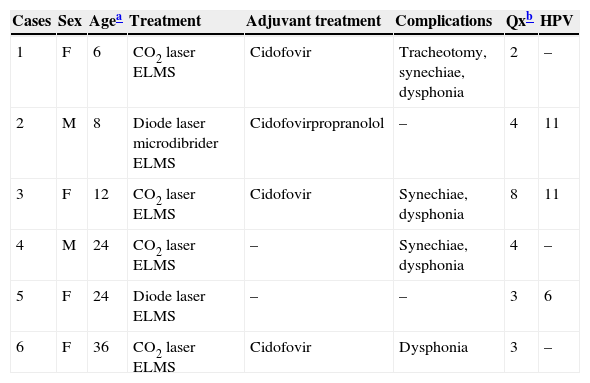
Juvenile laryngeal papillomatosis at the Hospital Clínico Universitario Virgen de la Arrixaca between January 2000 and December 2013.
| Cases | Sex | Agea | Treatment | Adjuvant treatment | Complications | Qxb | HPV |
|---|---|---|---|---|---|---|---|
| 1 | F | 6 | CO2 laser ELMS | Cidofovir | Tracheotomy, synechiae, dysphonia | 2 | – |
| 2 | M | 8 | Diode laser microdibrider ELMS | Cidofovirpropranolol | – | 4 | 11 |
| 3 | F | 12 | CO2 laser ELMS | Cidofovir | Synechiae, dysphonia | 8 | 11 |
| 4 | M | 24 | CO2 laser ELMS | – | Synechiae, dysphonia | 4 | – |
| 5 | F | 24 | Diode laser ELMS | – | – | 3 | 6 |
| 6 | F | 36 | CO2 laser ELMS | Cidofovir | Dysphonia | 3 | – |
ELMS: endolaryngeal microsurgery; F: female; HPV: human papillomavirus; M: male.
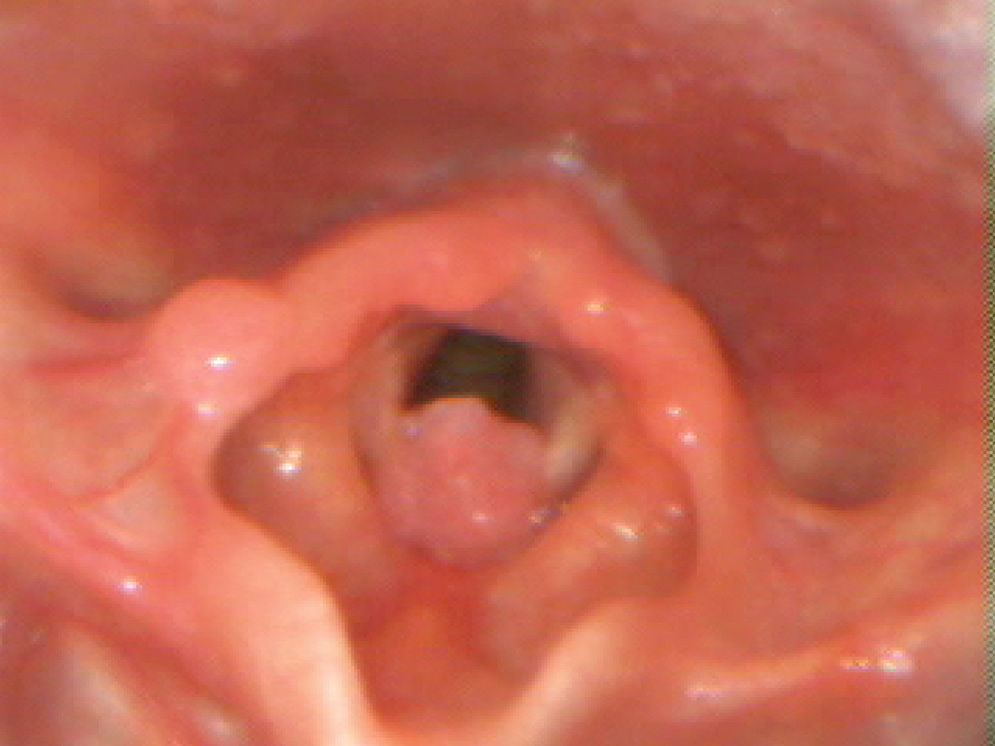
The laryngeal papillomas were detected by fibre-optic laryngoscopy, and an excision was performed (Fig. 1) by endolaryngeal microsurgery. In 4 of the 6 cases they received intraoperative adjuvant treatment with intralesional cidofovir on at least one occasion. Case 2 also received oral propranolol daily for a year. The histological findings were consistent with papillomatosis, and serotype HPV-11 was identified in cases 2 and 3 and HPV-6 in case 6.
The vocal cords are the most frequent site of JLP. Distal spread has been associated with poorer prognosis and with HPV-11 infection.3 The classic presentation is persistent dysphonia with weak crying between 2 and 4 years of age. The second most common symptom is stridor, first inspiratory and then biphasic. Less common presenting symptoms include chronic cough, recurrent pneumonia, failure to thrive, dyspnoea, dysphagia and acute respiratory distress, especially in infants with an upper respiratory tract infection.4
The differential diagnosis with this disease must be made with other causes of airway obstruction, primarily at the pharyngo-laryngeal level (laryngomalacia, vocal cord paralysis, glottic or subglottic granulomas or cysts, laryngitis, congenital or acquired subglottic stenosis, haemangiomas and traumas) and at the tracheal level (tracheal stenosis, tracheomalacia, extrinsic compression by abnormal vascular structures). Less commonly it will be confused with abnormalities at the nasal level (choanal atresia/stenosis, pyriform aperture stenosis, adenoid hypertrophy, tumours, rhinitis and foreign bodies), as well as at the pharyngeal level (nasopharyngeal stenosis, tonsillar hypertrophy, macroglossia and craniofacial abnormalities).
It is not unusual in JLP for an erroneous initial diagnosis to be made, given the range of non-specific symptoms it shares with other common respiratory diseases. In the series of cases described by Zacharisen and Conley,5 croup, laryngomalacia and asthma were the most common misdiagnoses before reaching a definitive diagnosis. One must remain alert to recurrent or progressive respiratory symptoms that do not follow the natural course of the most common diseases and do not improve with conventional treatment.
Delay in diagnosis could lead to obstruction of the upper airway with the risk of acute respiratory failure. Coope and Connett6 report the case of a five-year-old child with persistent dysphonia diagnosed with asthma, who died as a result of airway collapse. The post mortem showed obstruction of the upper airway by papillomatosis.
The natural course of the condition can be unpredictable: it may remit spontaneously, remain stable or show aggressive growth, although the most common outcome is spontaneous remission with increasing age, and after numerous surgical interventions to excise the lesions.2 In the presence of persistent dysphonia with or without stridor, laryngoscopic examination may offer early diagnosis and thereby avoid the development of associated complications.
Please cite this article as: Fita AM, Díaz Manzano JA, Reyes Domínguez SB, Pastor Costa P, Navarro Mingorance A. Disfonía infantil precoz como síntoma de alerta de la papilomatosis laríngea juvenil. An Pediatr (Barc). 2015;83:211–212.