Persistent pneumothorax is defined as pneumothorax of more than five days’ duration.1 It is associated with increased morbidity and cost of care.2,3 The most widely accepted treatment for it is pleurodesis. Several types of pleurodesis have been proposed, including surgical approaches and the instillation of different chemicals in the intrapleural space. The long-term impact of the use of these substances in children is not known,1,2 and thus surgery is usually the approach chosen in the paediatric population.2 Autologous blood patch (ABP) pleurodesis has proven to be a simple, inexpensive, efficacious and safe method.2,4 We present the case of the first patient with persistent bilateral pneumothorax we have treated successfully with ABP.
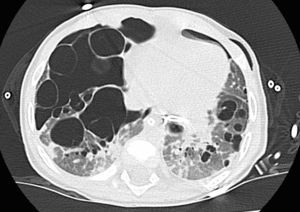
The patient was an infant aged 8 months with a crusty papular rash with onset at 3 months and weight faltering starting at age 5 months. He was admitted to hospital due to respiratory distress of 48h duration. The findings of plain radiography were compatible with interstitial lung disease and left pneumothorax. A high-resolution CT scan of the chest revealed multiple bilateral cyst-like lesions, left pneumothorax, a mild mediastinal shift and partial collapse of the left lung (Fig. 1). The patient was admitted to the paediatric ICU to undergo drainage of the air leak. A skin biopsy and bronchoalveolar lavage were performed, with analysis of the latter finding 11.6% of CD1 cells in cytometry and 20% of CD1 cells in the cytological examination, both of which are compatible with Langerhans cell histiocytosis (LCH). There were no significant abnormal findings in any of the other diagnostic tests. Treatment for systemic LCH with lung involvement was initiated with vinblastine and corticosteroids.
A chest tube was inserted in the left pleura, and by 48h the patient had developed a right pneumothorax requiring placement of another chest tube, with signs of a continuous bilateral air leak. Persistence of the bilateral pneumothorax led to performance of ABPs in the left and right sides on days 40 and 42 of admission, respectively. The air leak ceased immediately in the left hemithorax, and 15min after the procedure in the right hemithorax. The follow-up X-rays showed complete resolution on both sides of the chest (Fig. 2). The patient did not experience pain or other complications from the ABP, and remained asymptomatic at two years’ followup.
Persistent air leak is an infrequent complication following thoracic surgery, spontaneous pneumothorax, mechanical ventilation or lung infection.2 It is defined as an air leak lasting more than five days, and is associated with increased morbidity, hospital length of stay and cost of care.1–3 There is a large body of evidence on chemical pleurodesis, which consists in the introduction of different substances in the pleural space (talc, tetracycline, doxycycline and bleomycin) to trigger an inflammatory response in the cavity that leads to adhesion of the visceral and parietal pleurae. Previous research has described a decline in lung function following chemical pleurodesis in adults.4,5 The long-term effects of the use of these substances in children are not well understood. Autologous blood patch pleurodesis has been studied extensively in adults, and some authors propose it as the gold standard for treatment because it is cheap, quick and safe.6 There is a published case series of children treated with this technique, which was efficacious (100% success rate) and safe.2 In the case presented here, ABP was chosen due to the presence of underlying lung disease, as there is no evidence of a decline in lung function following ABP, while reduced function has been observed following the use of other substances.4,5 The technique consists in the instillation through a chest tube of 1–2mL/kg of blood previously extracted from the patient adhering to strict aseptic technique. After the blood is instilled, the cavity is rinsed with 10mL of physiological saline solution and the chest tube is suspended 60cm overhead for 30min to prevent drainage of the instilled blood while allowing air to escape the chest.2,4,5 We recommend changing positions to facilitate a better distribution of the blood.
While the exact closure mechanism is not understood, it has been postulated that the blood acts as a patch that directly seals the defect, followed by an inflammatory response in the pleural cavity.6 In the case presented here, treatment with vinblastine and corticosteroids promoted the persistence of pneumothorax, making the patch-like effect all the more relevant.
The most frequent complications of ABP are fever, pneumothorax and empyema. Unlike other techniques, it is painless, does not require sedation or analgesia, and can be repeated. We did not observe any of the previously described complications in our patient.
Autologous blood patch pleurodesis is a safe, inexpensive and efficacious treatment for persistent air leak. Larger studies need to be conducted in the paediatric population prior to recommending its routine use.
We wish to thank the nursing staff of the PICU and the paediatric oncology ward.
Please cite this article as: Navarro Mingorance A, Pastor Vivero MD, León León MC, Reyes Domínguez SB, Fuster Soler JL. Pleurodesis con sangre autóloga: una solución, segura y eficaz para el tratamiento de neumotórax persistente. An Pediatr (Barc). 2016;85:157–158.