Case 1: female patient aged 15 years that sought care at her assigned health care centre for irregular menstruation. There was no personal or family history of interest, and the patient was not taking any medication. Her age of menarche was 11.5 years.
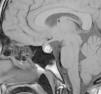
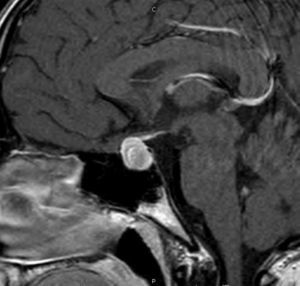
The patient was referred to the paediatric endocrinology unit after testing revealed an elevated prolactin level (198ng/mL; normal value range, 8.5–26.5ng/mL). During the structured interview, the patient reported one year of intermittent blurry vision and frontal headache of three months’ duration accompanied by light unilateral galactorrhoea. The findings of the physical examination were: height, 169.5cm (standard deviation [SD], +1.1); weight, 53.3kg; body mass index (BMI), 19.29kg/m2 (SD, −0.79). The patient was at Tanner stage V of pubertal development with proportionate features. There was no galactorrhoea, hirsutism or acne. The complete blood count and blood chemistry panel were normal, with the most salient finding being the serum prolactin level (205.6ng/mL). Magnetic resonance imaging (MRI) revealed an enlarged pituitary gland with a superior border that was convex towards the midline and signal hyperintensity suggestive of subacute haemorrhage (Fig. 1). The pituitary gland extended into and obliterated the suprasellar cistern, exerting a mass effect on the optic chiasm. The ophthalmological examination evinced mild hyperopia, and the visual field test and eye fundus examination were normal. The patient was given a diagnosis of prolactinoma with subclinical apoplexy based on these findings, and started treatment with cabergoline at a dose of 0.25mg the first week, followed by a maintenance dose of 0.50mg a week. One month after treatment initiation, the follow-up MRI scan showed an adenoma measuring 10mm×8mm (Fig. 2), values that may have been overestimated due to haemorrhagic features, and the serum prolactin level was 12.6ng/mL. At present, the patient has regular menstrual periods, normal vision without headache and no galactorrhoea.
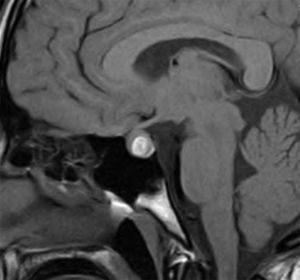
Case 2: male patient aged 14 years that was being followed up for obesity and tall height with advanced bone age. The assessment of the patient's headaches included performance of an MRI scan that revealed a 10mm×10mm nodule in the left region of the pituitary gland, with remodelling of the angle of the sella turcica with no extension to the cavernous sinus compatible with adenoma (at the threshold between microadenoma and macroadenoma). The patient did not present with vision changes or galactorrhoea. The findings of the physical examination were: height, 173.6cm (SD, +1.16); weight, 85.6kg; BMI, 28.4kg/m2 (SD, +3.3). The patient had predominantly abdominal obesity with adipomastia. The only abnormal finding in laboratory tests was an elevated prolactin level of 118ng/mL. Treatment with dopamine agonists was initiated at 0.50mg a week, given in 2 doses, to which the patient responded favourably (prolactin, 11.5mg/mL).
Hyperprolactinaemia secondary to a pituitary adenoma is a rare finding in the paediatric population. The prevalence of prolactinoma is 100 per one million inhabitants, accounting for fewer than two percent of all intracranial tumours.1 There is a wide variability in its main clinical features, which vary based on sex, tumour size and age of onset.2,3 We have presented two cases of prolactinoma in patients of both sexes with a similar age of onset and clinical features that are nearly opposite. In case 1, the patient presented with headache and vision changes and imaging findings compatible with haemorrhagic adenoma. Subclinical pituitary apoplexy in children and adolescents is rarely mentioned in the literature, and most of the evidence consists in the description of isolated cases.4 Patients may remain asymptomatic or have very mild symptoms compared to those of pituitary apoplexy. There is no correlation between prolactin levels and the duration or severity of symptoms. There is also no evidence of a relationship between tumour size and the presence of haemorrhagic processes.4 In children, development of subclinical pituitary apoplexy is more frequent due to the decreased susceptibility to infarction of the tumour and a greater resistance to haemorrhage than adults, and is probably underdiagnosed.5
As for treatment, cases of subclinical apoplexy, especially prolactin-producing adenomas, can be managed conservatively. Treatment with dopamine agonists can control prolactin levels and reduce tumour size significantly.4,5
In cases of hyperprolactinaemia secondary to prolactinoma, medication is recommended as the first-line treatment for both microadenomas and macroadenomas regardless of age.6 The primary goal of dopamine agonist therapy is to improve sex-gland and neurologic functioning. The followup requires close monitoring of the patient's clinical manifestations and blood chemistry, and treatment may be discontinued after two years if prolactin levels are no longer elevated and there is no visible tumour remnant on MRI.2,6 If treatment is discontinued, serum prolactin should be measured every three months in the first year and annually thereafter, and MRI performed if serum prolactin levels increased past the normal range.6
Please cite this article as: Mora Mendoza A, García-Cuartero B, Oyakawa Y, Castellanos RB. Prolactinomas en la población pediátrica. An Pediatr (Barc). 2016;85:158–159.