Atrial fibrillation (AF) is an exceptional arrhythmia in the pediatric age group in the absence of complex congenital heart defects or previous cardiac surgery. We present 2 cases of paroxysmal AF in childhood, both in patients without a known history of cardiac disease, triggered by intense physical activity and that responded well to treatment. We also reviewed the literature on this disease in the pediatric age group.
Case 1 corresponded to a male adolescent aged 14 years that presented to the emergency department with palpitations and a sensation of difficulty breathing with onset a few hours prior after performance of physical activity (martial arts, a sport with a high static component and a moderate dynamic component). He had no medical history of interest and was not receiving any ongoing pharmacological treatment. The father had idiopathic AF.
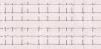
Several diagnostic tests were performed, among which the most relevant was an electrocardiogram (ECG) that showed an irregular rhythm with narrow QRS complexes and a heart rate of 80 beats per minute with multiple low-amplitude F-waves, compatible with AF (Fig. 1). The arterial blood pressure was 122/71mmHg. The body mass index (BMI) was under the 95th percentile. The results of blood chemistry tests were normal, with no abnormalities in electrolyte levels and negative results of drug testing in urine; thyroid hormone levels were normal. A Doppler ultrasound scan ruled out structural heart defects, revealing normal atria and ventricular function both in systole and diastole and absence of intracardiac thrombi. The scan detected the presence of persistent left superior vena cava with moderate dilatation of the coronary sinus, which was confirmed by a saline contrast study performed by injection of shaken physiological saline in the left cephalic vein.
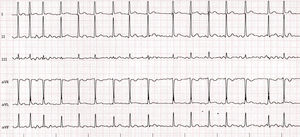
The patient was given a dose of oral flecainide (2.5mg/kg), which achieved restoration of the sinus rhythm. This was followed by initiation of maintenance therapy with flecainide.
At 12 months of follow-up the patient had experienced no recurrences, and the antiarrhythmic drug therapy was discontinued. A subsequent cardiac stress test revealed a normal heart rhythm and blood pressure, both at peak exertion and during recovery, with no associated vagal symptoms. The patient remained asymptomatic 9 months later.
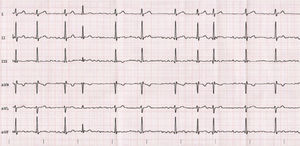
Case 2 corresponded to a male adolescent aged 17 years referred to the emergency department due to syncope following exertion (bodybuilding a sport with a high static component and a moderate dynamic component) that exhibited complete neurologic recovery in a few seconds with immediate development of palpitations and the sensation of tachycardia. The patient was put under observation with performance of a full ECG, which revealed atrial fibrillation with ventricular contractions occurring at 110–120 beats per minute (Fig. 2).
The patient was given an oral dose of 2.5mg/kg of flecainide, which achieved restoration of the sinus rhythm.
The physical examination revealed a mild systolic ejection murmur best heard over the aortic valve. The BMI was below the 95th percentile. The Doppler ultrasound scan revealed a bicuspid aortic valve with two raphes of mild severity, a disorder that had not been diagnosed previously. The atria had normal morphology and were not enlarged. There was no evidence of thrombi in the heart.
The patient had no personal or family history of interest and was not undergoing chronic pharmacological treatment. The urine drug test was negative and the levels of serum electrolytes and thyroid hormones were normal.
The patient remained under pharmacological treatment with flecainide for 12 months, without recurrence of arrhythmia at 5 months of follow-up.
Isolated atrial fibrillation is an infrequent arrhythmia in the pediatric population, especially in the absence of organic heart disease of a probably multifactorial etiology. Both of the cases we present here corresponded to a first episode of AF that was haemodynamically insignificant in patients with no known history of heart disease.
Persistent left superior vena cava, diagnosed in case 1, has been associated with the development of supraventricular arrhythmias, including AF. Radiofrequency catheter ablation of these connections can prevent their recurrence. Hsu et al. described 5 cases of AF where electrophysiology testing identified persistent left superior vena cava as the source arrhythmia.1,2
To our knowledge, an association between AF and bicuspid aortic valve, a defect detected in case 2, has not been previously reported, and therefore the coexistence of these 2 disorders could be coincidental and unrelated to the disease process.
Intense physical activity may cause electrical and structural changes in the atria that would promote the development of an episode of AF. In both our patients, AF was associated with physical activity. There is also evidence of an association between chest trauma with commotio cordis and AF.3
Cases of isolated familial AF have been reported in the literature in association with genetic mutations affecting multiple ion channels and circulating hormones such as atrial natriuretic peptide. However, the diagnostic yield of genetic testing for this type of arrhythmia is currently not known.4,5 In this regard, the presence of idiopathic AF in the father of case 1 may have increased the risk of AF in our patient. In addition, consumption of some recreational substances, such as cannabis, can trigger AF. In the cases presented here, we ruled out the consumption of arrhythmogenic substance use.
In a series of 1750 cases of isolated AF in children, the only risk factors identified were obesity with a BMI above the 95th percentile, male sex and age greater than 14 years.6
At present there is no consensus regarding the first-line antiarrhythmic drug for treatment of AF in the pediatric age group. However, drugs used to control heart rate (such as beta blockers) are the most widely used agents. In the 2 cases presented here, treatment with flecainide was chosen with the aim of achieving cardioversion. In cases refractory to pharmacotherapy, electrical cardioversion and radiofrequency ablation of the sources of atrial arrhythmia are effective alternatives.6
Lastly, the use of anticoagulant therapy was ruled out in both cases due to the low risk of thrombosis and the early recovery of the sinus rhythm. In any case, there are no guidelines providing the indication of prophylactic treatment for prevention of stroke in this population.
Please cite this article as: Roguera Sopena M, Sabidó Sánchez L, Villuendas Sabaté R, del Alcázar Muñoz R. Fibrilación auricular. A propósito de 2 casos. Arch Bronconeumol. 2020;92:47–49.