Congenital hypothyroidism (CH) is the most frequent preventable cause of intellectual disability in children. Early diagnosis and treatment of this disease prevent neurodevelopmental impairment. In recent years, there has been an increase the prevalence of CH, probably due to the increased survival of preterm infants.1
The diagnosis of CH starts with the detection of elevation of thyroid stimulating hormone (TSH) during neonatal screening, conducted 24–72h post birth, followed by imaging tests to determine the aetiology of this abnormality—thyroid scintigraphy (Tc99 and I123) and, in some cases, a cervical ultrasound scan.
In very small or very preterm newborns (weight<1500g or gestational age<32 weeks), delayed elevation of TSH is common, and thus CH cannot be detected in the first 48h post birth. Therefore, it is recommended that the screening be repeated in subsequent weeks in these patients, for which there is currently no standardised protocol in Spain. The European consensus guidelines recommend a second screening at 2 weeks post birth in preterm and very low birthweight newborns.2 This protocol has been applied in Andalusia since 2011, with the addition of a third screening in very preterm newborns at the time of hospital discharge.
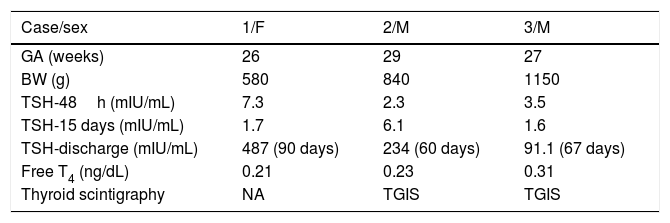
We present 3 clinical cases that were very similar (Table 1). All of them concerned very preterm newborns that had normal levels of TSH in the neonatal screenings performed at 48h and 2 weeks post birth. Detection of elevated TSH and, consequently, initiation of replacement therapy occurred between 60 and 90 days post birth (at the time of discharge). In every case, the level of free thyroxine (T4) was far below normal. The antithyroid antibodies test was negative, and in 2 cases a thyroid scan with Tc99 revealed a thyroid gland in situ.
Clinical and laboratory data of very preterm newborns with a discharge diagnosis of congenital hypothyroidism detected by neonatal screening.
| Case/sex | 1/F | 2/M | 3/M |
|---|---|---|---|
| GA (weeks) | 26 | 29 | 27 |
| BW (g) | 580 | 840 | 1150 |
| TSH-48h (mIU/mL) | 7.3 | 2.3 | 3.5 |
| TSH-15 days (mIU/mL) | 1.7 | 6.1 | 1.6 |
| TSH-discharge (mIU/mL) | 487 (90 days) | 234 (60 days) | 91.1 (67 days) |
| Free T4 (ng/dL) | 0.21 | 0.23 | 0.31 |
| Thyroid scintigraphy | NA | TGIS | TGIS |
BW, birth weight; F, female; GA, gestational age; M, male; NA, not available; TGIS, thyroid gland in situ; TSH, thyroid stimulating hormone; T4, thyroxine.
The neonatal records did not document the administration of iodine or any other drugs that may have interfered with the level of TSH or its measurement.
Although given the time elapsed since birth we were unable to analyse the persistence of hypothyroidism, the diagnosis was delayed in all 3 cases and there is a possibility of future neurodevelopmental impairment.
The approximate prevalence of CH is of 1 per 2240 births, with delayed elevation of TSH in 1 out of 295 cases in preterm newborns (1000–1500g) and in 1 out of 58 cases in newborns with birth weights of less than 1000g.3
In preterm infants, CH has a multifactorial aetiology that involves the immaturity of the hypothalamic-pituitary-thyroid axis, a reduced synthesis of thyroxine-binding globulin by the liver, non-thyroid diseases associated with complications commonly found in preterm infants (respiratory distress, intraventricular haemorrhage and necrotising enterocolitis), drugs that suppress the production of TSH (dopamine and corticosteroids) and low iodine intake.4
There is evidence that the delayed elevation of TSH occurs between weeks 2 and 6 post birth3 and that the delay is associated with low birth weight, small size for gestational age and/or multiple gestation, a 5-min Apgar score of less than 5 and duration of positive-pressure ventilation.5
Given the evidence on the delayed elevation of TSH in preterm infants, the authors of some studies have already recommended repetition of neonatal screening. Thus, Woo et al. reported performing the initial screening between days 2 and 5 post birth and repeating it in weeks 2, 6 and 10 or once the infant reaches a weight of 1500g.3 They also recommend repeating the screening in infants weighing more than 1500g if they remain critically ill. At present, there is no agreement on whether low thyroid hormone levels may have an impact on morbidity and mortality in preterm infants with transient hypothyroxinaemia.6
The recommendations of the Working Group on the Thyroid of the Sociedad Española de Endocrinología Pediátrica (Spanish Society of Paediatric Endocrinology, www.seep.es), published in 2015, stipulate that in newborns weighing less than 1500g, in addition to neonatal screening, the serum level of TSH should be measured at 15 days post birth and at discharge. However, as demonstrated by the cases presented here, this may not be sufficient, especially if the hospitalisation is prolonged.
In light of all of the above, we propose performance of at least 4 measurements of serum TSH levels in preterm newborns with birth weights of less than 1500g for detection of CH: at 24–72h, at 15 days and at 6 weeks post birth, and once the infant reaches a weight of 1500g. In our opinion, it would be optimal to implement this schedule of tests in the framework of neonatal screening programmes.
Please cite this article as: Yahyaoui R, Jiménez-Machado R, López Siguero JP. Propuesta de pauta en el cribado neonatal de hipotiroidismo congénito en grandes prematuros. Arch Bronconeumol. 2020;92:46–47.