To describe the characteristics of paediatric patients with suspected poisoning treated by advanced life support (ALS) units, and to evaluate quality indicators (QI) for the prehospital emergency care of these patients.
MethodA one-year observational study of patients under 18 years of age exposed to poisoning and treated by an ALS unit of the Medical Emergency System in Catalonia. Severe clinical criteria were defined, with 8 QI being evaluated for prehospital emergency care of poisoned paediatric patients.
ResultsThe study included a total of 254 patients, with a median age of 14 years old (p25-75=7–16), with intentional poisoning in 50.8% of cases. The most frequently involved toxic agent was carbon monoxide (CO) (33.8%). Poisoning was found in 48.8% of those patients, being serious in 16.5%. Intentionally (OR 5.1; 95% CI: 1.9–13.8) and knowledge of the time of exposure (OD 3.1; 95% CI: 1.3–7.3) were independent risk factors associated with the appearance of severe clinical symptoms. Five QI did not reach the quality standard and included, availability of specific clinical guidelines, activated charcoal administration in selected patients, oxygen therapy administration at maximum possible concentration in carbon monoxide poisoning, electrocardiographic assessment in patients exposed to cardiotoxic substances, and recording of the minimum data set.
ConclusionsPaediatric patients attended by ALS units showed specific characteristics, highlighting the involvement of CO and adolescents with voluntary poisoning. The QI assessment was useful to detect weak points in the quality of care of these patients and to develop strategies for improvement.
Describir las características de los pacientes pediátricos con sospecha de intoxicación atendidos por unidades de soporte vital avanzado (SVA) y evaluar los indicadores de calidad (IC) para la atención urgente prehospitalaria de estos pacientes.
MétodoEstudio observacional de los pacientes menores de 18 años con exposición a tóxicos, que fueron atendidos por una unidad de SVA del Sistema de Emergencias Médicas en Cataluña, durante un año. Se definieron criterios de clínica grave. Se evaluaron 8IC para la atención urgente prehospitalaria de los pacientes pediátricos intoxicados.
ResultadosSe incluyó a 254 pacientes. La edad mediana fue de 14 años (p25-75=7-16), con exposición intencionada en el 50,8% de los casos. El tóxico más frecuentemente implicado fue el monóxido de carbono (CO) (33,8%). Presentó clínica de toxicidad el 48,8%, siendo grave en el 16,5%. La intencionalidad (OR 5,1; intervalo de confianza del 95%: 1,9-13,8) y el desconocimiento del tiempo transcurrido desde el contacto (OR 3,1; intervalo de confianza del 95%: 1,3-7,3) fueron factores de riesgo independientes asociados a clínica grave. Cinco IC no alcanzaron el estándar de calidad: disponibilidad de guías de actuación específicas, administración de carbón activado en pacientes seleccionados, aplicación de oxigenoterapia a la máxima concentración posible en intoxicación por CO, valoración electrocardiográfica en pacientes expuestos a sustancias cardiotóxicas y registro del conjunto mínimo de datos.
ConclusionesLos pacientes pediátricos expuestos a tóxicos y atendidos por unidades SVA presentan características propias. Destacan la implicación del CO y de los adolescentes con intoxicaciones voluntarias. La evaluación de los IC ha sido útil para detectar puntos débiles en la calidad asistencial de estos pacientes y desarrollar estrategias de mejora.
In the paediatric age group, poisonings are heterogeneous and potentially severe events. The management of these patients must be based on stabilisation and supportive care measures, as well as initiation of specific treatment as early as possible, as its effectiveness often depends on timing.1
According to the Working Group on Poisoning of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine, SEUP), 17% de of patients seeking care for suspected poisoning in paediatric emergency departments (PEDs) are transported in an ambulance.2 When Advanced Life Support (ALS) unit is in charge of transport, there is an opportunity to initiate specific treatment early. However, in most cases prehospital emergency care is provided by staff not specialised in paediatrics, which can result in uncertainty as to the correct management of the poisoned patient.
Few epidemiological and clinical studies have been published on the subject of the prehospital management of patients requiring care for poisoning and, until the study presented here, none have analysed the severity of poisoning in these patients or the characteristics and quality of the care received.
Previous studies have demonstrated the usefulness of applying quality indicators (QIs) in paediatric poisonings to assess and monitor the quality of care offered poisoned patients managed in PEDs in Spain.3–5 The Working Group on Toxicology of the Societat Catalana de Medicina d’Urgències i Emergències (SoCMUE), in cooperation with the Working Group on Poisoning of the SEUP, adapted the QIs used in paediatric poisonings for application to the prehospital emergency care of these patients. These QIs have been endorsed by the SEUP and the Fundación Española de Toxicología Clínica (Spanish Foundation of Clinical Toxicology) as scientifically sound.6
The aim of our study was to describe the characteristics of paediatric patients with suspected poisoning managed by ALS units in Catalonia and assess the QIs applied to prehospital emergency care.
MethodsWe conducted a descriptive and observational study of patients aged <18 years exposed to poisons managed by ALS units of the Medical Emergency System (Sistema de Emergencias Médicas, SEM) in the entire region of Catalonia between June 1, 2016 and May 31, 2017. We excluded interhospital transfers. The ALS units of the SEM may consist of an emergency medical technician and a nurse (ALSn), a technician with a nurse and a physician (ALSp) or a technician and a physician (rapid intervention vehicle, RIV).
For each patient, we collected epidemiological and clinical data through the review of the care report of the SEM. The epidemiological variables under study included age, sex, cause of poisoning, involved substance(s), type of resource dispatched (ALSn, ALSp or RIV), setting of intervention and time elapsed from exposure. The clinical characteristics under study included the presence of manifestations of poisoning or severe manifestations, performance of electrocardiography (ECG) or assessment of the tracings visualised in the cardiac monitor and treatment. Within the latter variable, we differentiated between administration of activated charcoal (AC), oxygen therapy (as an antidote or for supportive care), administration of other antidotes, fluid therapy and other treatments. We also collected data on patient destination after prehospital care (discharge or transport to hospital), pre-arrival notification to the receiving emergency department (ED) and deaths during prehospital care.
Based on grades 2 and 3 of the Poisoning Severity Score,7 we defined severity as the presence of any of the following: moderate to severe decrease in level of consciousness (with or without appropriate response to pain), seizures, agitation, hypotension or poor peripheral perfusion, hypertensive crisis, arrhythmia, moderate to severe respiratory insufficiency, respiratory depression or hypoxaemia.
We classified patients by age into 0–5 years (infants and young children), 6–11 years (school-age children) and 12–17 years (adolescents). We compared patient characteristics by age group, type of resource dispatched and the presence of severe manifestations. In the comparison by type of resource dispatched, we took into account whether the units sent amounted or not to a full care team comprising a medical emergency technician, nurse and physician (ALSp or ALSn+RIV vs ALSn or RIV).
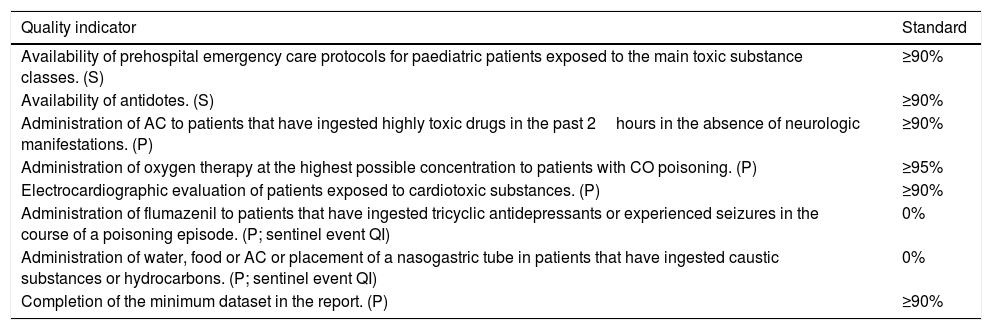
We evaluated 8 QIs of prehospital emergency care of poisoned paediatric patients (Table 1). We evaluated structural quality indicators by consulting with the documentation manager and assessing the drug stocks of the SEM. We evaluated process QIs by reviewing the collected clinical data. We established a minimum of 5 cases to analyse the QIs applicable to specific patient subgroups8 with the exception of sentinel event QI, which assess for the presence of serious events that should never occur. We compared the results of process QIs based on the dispatched resource.
Quality indicators of prehospital emergency care in poisoned paediatric patients.
| Quality indicator | Standard |
|---|---|
| Availability of prehospital emergency care protocols for paediatric patients exposed to the main toxic substance classes. (S) | ≥90% |
| Availability of antidotes. (S) | ≥90% |
| Administration of AC to patients that have ingested highly toxic drugs in the past 2hours in the absence of neurologic manifestations. (P) | ≥90% |
| Administration of oxygen therapy at the highest possible concentration to patients with CO poisoning. (P) | ≥95% |
| Electrocardiographic evaluation of patients exposed to cardiotoxic substances. (P) | ≥90% |
| Administration of flumazenil to patients that have ingested tricyclic antidepressants or experienced seizures in the course of a poisoning episode. (P; sentinel event QI) | 0% |
| Administration of water, food or AC or placement of a nasogastric tube in patients that have ingested caustic substances or hydrocarbons. (P; sentinel event QI) | 0% |
| Completion of the minimum dataset in the report. (P) | ≥90% |
AC, activated charcoal; P, process quality indicator; QI, quality indicator; S, structural quality indicator.
We analysed the data using the software SPSS version 24.0 for Windows, carrying out tests to assess the distribution of the data (Kolmogorov–Smirnov) and to compare quantitative data (Mann–Whitney U test) and qualitative data (chi square test, contingency tables, Fisher exact test). We used multivariate logistic regression to identify potential factors associated with the development of severe manifestations, calculating the corresponding 95% confidence intervals. We considered p-values of <.05 statistically significant. The study was approved by the Clinical Board of the SEM and the Ethics and Research Committee of the Hospital Clínic of Barcelona.
ResultsThe study included 254 patients exposed to toxic substances out of a total of 8319 patients aged <18 years managed by ALS units in the study period (3.1%). The median age was 14 years (interquartile range, 7–16). The exposure to the potentially toxic substance was unintentional in 126 cases (49.6%), while the substance was used for recreational purposes in 74 cases (29.1%) and with suicidal intent in 44 (17.3%). In 10 patients (3.9%) exposure involved the voluntary consumption of repeated doses of the substance for symptom control (pain or anxiety).
The most frequently involved toxic substance was carbon monoxide (CO), resulting from the incomplete combustion of gas used in the household or inhalation of smoke from a fire (n=86; 33.8%), followed by ethanol (n=66; 26%) and psychotropic drugs (n=41; 16.1%).
Symptoms of poisoning were present in 124 patients (48.8%) and severe in 42 (16.5%). The treatments given were oxygen therapy (n=82; 32.3%), fluid therapy (n=46; 18.1%) and administration of antidotes (n=17; 6.7%), AC (n=16; 6.3%;) and nebulised drugs (n=11; 4.3%). The antidotes given were flumazenil in 17 cases (6.7%) and naloxone in 6 (2.3%). A total of 225 patients (88.6%) were transported to a hospital, with pre-arrival notification in 21 cases (9.3%). All patients that were not transported to an ED reported low-risk exposures, were stable and were accompanied by their parents. There were no deaths.
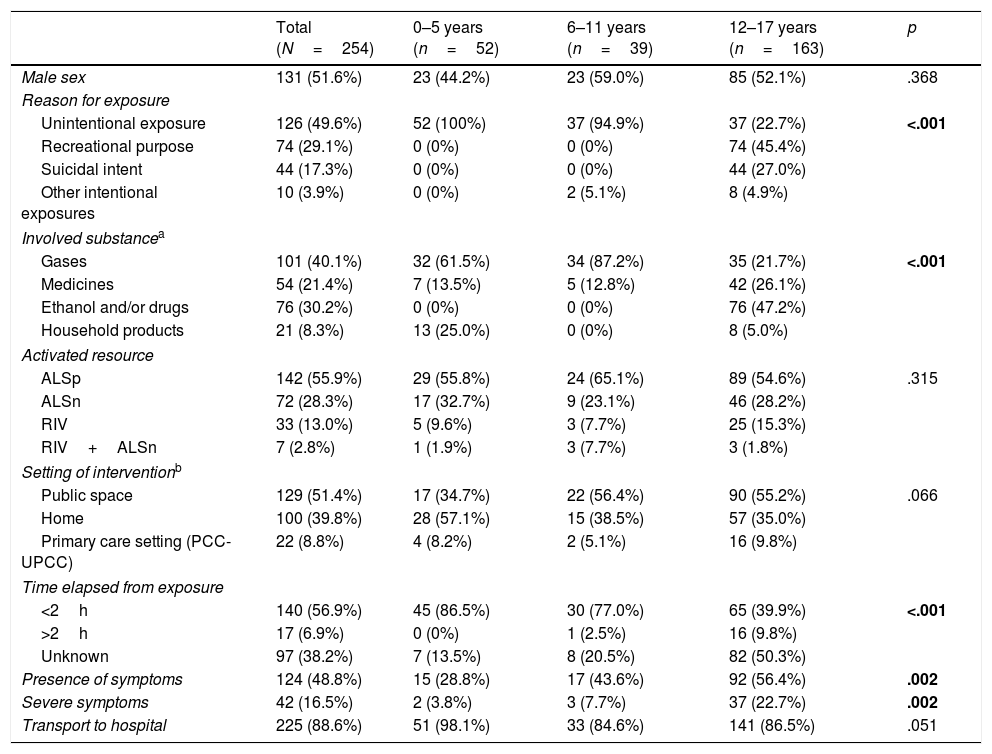
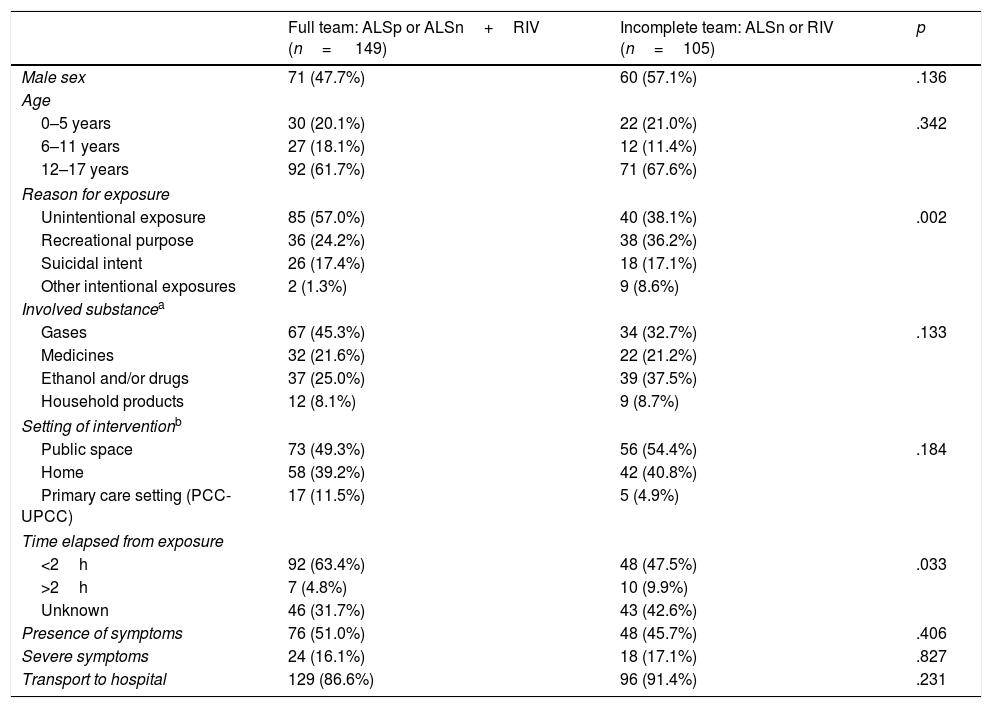
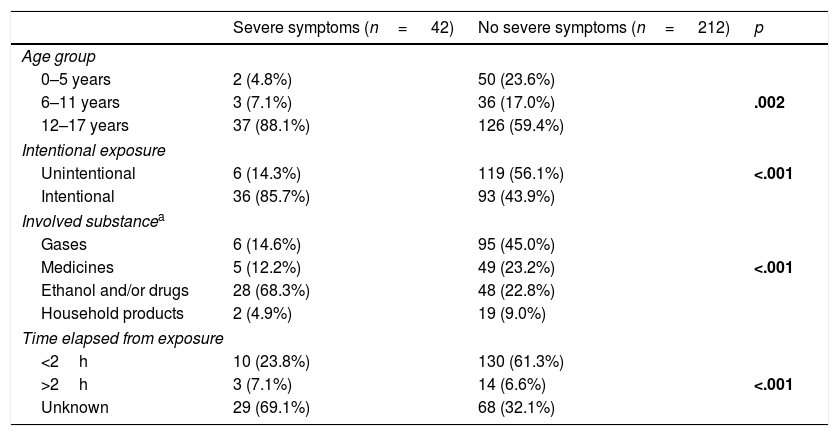
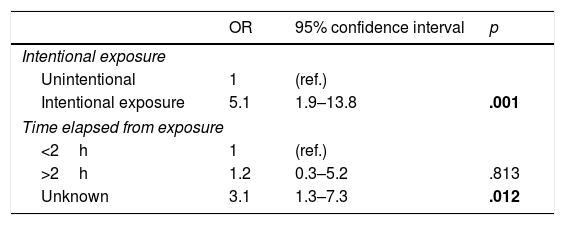
Table 2 summarises the characteristics of the patients compared by age group. Table 3 compares the characteristics of the patients by type of resource dispatched and Table 4 the association between epidemiological characteristics and the presence of severe symptoms. The multivariate analysis revealed that intentional exposure (OR, 5.1; 95% confidence interval [CI], 1.9–13.8) and not knowing the time elapsed from the exposure (OR, 3.1; 95% CI, 1.3–7.3) were independent risk factors associated with severe poisoning (Table 5).
Characteristics of patients aged <18 years managed by ALS units of the SEM after exposure to toxic substances. Comparison by age group.
| Total (N=254) | 0–5 years (n=52) | 6–11 years (n=39) | 12–17 years (n=163) | p | |
|---|---|---|---|---|---|
| Male sex | 131 (51.6%) | 23 (44.2%) | 23 (59.0%) | 85 (52.1%) | .368 |
| Reason for exposure | |||||
| Unintentional exposure | 126 (49.6%) | 52 (100%) | 37 (94.9%) | 37 (22.7%) | <.001 |
| Recreational purpose | 74 (29.1%) | 0 (0%) | 0 (0%) | 74 (45.4%) | |
| Suicidal intent | 44 (17.3%) | 0 (0%) | 0 (0%) | 44 (27.0%) | |
| Other intentional exposures | 10 (3.9%) | 0 (0%) | 2 (5.1%) | 8 (4.9%) | |
| Involved substancea | |||||
| Gases | 101 (40.1%) | 32 (61.5%) | 34 (87.2%) | 35 (21.7%) | <.001 |
| Medicines | 54 (21.4%) | 7 (13.5%) | 5 (12.8%) | 42 (26.1%) | |
| Ethanol and/or drugs | 76 (30.2%) | 0 (0%) | 0 (0%) | 76 (47.2%) | |
| Household products | 21 (8.3%) | 13 (25.0%) | 0 (0%) | 8 (5.0%) | |
| Activated resource | |||||
| ALSp | 142 (55.9%) | 29 (55.8%) | 24 (65.1%) | 89 (54.6%) | .315 |
| ALSn | 72 (28.3%) | 17 (32.7%) | 9 (23.1%) | 46 (28.2%) | |
| RIV | 33 (13.0%) | 5 (9.6%) | 3 (7.7%) | 25 (15.3%) | |
| RIV+ALSn | 7 (2.8%) | 1 (1.9%) | 3 (7.7%) | 3 (1.8%) | |
| Setting of interventionb | |||||
| Public space | 129 (51.4%) | 17 (34.7%) | 22 (56.4%) | 90 (55.2%) | .066 |
| Home | 100 (39.8%) | 28 (57.1%) | 15 (38.5%) | 57 (35.0%) | |
| Primary care setting (PCC-UPCC) | 22 (8.8%) | 4 (8.2%) | 2 (5.1%) | 16 (9.8%) | |
| Time elapsed from exposure | |||||
| <2h | 140 (56.9%) | 45 (86.5%) | 30 (77.0%) | 65 (39.9%) | <.001 |
| >2h | 17 (6.9%) | 0 (0%) | 1 (2.5%) | 16 (9.8%) | |
| Unknown | 97 (38.2%) | 7 (13.5%) | 8 (20.5%) | 82 (50.3%) | |
| Presence of symptoms | 124 (48.8%) | 15 (28.8%) | 17 (43.6%) | 92 (56.4%) | .002 |
| Severe symptoms | 42 (16.5%) | 2 (3.8%) | 3 (7.7%) | 37 (22.7%) | .002 |
| Transport to hospital | 225 (88.6%) | 51 (98.1%) | 33 (84.6%) | 141 (86.5%) | .051 |
ALS, advanced life support (ALSn: medical emergency technician+nurse; ALSp: technician+physician+nurse; RIV: technician+physician); CO, carbon monoxide; PCC, primary care centre; SEM, Medical Emergency System.
Characteristics of patients compared based on the type of activated resource.
| Full team: ALSp or ALSn+RIV (n= 149) | Incomplete team: ALSn or RIV (n=105) | p | |
|---|---|---|---|
| Male sex | 71 (47.7%) | 60 (57.1%) | .136 |
| Age | |||
| 0–5 years | 30 (20.1%) | 22 (21.0%) | .342 |
| 6–11 years | 27 (18.1%) | 12 (11.4%) | |
| 12–17 years | 92 (61.7%) | 71 (67.6%) | |
| Reason for exposure | |||
| Unintentional exposure | 85 (57.0%) | 40 (38.1%) | .002 |
| Recreational purpose | 36 (24.2%) | 38 (36.2%) | |
| Suicidal intent | 26 (17.4%) | 18 (17.1%) | |
| Other intentional exposures | 2 (1.3%) | 9 (8.6%) | |
| Involved substancea | |||
| Gases | 67 (45.3%) | 34 (32.7%) | .133 |
| Medicines | 32 (21.6%) | 22 (21.2%) | |
| Ethanol and/or drugs | 37 (25.0%) | 39 (37.5%) | |
| Household products | 12 (8.1%) | 9 (8.7%) | |
| Setting of interventionb | |||
| Public space | 73 (49.3%) | 56 (54.4%) | .184 |
| Home | 58 (39.2%) | 42 (40.8%) | |
| Primary care setting (PCC-UPCC) | 17 (11.5%) | 5 (4.9%) | |
| Time elapsed from exposure | |||
| <2h | 92 (63.4%) | 48 (47.5%) | .033 |
| >2h | 7 (4.8%) | 10 (9.9%) | |
| Unknown | 46 (31.7%) | 43 (42.6%) | |
| Presence of symptoms | 76 (51.0%) | 48 (45.7%) | .406 |
| Severe symptoms | 24 (16.1%) | 18 (17.1%) | .827 |
| Transport to hospital | 129 (86.6%) | 96 (91.4%) | .231 |
ALS, advanced life support (ALSn: medical emergency technician+nurse; ALSp: technician+physician+nurse; RIV: technician+physician); CO, carbon monoxide; PCC, primary care centre; SEM, Medical Emergency System.
Comparison of epidemiological characteristics in patients with and without severe symptoms.
| Severe symptoms (n= 42) | No severe symptoms (n= 212) | p | |
|---|---|---|---|
| Age group | |||
| 0–5 years | 2 (4.8%) | 50 (23.6%) | |
| 6–11 years | 3 (7.1%) | 36 (17.0%) | .002 |
| 12–17 years | 37 (88.1%) | 126 (59.4%) | |
| Intentional exposure | |||
| Unintentional | 6 (14.3%) | 119 (56.1%) | <.001 |
| Intentional | 36 (85.7%) | 93 (43.9%) | |
| Involved substancea | |||
| Gases | 6 (14.6%) | 95 (45.0%) | |
| Medicines | 5 (12.2%) | 49 (23.2%) | <.001 |
| Ethanol and/or drugs | 28 (68.3%) | 48 (22.8%) | |
| Household products | 2 (4.9%) | 19 (9.0%) | |
| Time elapsed from exposure | |||
| <2h | 10 (23.8%) | 130 (61.3%) | |
| >2h | 3 (7.1%) | 14 (6.6%) | <.001 |
| Unknown | 29 (69.1%) | 68 (32.1%) | |
Epidemiological characteristics associated with severe poisoning based on the multivariate logistic regression model.
| OR | 95% confidence interval | p | |
|---|---|---|---|
| Intentional exposure | |||
| Unintentional | 1 | (ref.) | |
| Intentional exposure | 5.1 | 1.9–13.8 | .001 |
| Time elapsed from exposure | |||
| <2h | 1 | (ref.) | |
| >2h | 1.2 | 0.3–5.2 | .813 |
| Unknown | 3.1 | 1.3–7.3 | .012 |
OR, odds ratio.
Statistically significant p-values are presented in boldface.
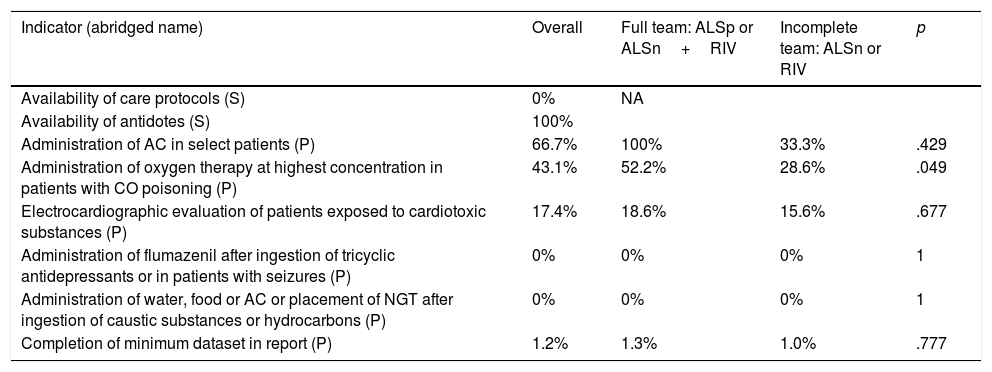
The quality standard was met for the “antidote availability” QI and the 2 sentinel event QIs, “administration de flumazenil to patients that have consumed tricyclic antidepressants or had seizures in the course of a poisoning episode” and “administration of water, food or AC or placement of a nasogastric tube in patients that had ingested caustic agents or hydrocarbons”.
The health care staff of the SEM did not have access to a specific protocol for the prehospital care of poisoned paediatric patients.
Activated charcoal was given to 4 out of 6 patients that had ingested a highly toxic drug in the past 2h in the absence of neurologic manifestations (66.7%).
Of the 72 patients exposed to CO and transported to a health care facility, 31 (43.1%) received oxygen therapy at the highest possible concentration (non-rebreather face mask or, in intubated patients, a FiO2 of 1). In 21 patients, oxygen was delivered through a Venturi mask or nasal prongs, achieving FiO2 values of <0.5, while the use of any form of oxygen therapy was not documented in the reports of another 20 patients.
The reports documented performance of electrocardiographic evaluation in 20 of the 115 patients exposed to cardiotoxic substances (17.4%). In 86, the involved agent was CO, and in this subset electrocardiographic changes were assessed in 6 patients.
Out of the 254 patients managed after exposure to a toxic substance, the minimum dataset (conjunto mínimo de datos [CMD]) established for discharge reports was collected in 3 cases (1.2%). The variables of the CMD documented least frequently were the weight (14 patients; 5.5%) and body temperature (36; 14.2%). The heart rate was recorded in 210 (82.7%), the respiratory rate in 142 (55.9%), the blood pressure in 177 (69.7%) and the blood glucose level (in case of altered level of consciousness) in 41 out of 62 patients (66.1%). The age, type of toxic substance, dose, time elapsed from exposure and route of exposure were documented in more than 90% of the patients. Table 6 presents the degree of compliance with QIs, overall and by type of resource dispatched.
Results found in the evaluation of quality indicators. Comparison of performance in quality indicators based on the type of resource activated.
| Indicator (abridged name) | Overall | Full team: ALSp or ALSn+RIV | Incomplete team: ALSn or RIV | p |
|---|---|---|---|---|
| Availability of care protocols (S) | 0% | NA | ||
| Availability of antidotes (S) | 100% | |||
| Administration of AC in select patients (P) | 66.7% | 100% | 33.3% | .429 |
| Administration of oxygen therapy at highest concentration in patients with CO poisoning (P) | 43.1% | 52.2% | 28.6% | .049 |
| Electrocardiographic evaluation of patients exposed to cardiotoxic substances (P) | 17.4% | 18.6% | 15.6% | .677 |
| Administration of flumazenil after ingestion of tricyclic antidepressants or in patients with seizures (P) | 0% | 0% | 0% | 1 |
| Administration of water, food or AC or placement of NGT after ingestion of caustic substances or hydrocarbons (P) | 0% | 0% | 0% | 1 |
| Completion of minimum dataset in report (P) | 1.2% | 1.3% | 1.0% | .777 |
AC, activated charcoal; CO, carbon monoxide; ALS, advanced life support (ALSn: medical emergency technician+nurse; ALSp: technician+physician+nurse; RIV: technician+physician); NA, not applicable; NGT, nasogastric tube; P, process quality indicator; S, structural quality indicator.
Statistically significant p-values are presented in boldface.
Poisonings in patients aged <18 years managed by the ALS units of the SEM in Catalonia have clearly distinct epidemiological characteristics compared to those episodes managed in PEDs.4,9 Adolescents amounted to 2/3 of the sample and, in more than half of cases, the exposure was intentional. In addition, CO was the substance involved most frequently. In opposition, according to the Working Group on Poisoning of the SEUP, when it comes to patients seeking care in Spanish PEDs after exposure to poisons, 70% are aged <5 years, exposure is unintentional in 65% of cases, and drugs are the substances involved most frequently (56%).9 In line with our findings, Salazar et al. demonstrated that among all patients exposed to toxic substances, patients that used substances with recreational purposes, inhaled CO or consume the substance with suicidal intent were those that contacted the SEM most frequently before seeking care in a PED.2
Exposure to CO has been reported as corresponding to a small percentage of patients seeking care in a PED for suspected poisoning (3.5–4.5%),10,11 whereas in our study, 33.8% of the patients had been exposed to this substance. These differences could be explained in part by the more frequent use of ambulance transport in this type of poisoning.2 In addition, a study conducted by the Working Group on Poisoning of the SEUP found that Catalonia is the autonomous region with the highest proportion of CO-related cases out of the total visits made to PEDs for suspected poisoning (7.6% compared to 3.1% in the rest of Spain).11 Another aspect that needs to be taken into account is that in many instances, CO-related cases involved multiple exposures, affecting an entire family or a group of individuals, so it is possible for units of the SEM to manage several children or adolescents in a single dispatch.
While we only analysed cases of patients managed by ALS units, fewer than half had symptoms of poisonings. This fact is related to the promptness with which caregivers consult with medical services when a child is exposed to a toxic substance, often before developing symptoms, and to the potential severity of the exposure. This factor was even more salient when we compared different age groups. Infants and children aged up to 5 years received care sooner after the exposure, and a lower proportion of them experienced severe symptoms compared to school-aged children and adolescents. However, we found a tendency towards taking them to hospital more frequently. The increased susceptibility of younger children to poisoning upon exposure to certain substances and a tendency of health care staff not specialised in paediatrics to protect younger patients may account for these findings. On the other hand, the differences we found in the reason for exposure and the involved substances are consistent with those previously described in poisoned paediatric patients managed in PEDs and are related to the risk behaviours characteristic of adolescence.9,10
A salient finding in our study was the unintentional poisonings and cases with exposure within the past 2h were managed more frequently by a full team, whereas the presence of symptoms or severe symptoms had no impact on the type of resource dispatched. As we said above, fear of the sudden onset of severe toxicity in an initially stable child may explain this finding. Patients in whom exposure was intentional with suicidal intent or for recreational purposes that required care from the SEM were usually managed at a point where symptoms had developed, mainly with altered level of consciousness, and were unable to provide specific information on the timing of the exposure. These situations are similar to those found in poisoning cases in adults, with which the prehospital care staff is very familiar, which may also explain these findings.
When it came to the evaluation of QIs, we found some weaknesses in the prehospital emergency care of poisoned paediatric patients. The absence of specific protocols is probably the reason in some cases, so their development and implementation is a key opportunity for improvement.
The position statements of the European Association of Poisons Centres and Clinical Toxicologists and the American Academy of Clinical Toxicology conclude that the gold standard for gut decontamination is administration of AC and that this measure is most effective when administered within 1 hour from ingestion,12,13 meaning that AC should be administered as soon as possible. Previous studies have demonstrated that its administration by medical emergency teams to select patients is safe and does not delay arrival to the ED.14,15 In our sample, AC was not given to 1/3 of eligible patients, missing the window for early administration of a simple and low-risk treatment.
Oxygen is a safe and accessible antidote for CO poisoning that must be administered as soon as possible.16–18 However, its administration was documented in less than half of the patients exposed to CO and transported to a hospital. Ferrés-Padró et al. recently reported difficulties in achieving the quality standard for this indicator in the adult population.19 In our study, we also found that participation of a full medical team (technician+physician+nurse) contributed to improving the quality of the care delivered to these patients, with more appropriate use of oxygen.
In paediatric patients exposed to cardiotoxic substances, it is important to assess for electrocardiographic abnormalities early on either by performance of ECG or evaluation of the tracings in the cardiac monitor. In our study, this was only done in 17.4% of patients exposed to cardiotoxic substances. An analysis of these cases showed that the substance involved most frequently was CO, and that in this subgroup electrocardiographic assessment was even less frequent (7%), which suggests that CO is erroneously considered to not be cardiotoxic in children.20–22 According to data published by Ferrés-Padró et al., an ECG was performed in 31.8% of adults managed by ALS units exposed to CO.19
To improve the quality of care in both adult and paediatric patients with CO poisoning, the Working Group on Toxicology of the SoCMUE has participated in the development of a consensus protocol with the Fire Department, the SEM and the Hyperbaric Medicine Units of Catalonia for the initial management of patients intoxicated by fire smoke, CO and hydrogen cyanide. This protocol has been disseminated recently and is now available to hospital and prehospital care teams.23
We found the worst performance in the QI pertaining to the documentation of the minimum dataset (CMD) in the care report summary. Probably because it has no direct impact on the patient, this is the area of care quality that is usually found to be most deficient. A study by Giménez et al. found that the information of the CMD was only completed in the discharge summary of 1.9% of poisoned patients managed in a PED,4 although this outcome was improved to up to 51% with the introduction of corrective measures (a poisoned patient checklist and a specific history-taking form in the electronic health record system).5 A study by Nogué et al. found that the CMD was completed in 7.2% of patients, with no significant difference after performance of training sessions on the subject.8
We ought to highlight that of all the variables included in the CMD, those documented least frequently were the body weight and the body temperature. Knowing the approximate body weight is essential in children for calculation of the required doses of medication, and changes in body temperature may be indicative of the development of toxic effects or complications of poisoning. On the other hand, the heart rate and respiratory rate were documented more frequently compared to the hospital setting and the care of adult patients,4,5,8,19 which evinces a concern to correctly assess haemodynamic and respiratory stability in children. Nevertheless, these records need to be improved, as documentation did not reach the standard of 90% for any of the variables included in the CMD.
Kerner et al. demonstrated that the use of checklists improves the quality of prehospital emergency care and is generally well received by health care staff. Specifically, they found increased documentation in the care summaries, including documentation of ECG use and increased adherence to clinical practice guidelines.24 The development of a simple checklist for the care of poisoned patients by ALS units of the SEM could, therefore, be a useful corrective measure. On the other hand, we ought to highlight that the standards for the 2 sentinel event QIs included in the study were met, which indicates that situations involving a high risk of iatrogenic harm were avoided.25,26
Another finding worth highlighting is that pre-arrival notification was only given to the receiving ED in 10% of cases. There is previous evidence that, on the one hand, the time elapsed between arrival of the patient to the ED and initiation of emergency care and gut decontamination are far from achieving the established standards,4,5,8 and, on the other, that pre-arrival notification expedites both.27 Therefore, the development of a protocol for activation of SEM teams including systematic notification to the receiving ED and of specific care protocols for the poisoned paediatric patient are quality improvement strategies that can be implemented at the prehospital as well as hospital care levels. Such an activation protocol has already been developed in collaboration with the Working Group on Toxicology of the SoCMUE.
There are limitations to this study. The retrospective collection of clinical data from the care report summaries of the SEM involve a loss of information that may have contributed to poorer outcomes in some quality indicators. For instance, there was no documentation of oxygen having been given to 20% of patients exposed to CO, but it is possible that oxygen was administered, and the intervention not recorded. In addition, we only analysed cases of patients managed by ALS units of the SEM in Catalonia, and therefore our findings cannot be extrapolated to other types of prehospital emergency care.
Our study allowed us to define the characteristics of patients aged <18 years managed by ALS units of the SEM following exposure to toxic substances in Catalonia. One salient finding was the protective attitude towards younger children, with engagement of a full emergency team in episodes of unintentional poisoning with recent exposure even though the most severe cases corresponded to intentional exposure and patients in whom the timing of exposure was unknown. The evaluation of QIs was useful for the detection of weak areas in the quality of care provided to these patients and for identifying opportunities for improvement.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez-Sánchez L, Ferrés-Padró V, Martínez-Millán D, Fernández-Calabria C, Amigó-Tadín M, Jiménez-Fàbrega FX, et al. Atención prehospitalaria urgente de los pacientes pediátricos expuestos a tóxicos: características epidemiológico-clínicas y evaluación de la calidad asistencial. An Pediatr (Barc). 2020;92:37–45.
Previous presentations: This study was presented at the 23rd Meeting of the Sociedad Española de Urgencias de Pediatría, April 2018, Sitges, Spain, and at the XXII Jornadas Nacionales de Toxicología Clínica, October 2018, Cordoba, Spain.