At present, there are few validated scoring tests for assessing acute bronchiolitis (AB) severity, and limited information on their test power. The aim of the present study is to evaluate the validity of an acute bronchiolitis severity score (ABSS) to help in deciding PICU admission.
Patients and methodProspective, descriptive, observational study of previously healthy infants under 1 year of age with AB, where the ABSS was used to compare severity as regards the need for PICU admission. The sample size was estimated as at least 175 patients. The research team was trained in the use of ABSS. All patients in the study were evaluated with ABSS daily, as well as in the case of clinical deterioration. The initial and maximum ABSS scores were contrasted to the need for PICU admission. A receiver operative curve was constructed, and the area under the curve was calculated, and the optimum point of sensitivity/specificity was estimated.
ResultsThe study included a total of 190 patients (male/female: 58%/42%). PICU was required in 11 (6%). The mean±SD ABSS-maximal score for patients who required and did not require PICU was 10.55±1.12 and 6.35±2.3, respectively (p<.001). The AUC for ABSS-maximal was 0.94 (p<.001, 95% CI: 0.90–0.98). The optimal cut-off point was set at ≥10 points for a sensitivity of 82% and a specificity of 91%.
ConclusionsABSS estimates the severity of AB regarding the need for PICU admission, with a sensitivity and specificity of clinical usefulness.
En la actualidad existen pocas escalas validadas para valorar la bronquiolitis aguda (BA) y escasa información de su potencia de prueba. El objetivo del presente estudio es valorar la validez de una escala de severidad de BA (ESBA) para orientar los ingresos en UCIP.
Pacientes y métodoEstudio observacional prospectivo descriptivo de lactantes previamente sanos menores de un año con BA, donde se utilizó la ESBA para contrastar la gravedad con la necesidad de ingreso en UCIP. El tamaño de la muestra se estimó en al menos 175 pacientes. El equipo investigador fue entrenado en el uso de la ESBA. Todos los pacientes del estudio fueron evaluados con la ESBA diariamente y en caso de deterioro clínico. Se analizaron y compararon las puntuaciones ESBA inicial y máxima respecto a la necesidad de UCIP. Se construyó una curva operativa de receptor, se calculó el área bajo la curva y se estimó el punto óptimo de sensibilidad/especificidad.
ResultadosSe incluyó a 190 pacientes (varón/mujer: 58%/42%). Precisaron UCIP 11 (6%). La puntuación media± DE de la ESBA-máxima para pacientes que precisaron y no precisaron UCIP fue de 10,55±1,12 y 6,35±2,3, respectivamente. Esta diferencia fue significativa (p<0,001). El ABC para la ESBA-máxima fue 0,94 (p<0,001; IC del 95%: 0,90-0,98). El punto de corte óptimo se estableció en ≥ 10 puntos, para una sensibilidad del 82% y una especificidad del 91%.
ConclusionesLa ESBA estima la gravedad de la BA respecto a la necesidad e ingreso en UCIP con una sensibilidad y especificidad de utilidad clínica.
The possibility of assessing severity in patients with acute bronchiolitis (BA) based on clinical manifestations is of great interest to clinicians as an indispensable step in decision-making or for the purpose of sharing information with other providers regarding infants with AB. Clinical scoring systems are assessment tools that, based on the observation of certain variables in patients with a disease, allow the addition of ratings given to different items to obtain a total, cumulative score. Several scales have been published for assessment of bronchiolitis,1–5 and the one used most widely is the Wood-Downes-Ferres (WDF) scoring system.6,7 Since the WDF score is a modification of a scale originally developed for assessment of asthma patients, was not designed in consideration of the pathophysiology of AB and has not been originally designed for or validated in patients with AB, its use for assessment of this disease may not be justified.
On the other hand, few clinical scoring systems for AB have been validated,1,2,4 and even fewer have been studied for the purpose of establishing the sensitivity and specificity of different cut-off points in relation to changes in clinical parameters during the course of AB and patient outcomes. Some of the scales that have been validated attempt to comprehend the full range of infectious respiratory disease, without taking into account the specific pathophysiological characteristics of AB.3 In some instances, the validation process has revealed that the scale was a poor fit for bronchiolitis.8 Furthermore, the clinical practice guidelines published in Spain call for the development and validation of scales for the assessment of severity of AB.9 Recently published systematic reviews have voiced the need to validate scales specifically designed to assess severity in AB.10
The previously published Acute Bronchiolitis Severity Scale (ABSS) seems to be easy to use and administer,4 and has shown adequate test–retest reliability, inter-observer reliability and internal consistency. It is based on reproducible parameters commonly assessed in the physical examination and does not include measurements that require equipment such as oxygen saturation. The final score is obtained by adding the points obtained in the assessment of respiratory rate, heart rate, respiratory effort, the presence of adventitious breath sounds such as wheezing or crackles and measurement of the inspiration-to-expiration ratio. Each of these parameters is categorised and assigned a specific score. The final cumulative score ranges between 0 and 13 points.
Following the introduction of this scale in our hospital and its use in the assessment and followup of infants admitted in the past 5 years, the aim of this study was to assess the validity of this clinical scoring system and establish the optimal cut-off point for the identification of patients with very severe disease that may require admission to the PICU for administration of mechanical ventilation (MV).
Patients and methodsWe conducted a prospective, observational and descriptive study in previously healthy infants aged less than 1 year admitted with classical AB criteria11 to a children's referral hospital. We performed a sample size calculation and estimated that we needed at least 175 infants to achieve a 95% level of confidence assuming a proportion of patients admitted to the PICU with AB of 6.5% based on previous epidemiologic studies.12–14 We excluded patients with chronic underlying disease, such as heart disease, bronchopulmonary dysplasia and neurologic disorders associated with motor impairment. We also excluded infants admitted to the PICU for reasons other than respiratory problems associated with AB, such as intercurrent sepsis and/or apnoea. We conducted the study from September 1, 2015 to March 31, 2016. Our study adhered to the recommendations for research on diagnostic accuracy15 and was approved by the ethics board of our hospital.
Before starting data collection, the medical research team was trained on the use of ABSS to ensure a homogeneous interpretation of its parameters. Each of the members of the research team used a free application that had the ABSS (included in the Paediatric Scores application for Android smartphones, downloaded from the Google Play Store). The clinicians that managed the infants with AB were blinded to the reference that was going to be applied to assess the validity of the scale.
Having obtained the informed consent of their legal guardian, we assessed each patient using the ABSS at admission and then daily during their stay, as well as any time the patient's condition worsened. All of the scores were recorded in the patient's chart. At the end of the study, we analysed and compared the baseline and highest ABSS scores in relation to the need for PICU admission for MV (including non-invasive ventilation, continuous positive airway pressure, conventional MV or high-frequency oscillatory ventilation, and excluding patients that only required high-flow nasal cannula oxygen therapy). In patients admitted to the PICU, we considered the highest ABSS score prior to PICU admission. We used these scores to plot a receiver operating characteristic (ROC) curve for the need of admission to PICU for MV. We calculated the area under the curve (AUC) with the corresponding 95% confidence interval (CI) and estimated the optimal cut-off point in the upper left corner to maximise sensitivity and specificity. Using the resulting values, we calculated the positive likelihood ratio (LR+) and negative likelihood ratio (LR−) associated with the established cut-off point.
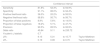
Table 1 presents the parameters assessed in the ABSS. Table 2 presents the description for the correct interpretation of each clinical parameter in the scale.
Items and scoring of the acute bronchiolitis severity scale.
| Score | 0 | 1 | 2 | 3 | 4 |
|---|---|---|---|---|---|
| Wheezing | No | Wheezing at end of expiration | Wheezing throughout expiration | Wheezing during inspiration-expiration | Severe hypoventilation |
| Crackles | No | Crackles in 1 field | Crackles in 2 fields | Crackles in 3 fields | Crackles in 4 fields |
| Effort | No effort | Subcostal or lower intercostal retractions | + Suprasternal retractions or nasal flaring | + Nasal flaring and suprasternal retractions (universal) | |
| I:E ratio | Normal | Symmetrical | Inverted |
| Age | 0 points | 1 point | 2 points |
|---|---|---|---|
| Respiratory rate | |||
| <2 months | <57 | 57–66 | >66 |
| 2–6 months | <53 | 53–62 | >62 |
| 6–12 months | <47 | 47–55 | >55 |
| Heart rate | |||
| <2 months | 125–152 | 153–180 | >180 |
| 2–12 months | 120–140 | 140–160 | >160 |
Summary for the interpretation of ABSS items.
| Wheezinga | Assess the presence of wheezing at the end of or throughout expiration and whether it is also audible during inspiration. In cases of severe obstruction, assess hypoventilation in absence of wheezing |
| Cracklesa | Assess the extent of clearly audible crackles in the chest in every respiratory cycle in each lung in both the anterior and posterior fields |
| Effort | Cumulatively assess the level of established and persistent respiratory effort from subcostal retractions to universal retractions, as described in the table |
| I:E ratio | Assess whether the inspiration-to-expiration ratio is normal, symmetrical, or inverted with prolonged expiration time |
| RR | Rate over the course of a minute without interference from coughing, crying or apnoeic episodes, according to age |
| HR | Basal heart rate measured over 1 minute, according to age |
ABSS, Acute Bronchiolitis Severity Scale.
Of a total of 215 patients with AB admitted to the unit, 12 had a chronic underlying disease, 2 were older than 12 months, 6 had been admitted to the PICU due to apnoeic episodes and 2 had been admitted due to sepsis associated with bronchiolitis. Three patients dropped out of the study, and 1 did not require MV after admission to the PICU. None of the patients in the sample died. The use of the scale was not associated with adverse events in any of the patients. The final sample comprised 190 infants that met all the inclusion criteria, of who 59% were male and 41% female. Testing of nasopharyngeal aspirate specimens detected respiratory syncytial virus in 148 of the patients (77.8%). Table 3 summarises the main characteristic of the patients. A total of 11 patients in the sample (5.8%) required admission to the PICU for MV.
Description of the sample of infants admitted due to acute bronchiolitis during the study (n=190).
| Median | IQR | |
|---|---|---|
| Age (months) | 1.83 | 1.08–3.25 |
| Birth weight (g) | 3200 | 2800–3530 |
| Weeks of gestation | 39 | 37.9–40 |
| Maternal age (years) | 30 | 25–34 |
| Weight at admission (g) | 4850 | 3937–5876 |
| ABSS at admission | 5.0 | 3–7 |
| Highest ABSS | 6.0 | 5–9 |
The mean±standard deviation (SD) of the baseline ABSS score in patients that required admission to the PICU for MV was 6.41±2.97, compared to 5.25±2.48 in patients that did not require it. The highest ABSS score in these groups of patients were 10.55±1.12 and 6.35±2.3, respectively. The comparison of mean values with the Student t-test was only significant for the highest ABSS score (p<.001). Table 4 presents the frequency distribution of the highest ABSS scores in infants admitted with AB. None of the patients scored 13 points at any time (the maximum possible score in the ABSS).
Frequency distribution of the highest ABSS scores during the stay of infants admitted with acute bronchiolitis.
| ABSS score | Absolute frequency | Percentage | Cumulative percentage |
|---|---|---|---|
| 1 | 1 | 0.5 | 0.5 |
| 2 | 5 | 2.6 | 3.2 |
| 3 | 17 | 8.9 | 12.1 |
| 4 | 15 | 7.9 | 20.0 |
| 5 | 26 | 13.7 | 33.7 |
| 6 | 34 | 17.9 | 51.6 |
| 7 | 30 | 15.8 | 67.4 |
| 8 | 14 | 7.4 | 74.7 |
| 9 | 23 | 12.1 | 86.8 |
| 10 | 12 | 6.3 | 93.2 |
| 11 | 8 | 4.2 | 97.4 |
| 12 | 5 | 2.6 | 100.0 |
| Total | 190 | 100.0 |
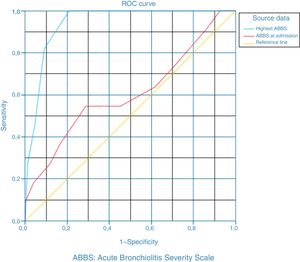
The AUC was 0.61 for the initial ABSS score (p=.24; 95% CI, 0.41–0.80) and 0.94 for the highest ABSS score (p<.001; 95% CI, 0.90–0.98). Fig. 1 shows both ROC curves. The optimal cut-off point to identify the most severely ill patients who may require intensive care and MV was a score of 10 points. Table 5 shows the contingency table for the association between the ABSS score and PICU admission. Table 6 presents the values of the sensitivity, specificity, LR+ and LR− for the selected cut-off point. We obtained a LR+ of 9.15 and a LR− of 0.19.
Diagnostic testing parameters for a 10-point cutoff in the ABSS in relation to PICU admission for MV.
| Confidence interval | ||||
|---|---|---|---|---|
| Sensitivity | 81.8% | 52.3% | to 94.9% | |
| Specificity | 91.1% | 86.0% | to 94.4% | |
| Positive likelihood ratio | 36.0% | 20.2% | to 55.5% | |
| Negative likelihood ratio | 98.8% | 95.7% | to 99.7% | |
| Proportion of false positives | 8.9% | 5.6% | to 14.0% | |
| Proportion of false negatives | 18.2% | 5.1% | to 47.7% | |
| Precision | 90.5% | 85.5% | to 93.9% | |
| Odds ratio | 45.84 | 9.11 | to 230.72 | |
| Youden's J statistic | 0.7 | |||
| LR+ | 9.15 | 5.31 | to 15.77 | Taylor Miettinen |
| LR− | 0.19 | 0.06 | to 0.70 | Taylor Miettinen |
LR−, negative likelihood ratio; LR+, positive likelihood ratio.
The results of our study support the validity of the ABSS for classification of patients with severe AB. Using ROC curve analysis, we found a valid cut-off point to help assess the need for PICU admission. The sample under study was representative of patients with AB during the epidemic season, as its composition was consistent, in epidemiological terms, with the descriptions found in the current literature.16,17,14 The sensitivity and specificity values were acceptable for the application of the scale in clinical practice. The values of the LR+ and LR− suggest that the selected cut-off point is valid to discriminate patients with severe respiratory problems in the context of AB. We assessed the post-test probability for the established cut-off point by means of the Fagan nomogram,18 and found that it would be useful in clinical practice to estimate the likelihood of a patient requiring paediatric intensive care.19
Our analysis was restricted to infants aged less than 12 months, as the mean age in most published case series ranges between 2 and 4 months and the most severe cases tend to cluster below age 6 months.20–22 We attempted to include the entire cohort of patients that developed AB during a single epidemic season, only excluding patients with underlying chronic diseases or admitted to the PICU for treatment of the apnoeas that may develop in association with AB, conditions that could be a source of bias given that the ABSS assesses impairment of respiratory function.
The reference standard we used to assess the validity of the scale was the need for admission to the PICU for administration of MV. While there is a degree of variability in the need for mechanical ventilation, we feel that this variable is a good proxy of disease severity in patients with AB. Blinding clinicians to this choice of standard guaranteed the internal validity of our study. Furthermore, the data in our study comprehended nearly the entire range of possible scores in the ABSS (Table 4), as the only score that was never obtained in our sample was 13, the highest possible score in the scale. Comparison of the ABSS with scales that have not been validated, such as the WDF, showed slightly greater values of the AUC for the ABSS, although a different external reference standard of severity was used in the assessment of each scale.23
The ABSS at admission is not a good predictor of eventual need of PICU admission, although it is important to consider that the purpose of the scale is to assess the severity of disease, rather than predict patient outcomes.
As for the scale itself, every parameter it includes is directly associated with impairment of respiratory function and assesses clinical variables that have been included traditionally in various scales assessing respiratory disease. The ABSS may only be administered by trained health professionals, unlike other scales that have been developed to be used by any caregiver.3 There is debate as to whether oxygen saturation should be included in this or other scales for the assessment of severity of AB. Some AB scoring systems include this parameter so that patients receiving varying degrees of respiratory support are scored differently.1 In our opinion, including this parameter not only decreases the feasibility of this scoring system, but also obstructs some of the applications of the scale, such as assessing the response to oxygen therapy using the same standard employed to assess respiratory function previous to initiation of support. There is evidence of a trend to overestimate severity based on pulse oximetry and its association with an increase in hospital admissions of patients with AB,24 which leads us to believe that including this parameter in an AB assessment scale offers no benefits, while it may preclude its use in outpatient settings with fewer technological resources, which is a disadvantage considering that a shared “language” is necessary for adequate communication between levels of care.
One of the main limitations of our study is that it was conducted in a single hospital. In addition, we only analysed PICU admissions during a single season, which may result in a decreased reliability of our results. However, we believe that these results are probably reproducible in other hospitals, since it is very easy to assess the parameters included in this scale. Performance of multicentre prospective studies would be useful to corroborate the findings of our study.
In conclusion, the ABSS can help clinicians identify patients at higher risk of requiring respiratory support at the PICU level. Patients can clearly benefit from the use of the ABSS, as it allows quantification of clinical deterioration with a specific score that would alert clinicians of patients that are at higher risk. Weighing this benefit against the near-zero probability of adverse effects and given its easy implementation, the ABSS can be considered cost-effective and worth using routinely.
Conflicts of interestsThe authors have no conflicts of interest to declare.
Please cite this article as: Ramos-Fernández JM, Piñero-Domínguez P, Abollo-López P, Moreno-Pérez D, Cordón-Martínez AM, Milano-Manso G, et al. Estudio de validez de una escala de gravedad de la bronquiolitis aguda para orientar el ingreso en UCIP. An Pediatr (Barc). 2018;89:104–110.