The representation of Spain in European epidemiological studies on diabetes is limited, with only one centre in the Hvidoere study and another in the SWEET study. No Spanish studies have been published that combine epidemiological data and care resources. The aim of this study was to determine the epidemiological data, care resources and use of new technologies in all Andalusian hospitals that care for children with diabetes mellitus type 1 (DM1) under 14 years.
Material and methodsAn electronic questionnaire of 18 questions was sent to all paediatric endocrinologists who treated children with diabetes in Andalusian hospitals.
ResultsThere was a mean of 3.12 (SD: 2.58) paediatric endocrinologist for every 100 patients, with a mean diabetes nurse educator ratio of 2.50 (SD: 3.94) per 100 patients and centre. Only 1 of the 29 centres had a psychologist, 9/29 had a day hospital and 11/29 had a 24-h telephone line. The mean of days of consultations exclusively for patients with DM1 was 1.56 days (SD: 1.21) per week. Continuous insulin infusion was used to treat 5% of patients, with a significant increase in centres with more than 150 patients.
ConclusionsThis study offers, for the first time, current data on the epidemiological situation related to healthcare data, comparing them with the recommendations of European standards, highlighting a low ratio of endocrinologists and educators in diabetes, absence of psychologists and low technology penetrance.
La representación de nuestro país en los estudios epidemiológicos europeos en diabetes es exigua, tan solo un centro en el estudio Hvidoere y otro en el SWEET. No existen estudios publicados en España que combinen datos epidemiológicos y recursos asistenciales. El objetivo de este estudio es conocer los datos epidemiológicos, los recursos asistenciales y el uso de nuevas tecnologías en los hospitales andaluces que atienden a niños con diabetes mellitus tipo 1 (DM1) menores de 14 años.
Material y métodosUn cuestionario electrónico de 18 preguntas fue enviado a los endocrinólogos pediátricos que atendían a niños con DM1 en todos los hospitales andaluces.
ResultadosLa media de la ratio de endocrinólogo pediátrico por 100 pacientes fue 3,12 (DE: 2,58). La media de la ratio de enfermero educador en diabetes por 100 pacientes y centro fue de 2,50 (DE: 3,94). Solo uno de los 29 centros disponía de psicólogo, 9/29 disponían de hospital de día y 11/29 disponían de atención telefónica durante 24h. La media de días de consulta a la semana destinados exclusivamente a pacientes con DM1 fue de 1,56 días (DE: 1,21). Un 5% de los pacientes fueron tratados con infusor continuo de insulina, con un aumento significativo en los centros que tenían más de 150 pacientes.
ConclusionesEste estudio ofrece por primera vez datos actuales de la situación epidemiológica en Andalucía en relación con los datos asistenciales; comparándolos con las recomendaciones de estándares europeos, destaca una baja ratio de endocrinólogos y educadores en diabetes, ausencia de psicólogo y baja penetrancia de tecnología.
The importance of type 1 diabetes mellitus (T1D) in children has grown in recent years, with its incidence and prevalence increasing in Spain1 and other European countries, a phenomenon that has also been observed in Andalusia.2,3
The first prospective study performed in Andalusia that collected data for the entire autonomous community by searching hospital records for the 2000–2009 period reported an incidence of T1D in children aged less than 14 years of 20.76 cases per 105 inhabitants per year (age 0–4 years: 14.34 cases/105 inhabitants/year; age 5–9 years: 23.46 cases/105 inhabitants/year; age 10–14 years: 25.15 cases/105 inhabitants/year).1
Several studies have demonstrated significant variability between healthcare facilities in the management of children with diabetes,4,5 and the increasing complexity of new technologies applied to the management of diabetes may require a restructuring of the care provided to these patients6 and the institution of centres of reference.7
Some European countries have national registries of the paediatric population with diabetes, collecting not only epidemiologic data, but also data for the assessment of patient outcomes during follow-up.8,9 Groups that study and follow up cohorts of children with diabetes continue to report that there is significant variability in clinical management between centres.10 One such study conducted in the United Kingdom in 2008 that compared its results with those of 2002 found partial non-adherence to clinical guidelines.11
The Hvidøre group has assessed the level of metabolic control in children and adolescents.12 They analysed clinical characteristics, insulin regimes, acute complications and comorbidities. They found differences between hospitals in the levels of glycated haemoglobin (HbA1c), which continued to be significant after adjusting for insulin regimen. This group has presented data obtained from 26 hospitals in 23 countries (including 1 in Spain) and analysed several variables that could contribute to the differences in metabolic control, through both diet13 and exercise,14 and found no statistically significant associations. There is evidence that “nonmedical” variables (communication, clear goal-setting and family factors, among others15) may have a greater impact on adherence to treatment.16
The SWEET group17 (acronym for Better control in Pediatric and Adolescent diabeteS: Working to crEate CEnTers of Reference) started out as a partnership of organisations in 13 European countries led by the International Society for Pediatric and Adolescent Diabetes (ISPAD) with the purpose of developing quality control systems and recommendations for care and treatment of diabetes in children and adolescents. At present, it collects data from 48 centres, some outside Europe, including centres in Africa, North America, South America and Asia.
The representation of Spain in these studies is scarce. There is only one Spanish centre participating in the Hvidøre study and one other included in the SWEET registry. Neither of these studies is very representative of the clinical situation of diabetes in Europe, especially Spain.
The aim of this study was to evaluate the epidemiological data, healthcare resources and use of new technologies of Andalusian hospitals managing children aged less than 14 years with T1D.
Materials and methodsWe sent a link to an online questionnaire to all public and private hospitals in Andalusia that managed children with T1D and resent the link three times to minimise missing data. The questionnaire comprised 18 items and fields for collection of identifying data for the responding clinicians and facilities. The items were organised into three sections to collect data on epidemiological variables, healthcare resources and the use of new technologies. We accepted responses between January and December 2014.
A similar questionnaire had been tested in a previous nationwide study (2009)18 and a regional study (2013),19 with response rates exceeding 90%.
We categorised participating hospitals based on the number of children with T1D that they managed and taking as a reference the centre size classification proposed by the SWEET registry, into: (a) large centres (more than 150 patients); (b) medium-sized centres (150 to 50 patients), and (c) small centres (fewer than 50 patients).7
Patients under studyWe included individuals that had received a diagnosis of T1D as children and were followed up in paediatric services. The age of patients ranged between 0 days and 14 years, and we did not collect specific data for this variable. We did not perform any type of sampling and instead attempted to collect data on as many patients as possible who were being followed up in these centres. To this end, we appointed a collaborating researcher in each province who was well acquainted with their area and submitted the questionnaire to local hospitals. The purpose of this appointment was to increase patient recruitment and to monitor data collection to prevent potential errors.
We anonymised the data, so identification of included patients would be impossible, which exempted our study from the need to obtain informed consent.
Local databases were managed anonymously, and a central database was formed for each province that was managed by the appointed researcher and registered with the Data Protection Agency by the submission of an electronic form, as mandated by the Spanish Organic Law on the Protection of Personal Data.
Statistical methodsWe performed a descriptive analysis, summarising continuous variables as mean and standard deviation (SD), and categorical variables as percentages.
We compared groups by means of the Student t-test for independent samples. We assessed the associations between variables by means of analysis of variance. We used the Kruskal–Wallis when dependent variables did not follow a normal distribution.
We assessed the correlation between nonparametric ordinal variables by means of the Spearman rho, the correlation between mixed data by means of the Kendall tau and the correlation between normally distributed variables by means of the Pearson correlation coefficient. We defined statistical significance as a p-value <0.05. We exported the responses submitted online to a Microsoft Excel database and subsequently to the free statistical software application R (https://www.r-project.org/).
ResultsThe study included 29 Andalusian hospitals (100% of hospitals that followed up children with diabetes), which managed approximately 2547 patients with T1D, of whom 325 had received the diagnosis in the last year. Using as reference the number of children aged less than 14 years (incidence) and less than 15 years (prevalence) reported by municipal population censuses from 2013:
- –
The minimum incidence was 23.5/100 000.
- –
The minimum prevalence was 1.7/1000.
At the time of diagnosis, 32% of patients had diabetic ketoacidosis and needed to be hospitalised for a mean of 6.2 days.
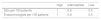
When it came to centre size, the 4 hospitals in group 1 managed 1189 patients, the 12 hospitals in group 2 managed 1021 patients and the 13 hospitals in group 3 managed 337 patients (Table 1).
Distribution of the number of patients and the endocrinologist- and DE-to-patient ratio (per 100 patients with diabetes).
| Group | Hospitals | Patients (n) | Endocrinologists | DEs | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Range | Total | Mean (SD) | Range | Mean (SD) | Range | ||
| 1 | 4 | 297.25 (132.41) | 159–425 | 1.189 | 0.71 (0.45) | 0.2–1.2 | 0.37 (0.19) | 0.2–0.6 |
| 2 | 12 | 85.08 (29.31) | 55–143 | 1021 | 1.85 (1.03) | 0–3.6 | 1.55 (0.74) | 0–3.17 |
| 3 | 13 | 25.92 (11.52) | 10–46 | 337 | 5.24 (2.49) | 2.17–10 | 4.04 (5.55) | 0–20 |
Group 1: following up more than 150 patients. Group 2: following up 50–150 patients. Group 3: following up fewer than 50 patients. We show the mean and standard deviation, range (minimum–maximum) and total.
SD, standard deviation; DE, diabetes educator.
Paediatric endocrinologists involved in the care of patients with diabetes: the mean number of endocrinologists per hospital was 1.38 (SD, 0.56), with a minimum of 0 and a maximum of 2. The cumulative number of endocrinologists was 7 in group 1, 18 in group 2 and 15 in group 3.
Ratio of endocrinologists involved in diabetes care per 100 patients with T1D: the overall ratio of endocrinologists per 100 patients was 3.12 (SD, 2.58). In the analysis by groups, we found a ratio of 0.70 in group 1 (SD, 0.45), of 1.84 in group 2 (SD, 1.03) and of 5.24 in group 3 (SD, 2.48). We found statistically significant differences in the ratio of endocrinologists per 100 patients between groups, but not within groups (Table 1).
Diabetes educators (DEs): the mean number of DEs per hospital was 0.98 (SD, 0.66), with a minimum of 0 and a maximum of 2.
Ratio of DEs per 100 patients: the mean ratio of DEs per 100 patients with T1D and per centre was 2.50 (SD, 3.94). When we analysed by group, we found that the ratio was 0.37 in group 1 (SD, 0.19), 1.55 in group 2 (SD, 0.73) and 4.03 in group 3 (SD, 5.55). We did not find statistically significant differences in this ratio between or within groups (Table 1).
Dietitians: Eight of 29 centres had dietitians. When we analysed by group, we found that the percentage of centres where a dietitian was available was 50% in group 1 (2/4), 16.7% in group 2 (2/12) and 30% in group 3 (4/13).
Psychologists: only one hospital had a psychologist in staff for these patients (1/29); it belonged to group 2.
Use of advanced technologiesUse of continuous subcutaneous insulin infusion (CSII): we collected data for a total of 142 insulin pumps used in the management of a total of 2547 patients (5.5%).
The mean number of patients treated with CSII was 22 in the hospitals of group 1(SD, 9.20), with a range of 15–35 (7.4% of patients were received CSII). In group 2, the mean number of patients treated with CSII was 3.75 patients (SD, 4.67), with a minimum of 0 and a maximum of 15 (1.4% of patients received CSII). In group 3, the mean number of patients treated with CSII was 0.69 (SD, 1.03), with a minimum of 0 and a maximum of 3 (0.89% of patients treated with CSII) (Table 2).
One-way ANOVA revealed statistically significant differences between groups in the use of CSII, with the highest use found in the hospitals of group 1 (p<0.001). The differences within groups in the use of CSII were not statistically significant.
Since this variable did not meet the assumptions of normality or homogeneity of variance, we used the nonparametric Kruskal–Wallis test and obtained a p-value of 0.001, which indicated the presence of differences between groups. This led us to perform the Mann–Whitney U-test with the Bonferroni correction, which revealed significant differences between groups 1 and 2 (p=0.003) and groups 1 and 3 (p=0.003).
Use of continuous glucose monitoring (CGM): 10 out of 29 hospitals used CGM. These hospitals included 75% of the centres in group 1 (3/4), 50% of the centres in group 2 (6/12) and 7.7% of the centres in group 3 (1/13).
Below are the differences between groups:
- -
Groups 1 and 2: p=0.72, 95% CI for the difference in proportions, –0.42 to 0.93.
- -
Groups 1 and 3: p=0.03, 95% CI for the difference in proportions, 0.06 to 1.28.
- -
Groups 2 and 3: p=0.05, 95% CI for the difference in proportions, 0.00 to 0.82.
Number of days a week that hospitals held clinics devoted exclusively to diabetes, where care was not shared with other metabolic disorders: mean of 1.56 days a week (SD, 1.21), with a range of 0–5 days. Hospitals in group 1 offered exclusive diabetes care services a minimum of 0 days and a maximum of 5 days a week, with a mean of 2.75 days (SD, 2.21). In group 2, the minimum was 0 days and the maximum 3 days, with a mean of 1.21 days (SD, 0.84). In group 3, the minimum was 1 day and the maximum 3 days, with a mean of 1.50 days (SD, 0.89). We performed ANOVA, which revealed differences between groups with a p-value that neared the threshold for statistical significance (p=0.08).
Day hospital: 11 out of 29 hospitals offered day hospital services (38%). When we analysed this variable by group, we found that these services were offered by 50% of hospitals in group 1 (2/4), 50% in group 2 (6/12) and 23.1% in group 3 (3/13). The differences between groups were not statistically significant.
Round-the-clock telephone consultation: Nine hospitals out of 29 offered telephone consultation 24h a day; including 25% of hospitals in group 1 (1/4), 8.3% of hospitals in group 2 (1/12) and 53.8% of hospitals in group 3 (7/13).
Frequency of check-ups: patients had checkups at a mean interval of 3.09 months (SD, 0.27), with a maximum of 4 months and a minimum of 3 months. When we analysed by group, we found that patient checkups were performed at a mean interval of 3.38 months in group 1 (SD, 0.48), of 3.08 months in group 2 (SD, 0.19) and 3.00 months in group 3 (SD, 0.22). The analysis of variance found statistically significant differences between groups (p=0.04). The differences within groups were not significant.
Length of stay at onset: the mean length of stay following diagnosis was 6.19 days (2.35), with a minimum of 3.16 days and a maximum of 16 days. When we calculated length of stay per group, we found that the mean stay was 5.2 days in group 1 (SD, 1.90), with a range of 2.2–8.3 days; 5.85 days in group 2 (SD, 0.95), with a minimum of 5.25 and a maximum of 6.45; and 6.8 days in group 3 (SD, 3.20), with a minimum of 4.85 and a maximum of 8.73. The ANOVA did not detect statistically significant differences between or within groups.
DiscussionThis study is the first to report current epidemiologic information on the management of T1D in Andalusia based on healthcare data, comparing it to European criteria for diabetes centres of reference.
In reference to these criteria,7 we found that the mean number of endocrinologists per 100 patients in centres managing more than 150 patients (group 1) was 0.70, which corresponds to a low-to-intermediate level of care (Table 3). When it came to the ratio of DEs per 100 patients in centres with more than 150 patients, the mean was 0.37, which corresponds to a low level of care.
Recommendations for the number of professionals per 100 patients in the diabetes care team by level of care.
| High | Intermediate | Low | |
|---|---|---|---|
| DEs per 100 patients | 1 | 0.6 | 0.5 |
| Endocrinologists per 100 patients | 1 | 0.8 | 0.5 |
DE, nurse working as a diabetes educator.
Adapted from Danne et al.7
We were unable to make comparisons with these quality standards for hospitals that did not belong to group 1, as the reference centres used to develop the standards managed 150 or more patients with diabetes.
Type 1 diabetes is a chronic disease whose management requires a holistic approach and delivery by a multidisciplinary team with setting of shared goals.20
A diabetes diagnosis, with the significant changes its management entails, may trigger high levels of stress, affect mood and reduce quality of life21,22 both in children and their families, so involvement of a multidisciplinary team from the outset is essential to facilitate an adequate adaptation to the disease.23,24
The document of the 2014 ISPAD consensus guidelines of 201425 stated that young people with diabetes appear to have a higher incidence of depression, anxiety, psychological distress and eating disorders compared to their healthy peers. In light of this evidence, we ought to underscore that in our study, only 1 diabete unit in 1 of the 29 surveyed hospitals in Andalusia had a psychologist in the care team.
Continuous subcutaneous insulin infusion is considered a very effective and safe treatment that is widely used by children and adolescents with T1D. This modality offers several benefits to children and adolescents, such as optimal glycaemic control, a reduced frequency of severe hypoglycaemic episodes, improved quality of life, greater flexibility and a reduction of HbA1c levels.26–29
The use of CSII in the paediatric age group has increased substantially in the last decade (2007–2016), although it is still limited in some European countries. The main factors preventing the widespread use of this modality is the lack of funding of health systems and the reduced number of health professionals trained in its use and of diabetes educators.30
In 2015, the SWEET Registry collected information from 48 centres managing 28 667 aged 0 to 18 years and found that 40.2% were treated with CSII.31
This prevalence of CSII use is far from the one found in our survey, where CSII was used in 5.5% of patients. A logistic regression model of data from the SWEET Registry adjusted for age, sex and duration of diabetes found that use of CSII increased with centre size.32 This is consistent with our survey results, as we found statistically significant differences between centre groups, with a higher percentage of CSII use in centres that managed more than 150 patients.
The use of advanced technologies in CSII and CGM requires an increased allocation of human resources,30 which in our study mainly occurred in hospitals classified in group 1, where the ratios of paediatric endocrinologist and DEs per 100 patients were lower. This finding further emphasised the scarcity of human resources in centres managing more than 150 patients.
Epidemiologic data for Andalusia show that the incidence remains high relative to the rest of the Spanish population, more than doubling the current incidence in Vizcaya,33 and we are offering data on prevalence for the first time.
It would be useful to track quality indicators (HbA1c, number of episodes of severe hypoglycaemia/100 patients, number of ketoacidosis-related admissions/100 patients, among others), as surveillance on these outcomes and comparison with data from European registries would allow us to identify the care resources that may be inadequate.
Although the data presented here refer to a single autonomous community in Spain, the size of the survey and the 100% response rate, with data from every hospital in the region, are significant strengths.
One possible limitation of this study is the potential inaccuracy in case data collection. The collection of quantitative data, such as the number of patients managed in each hospital, the number of cases diagnosed each year, etc., depends on the clinicians that were the point of contact for each facility.
In conclusion, we present the first epidemiological data on the care resources available to children and adolescents with T1D in the Autonomous Community of Andalusia. We take this opportunity to underscore the importance of establishing and analysing the human resources devoted to the management of these patients, which should be considered when planning and allocating resources for health care in T1D.
Conflict of interestThe authors have no conflicts of interest to declare.
We want to thank the GADI collaborative group (Grupo Andaluz de Diabetes Infantil, Andalusian Group on Childhood Diabetes).
Please cite this article as: López-Siguero JP, Pérez-González O, Gómez-Gila AL, Leiva-Gea I. Situación de la diabetes mellitus tipo 1 en Andalucía. Datos asistenciales, uso de terapias avanzadas y recursos humanos. An Pediatr (Barc). 2018;89:111–116.