Takayasu arteritis is a chronic inflammatory and granulomatous vasculitis of autoimmune aetiology that affects the large vessels and may lead to the development of stenosis, occlusion or aneurisms.1 Its incidence is of 1.2–2.6 cases per million inhabitants,1 and it therefore may be the third most frequent vasculitis in the paediatric age group following Henoch-Schönlein purpura and Kawasaki disease. It usually has onset in adulthood, with its incidence peaking between ages 25 and 30 years.2
We present the case of a patient with atypical features of this disease, including her young age, the short time elapsed between onset and diagnosis, the short length of the aortic segment involved and the diagnosis during the inflammatory phase, emphasising the considerable usefulness of positron emission tomography/computed tomography (PET/CT), which allowed an early diagnosis.
The patient was a girl aged 5 years with no relevant history that was brought to the emergency department with intermittent but intense periumbilical abdominal pain of 2 weeks’ duration, associated with fever of up to 38°C with no additional symptoms. Her vital signs, including the blood pressure in all 4 extremities, and the general examination were normal. The examination did not detect cardiac or abdominal murmurs and the carotid, axillary, antecubital, inguinal and popliteal pulses were all normal.
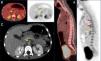
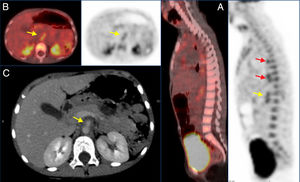
The blood tests revealed microcytic anaemia (haemoglobin, 10g/dL; mean corpuscular volume, 68) with leucocytosis (13000/mm3, 74% neutrophils) and an elevated serum C-reactive protein (CRP) level of 18.4mg/dL, while the liver and kidney function tests were normal. The findings of a throat swab culture, urinalysis, chest radiograph and abdominal ultrasound examination were normal. Since the symptoms persisted and the elevation of CRP increased (to a maximum of 32mg/dL), a computed tomography (CT) scan was performed that revealed periaortic wall thickening between the exit of the celiac trunk and the proximal third of the superior mesenteric artery (SMA) compatible with periaortitis (Fig. 1), which led to referral to our hospital.
PET/CT and CT images. (A) Sagittal PET/CT and CT views showing increased tracer uptake in the walls of the thoracic aorta (red arrows) and superior mesenteric artery (yellow arrow). (B) Axial PET/CT and CT views showing increased uptake in the walls of the superior mesenteric artery with a SUVmax of 4.03 (yellow arrows). (C) Axial CT view showing thinning of the walls of the proximal segment of the superior mesenteric artery (yellow arrow).
Samples were obtained for blood and stool culture, serologic tests (syphilis, cytomegalovirus, Mycoplasma, parvovirus), Mantoux, autoimmunity study (antinuclear [ANA] and extractable nuclear antigen [ENA], anti-proteinase 3 [PR3] and anti-myeloperoxidase [MPO] antibodies, rheumatoid factor), quantification of levels immunoglobulins—including IgG4—and complement levels, all with normal or negative results. The findings of the cardiac and ophthalmological evaluations were normal. An abdominal doppler ultrasound examination confirmed the findings of the CT scan; and the findings of an ultrasound scan of the supra-aortic trunks were normal. Given the small extension of the periaortitis and the absence of stenosis, a PET/CT scan was ordered, which revealed patchy deposits in the wall of the thoracic descending aorta with a maximum standardised uptake (SUVmax) of 4.11 and diffuse enlargement of 2.3cm in the abdominal aorta with a SUVmax of 4.03, suggestive of vascular inflammation (Fig. 1).
The patient received a diagnosis of Takayasu arteritis type III. The initial treatment consisted of steroids, first delivered intravenously and after by the oral route, and methotrexate, and achieved rapid resolution of the pain and a reduction in the serum levels of CRP. At one month, given the persistence of CRP elevation, the patient started treatment with infliximab, with a very good response. At present (age 7 years), the patient is asymptomatic and serial Doppler ultrasound examinations have demonstrated the resolution of aortic thickening, while the findings of follow-up MR angiography and CPR tests have been normal.
The course of Takayasu arteritis is divided into 2 phases. The initial inflammatory phase is characterised by intermittent nonspecific symptoms (fever, anorexia, night sweats, weight loss) and may last months or even years. It is followed by an occlusive phase, which manifests with headache, ischaemic strokes, hypertension or intermittent claudication in the upper or lower extremities, among other symptoms. The nonspecificity of the initial symptoms accounts for the mean delay in diagnosis of 11 months reported for the paediatric age group.3 In children, the most commonly involved sites are the renal arteries and the abdominal aorta.3
In 2010, new criteria were published for the classification (not for diagnosis) of several paediatric vasculitis, including Takayasu arteritis (Table 1).4
Criteria for classification of Takayasu arteritis proposed by the European League Against Rheumatism (EULAR), the Paediatric Rheumatology International Trials Organisation (PRINTO) and the Paediatric Rheumatology European Society (PRES).
| Mandatory criterion | Additional criteria |
|---|---|
| Angiographic abnormality detected by angiography (conventional, CT, or MRI) of the aorta or its main branches and pulmonary arteries showing aneurysm/dilatation, narrowing, occlusion or thickened arterial wall; these changes are usually focal or segmental | Lost/decreased peripheral artery pulse and/or claudication in limbs |
| Discrepancy of four limb systolic blood pressure >10mm Hg difference in any limb | |
| Audible murmurs or palpable thrills over large arteries | |
| Arterial hypertension (Systolic/diastolic BP greater than 95th centile for height) | |
| Elevation of acute phase reactants (erythrocyte sedimentation rate>20mm or CRP above the reference value applied in the laboratory) |
Requires meeting the mandatory criterion and at least 1 additional criterion.
Although it has been classically diagnosed by means of angiography, PET/CT has demonstrated a high sensitivity and specificity,5 especially in patients that have not reached the occlusive phase or with involvement of a small aortic segment, as was the case in our patient. Magnetic resonance angiography is very useful, but it poses some challenges in paediatric patients (higher heart rates; smaller volumes of contrast, as the dose is based on weight; breathing movements during sedation),6 especially in cases without occlusion; it offers a high resolution for the definition of anatomical structures, but provides little information on inflammatory activity.
The treatment is based on the administration of corticosteroids, immunosuppressive agents (methotrexate, azathioprine) and biological agents (anti-TNF or, more recently, anti-IL6).
The diagnosis of Takayasu arteritis should be contemplated in patients with prolonged or recurrent fever, intermittent abdominal pain, hypertension or focal neurologic signs associated with an unexplained elevation of acute-phase reactants. Early diagnosis allows prompt initiation of treatment and can prevent the progression of the disease to an irreversible stage.
Please cite this article as: Pastor Martínez R, Gallardo Padilla M, Peña González LP, Gómez Grande A, de Inocencio Arocena J. Utilidad de la PET/TAC en el diagnóstico de la arteritis de Takayasu de segmento corto. An Pediatr (Barc). 2019;91:55–57.