Although fever has beneficial effects, its control is recommended due to the general malaise associated with it.1 Its presentation leads parents to seek emergency services due to fear of seizures, brain damage or severe disease.1 Good clinical practise guidelines (GCPGs) recommend controlling fever by physical methods and the administration of antipyretics to improve the wellbeing of the child.2,3 However, surveys of doctors reveal indications for their use that are not recommended.4,5 To evaluate this behaviour prospectively, we analysed the prescription of antipyretic drugs in a paediatric emergency room.
The study protocol was approved by the local committee for research and ethics. We recruited 181 patients younger than 16 years, previously healthy, that had acute fever (<72h) in their first visit to the emergency department and discharged in less than 24h without fever. The paediatrician in charge made the treatment decisions. Risky indications were reported, and it was ensured that the doses administered were given at the correct dosage.
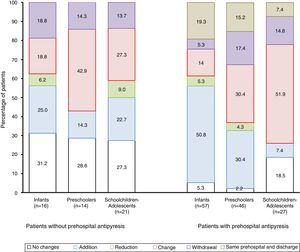
We analysed age, sex, administration of prehospital medication, history of febrile seizures and reason for seeking care, medication(s) administered at the hospital, and medication(s) prescribed at discharge. We analysed changes by age group. The changes considered were: (1) no changes; (2) addition: to antipyretic agent(s) given prehospital or at the hospital; (3) substitution: the prescription at discharge differed in at least one antipyretic agent from previous prescription; (4) reduction: the number of antipyretics prescribed at discharge was lower; (5) withdrawal of antipyretics at discharge; and (6) same treatment before admission and at discharge, with changes in antipyretic prescription only at the emergency room.
We performed the statistical analysis using absolute frequencies and percentages, comparing variables with the χ2 test, analysis of variance and the nonparametric Kruskal–Wallis test as applicable. We set the level of statistical significance at P<.05.
The main reasons for seeking care were respiratory and gastrointestinal infections. The former predominated in infants and preschoolers, and the latter in schoolchildren and adolescents (Table 1).
Body temperature control in the emergency room by age group, N (%).
| Infants | Preschoolers | Schoolchildren and adolescents | P-value | |
|---|---|---|---|---|
| N=73 | N=60 | N=47 | ||
| Sex, N (%) | .26a | |||
| Male | 45 (61.6) | 29 (48.3) | 24 (51.1) | |
| Female | 18 (38.4) | 31 (51.7) | 23 (48.9) | |
| Infection site, N (%) | .052a | |||
| URTI | 47 (64.4) | 39 (65.0) | 20 (42.6) | |
| PIGE | 12 (16.4) | 16 (26.7) | 22 (46.8) | |
| Febrile syndrome | 6 (8.2) | 1 (1.7) | 3 (6.4) | |
| UTI | 4 (5.5) | 1 (1.7) | 1 (2.1) | |
| LRTI | 2 (2.8) | 2 (3.3) | 1 (2.1) | |
| Other | 2 (2.8) | 1 (1.7) | 0 | |
| History of febrile seizure, N (%) | 6 (8.2) | 0 | 0 | .01a |
| Antipyresis before admission, N (%) | ||||
| Monotherapy | 44 (60.2) | 28 (46.6) | 21 (44.7) | .09a |
| Combination (2) | 11 (15.0) | 16 (26.6) | 6 (12.7) | |
| Combination (3) | 1 (1.4) | 2 (3.3) | 0 | |
| Combination (4) | 1 (1.4) | 0 | 0 | |
| No antipyresis | 16 (21.9) | 14 (23.3) | 20 (42.7) | |
| Antipyresis in emergency room, N (%) | ||||
| Monotherapy | 65 (89) | 53 (88) | 41 (87) | .65a |
| Combination (2) | 3 (4) | 4 (6) | 1 (2) | |
| Only physical methods | 5 (7) | 3 (5) | 5 (11) | |
| Antipyresis prescribed at discharge, N (%) | ||||
| Monotherapy | 20 (40) | 22 (37) | 11 (23) | .70a |
| Combination (2) | 33 (45) | 27 (45) | 27 (57.5) | |
| Combination (3) | 5 (7) | 3 (5) | 2 (4) | |
| Only physical methods | 6 (8) | 8 (13) | 7 (8) | |
| Temperature at admission, °C | ||||
| Mean±1 SD | 38.4±0.4 | 38.5±0.5 | 38.5±0.4 | .55b |
| Minutes elapsed to temperature control, median (min-max) | ||||
| No antipyresis before admission | 60 (19–80) | 60 (30–105) | 68.5 (40–162) | .12c |
| Antipyresis before admission | 60 (10–190) | 60 (19–130) | 78 (30–182) | .004d |
LRTI: lower respiratory tract infection (bronchiolitis, acute bronchitis); Other: mesenteric adenitis (1) and dentition (1) in infants, hand-foot-mouth disease (1) in a preschooler; febrile syndrome: fever without a source; PIGE: probably infectious gastroenteritis with or without dehydration; URTI: upper respiratory tract infection (rhinopharyngitis, pharyngitis, pharyngoamygdalitis, laryngitis, laryngotracheitis and otitis media); UTI: urinary tract infection.
The number of patients that received prehospital antipyretic treatment was 130 (71.8%); this proportion was higher in infants (78.1%) and preschoolers (76.7%) than in schoolchildren and adolescents (57.4%) (χ2=6.9; df=2; P=.03). The most common pattern was prescription of a single antipyretic agent (N=93), but two alternating agents were prescribed in 25.3% (33/180) of patients, and more than two in four patients. The most frequently prescribed agents were paracetamol and ibuprofen (in monotherapy or alternating). In infants it was paracetamol (43.8%), as opposed to ibuprofen in preschoolers (54%) and schoolchildren and adolescents (64.7%).
All patients were treated with physical methods in the emergency room, and 92.2% (167/181) with at least one antipyretic in monotherapy (159/167; 94%), with no differences between groups (Table 1). The most frequently prescribed antipyretic agent, in monotherapy or in combination, was metamizole (97/167; 58%), followed by paracetamol (51/169; 30.2%) and ibuprofen (19/169; 11.2%). Eight patients received a combination (paracetamol and naproxen). The route used most frequently in infants was the rectal route (73.5%); in preschoolers they were the rectal (43.9%) and oral (29.8%) routes; and in schoolchildren and adolescents, the oral route (52.4%). The mean time elapsed until the body temperature normalised was 1h.
Of the children that did not receive prehospital antipyretic agents, 22% (11/50) were discharged with a prescription for physical antipyresis alone, and there were no changes in treatment in 31%. In the rest, the most frequent changes were the addition of an antipyretic agent other than the one used in the emergency room, or switching to another (Fig. 1).
Distribution of the modifications in antipyretic management by age group and depending on whether the patient had received prehospital antipyresis (first three bars) or not (last three bars). The modifications considered were: addition, if other agent(s) were added to the original prescription; reduction, if the original treatment consisted of two or more agents and the discharge prescription included fewer of them; change, if the final prescription differed in at least one to all the antipyretic agents; withdrawal, if antipyretic treatment was discontinued completely; same prehospital and discharge when the antipyresis scheme was only modified during the hospital stay. The difference between groups without prehospital antipyresis was χ2=3.9; df=8; P=.90; and the difference between groups with prehospital antipyresis was χ2=31.5; df=10; P=.0005.
The predominating prescription pattern at discharge in children that had received prehospital antipyretic treatment was: for infants, continuation of the agent prescribed at hospital and addition of one or more others; for preschoolers, addition or switching of antipyretic agents; and for schoolchildren and adolescents, switching to another agent. At discharge, 86.7% (157/181) of the patients were prescribed one or more antipyretics; 55.4% were prescribed a combination of two agents, 40.7% a single agent; and 3.8% (6/157) three agents. The antipyretic most frequently prescribed as monotherapy was paracetamol (52.6%), prescribed in 72.4% of infants, followed by ibuprofen (34.6%). The antipyretic most frequently prescribed in combination was ibuprofen (48.4%) (Fig. 1).
We found that antipyretics were used very frequently prior to visiting the emergency department. Although the use of paracetamol or ibuprofen (alone or in combination) was most prevalent,6 we also found combinations of up to three agents for which the efficiency and safety have not been demonstrated. The use of physical methods, as recommended in different GCPGs, predominated in the emergency room;2,3 however, prescription of antipyretics not previously used and of agents like metamizole (banned in developed countries) to schoolchildren and adolescents was also common. The current recommendations are the use of monotherapy by the oral route and educating parents on the benefits of fever and its adequate control.1,2 The major finding in our study was the change in the prescription of antipyretics at discharge to the home. Contrary to what we expected, at discharge most patients were prescribed an additional antipyretic or an antipyretic other than the one that had been used to control the fever. This may be interpreted as anxiety on the part of both parents and doctors, so better communication and education on warning signs, and not only on the control of body temperature, would be advisable. Our results need to be confirmed by studies performed in other locations and under different conditions.
Please cite this article as: Velasco Aznar A, Rendón-Macías ME, Iglesias-Leboreiro J, Bernárdez-Zapata I. Uso de antipiréticos en urgencias pediátricas. An Pediatr (Barc). 2015;82:268–271.