Sickle cell disease is an inherited monogenic disease. The most frequent form is due to a homozygous mutation in the βS allele that encodes haemoglobin S.1 Its clinical course, while highly variable, is characterised by chronic haemolytic anaemia and vaso-occlusive events leading to early multiorgan failure.2
We present the case of a 7-month-old infant who was brought to the emergency department because of swelling in the left hand, with no evidence of preceding trauma, preserved spontaneous movement and no fever. The family was from Equatorial Guinea and the patient had resided in Spain since birth. The pregnancy, delivery and neonatal period had passed without complications. The patient was up to date with the routine immunisation schedule and had not been vaccinated against pneumococcus. There was no family history of interest.
The physical examination showed that the patient was stable, with appropriate anthropometric values and vital signs. He had swelling in the dorsal aspect of the left hand that was tender to palpation, with no other signs of inflammation; examination of the remaining organ systems was normal.
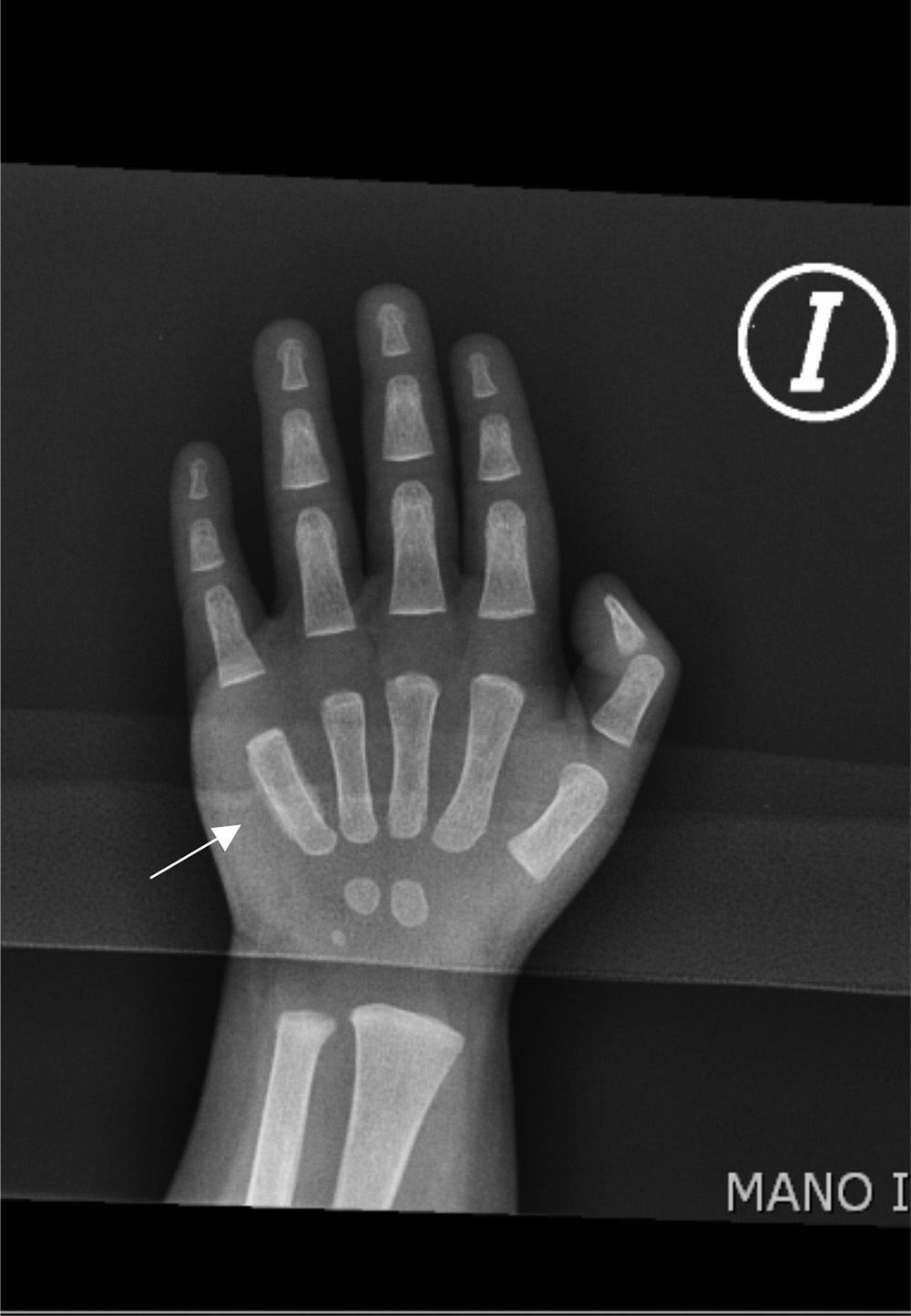
An initial radiographic examination (Fig. 1) revealed a periostic reaction at the fifth metacarpal bone.
At this point, the differential diagnosis included bone tumour, osteomyelitis and bone infarction in the context of sickle cell disease. Laboratory analyses revealed a regenerative microcytic anaemia (haemoglobin [Hb]: 8.6g/dL, mean cell volume70fL, reticulocytes 7.4%), with normal values for the rest of the complete blood count; normal coagulation, negative direct and indirect Coombs tests, normal bilirubin and haptoglobin levels, lactate dehydrogenase 706Ul/L, and a normal iron panel; the morphological study of red blood cells revealed sickle cells. Serological tests for CMV, treponema, HIV, HCV, EBV and VZV were negative, and the patient tested negative for antiHBc and HBSAg and positive for antiHBs; the urine test was normal. In light of the results of the diagnostic tests and the suspicion of sickle cell disease and dactylitis, intravenous fluid therapy and analgesic treatment with paracetamol were initiated. On the second day after admission the diagnosis was confirmed by analysis of haemoglobin variants (HPLC) (HbF: 26.9%; HbA2: 2.1%; HbS: 50%). Prophylaxis with penicillin was initiated, and the patient was given the pneumococcal vaccine (Prevenar 13®). The patient had a favourable outcome with gradual resolution of the local inflammatory signs.
Dactylitis, or hand-foot syndrome, is an episode of vaso-occlusive pain in small bones of the hands and feet that typically develops in children younger than 4 years with sickle cell disease, as at later ages the haematopoietic tissue in these locations is replaced by fibrous connective tissue and fat.3 Vaso-occlusive bone pain often constitutes the onset of sickle cell disease. It presents with pain and oedema, and is often accompanied by mild erythema and low-grade fever.4 Radiographic examination usually only shows a soft tissue oedema in the early stages, and may show bone abnormalities at a later stage. Osteomyelitis and cancerous conditions must be considered in the differential diagnosis, as they have similar clinical and radiological features, and their differentiation is crucial considering how differently these conditions are managed. The development of dactylitis in the first year of life, along with severe anaemia and leukocytosis in the first 2 years of life, has been described by some authors as predictors of severe disease associated with adverse events (acute chest syndrome, frequent pain crises, stroke or death). Its treatment involves hydration and pain management.5
Our patient was readmitted 15 days later due to a 2-day history of fever with concomitant vomiting and diarrhoea without pathological products. The general health status was fair, with asthenia, pallor, and mild dehydration. The most salient features of the examination were a splenomegaly of 3cm in the absence of hepatomegaly and hyperactive bowel sounds. Laboratory analysis revealed the following levels: Hb 4g/dL (previous value: 8.1g/dL), platelets: 75000mm3 (previous: 207000mm3), leukocytes: 20500mm3 (neutrophils: 9200mm3). The comprehensive metabolic panel was normal. The levels of C-reactive protein and procalcitonin were 48.9mg/L and 4.57ng/mL, respectively.
Since severe splenic sequestration was suspected, an urgent transfusion of red blood cell concentrate was performed, and intravenous (IV) rehydration therapy and empirical treatment with IV ceftriaxone were initiated.6 The patient had a favourable outcome, as he did not require further transfusions and his platelet levels recovered.
After 6 days of receiving ceftriaxone and obtaining negative blood, urine and stool culture results and a positive result for rotavirus, intravenous antibiotic treatment was discontinued and prophylactic treatment with penicillin resumed.
This patient is being treated with chronic exchange transfusions to maintain HbS levels below 30% (carrier levels) and is a candidate for splenectomy at 2 years of age to prevent recurrence, a measure that is still controversial but that is approved by current guidelines.
Please cite this article as: Solé-Ribalta A, Vilà-de-Muga M, Català-Temprano A, Luaces-Cubells C. Dactilitis, debut precoz de drepanocitosis y predictor de mal pronóstico. An Pediatr (Barc). 2015;82:267–268.