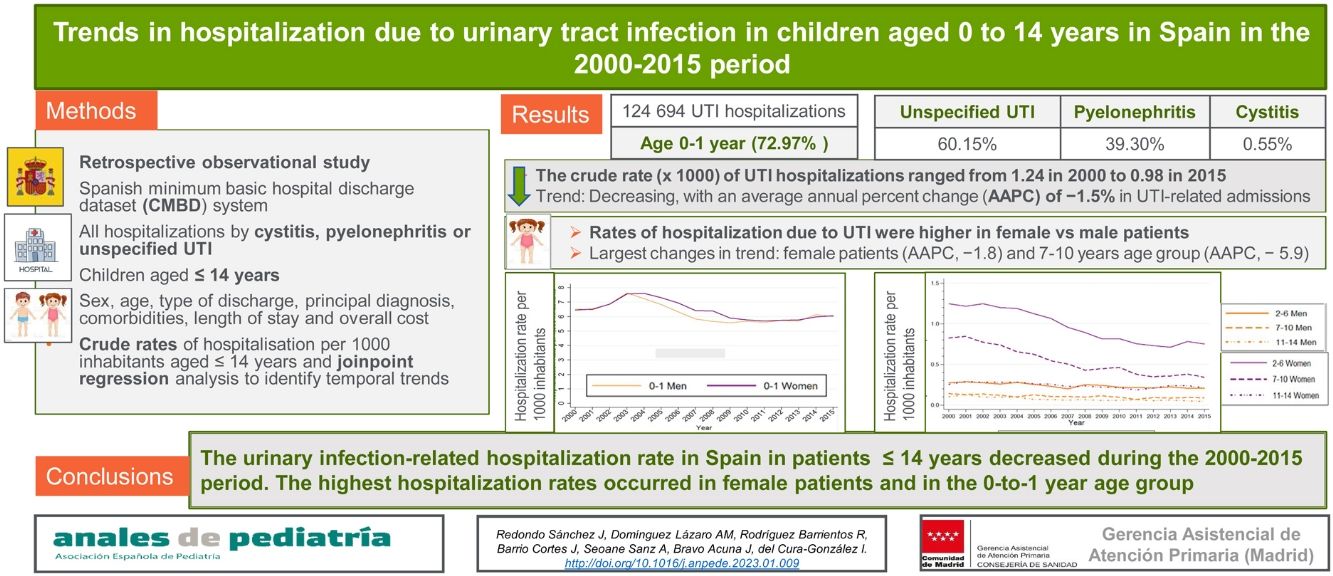
To analyse the trends in hospital admissions related to urinary tract infection among children aged 0–14 years in Spain in the 2000–2015 period.
MethodsWe conducted a retrospective observational study using the minimum basic hospital discharge dataset system of Spain, which applies the International Classification of Diseases, version 9 (ICD-9) coding system. We included every hospitalisation due to cystitis, pyelonephritis and unspecified UTI among children aged less than 15 years. We collected data on patient sex and age, type of discharge, main diagnosis, comorbidities, length of stay and overall cost. We calculated crude hospitalization rates per 1000 inhabitants aged less than 15 years and performed a joinpoint regression analysis to identify temporal trends.
ResultsIn the 2000–2015 period, there were 124 696 hospitalizations in children under 15 years. Of these patients, 72.97% were aged 0–1 year and 60.12% had a diagnosis of unspecified UTI, 39.27% of pyelonephritis, and 0.52% of cystitis. The crude rate of hospitalization due to UTI ranged from 1.24 in year 2000 to 0.98 in 2015. The rate of hospitalization was higher in female versus male patients. The joinpoint analysis found a decreasing trend in the rate of hospitalization due to UTI, with an average annual percent change (AAPC) of −1.5% (95% confidence interval [CI], −2.4 a −0.6). The largest decreases occurred in female patients (AAPC, −1.8; 95% CI, −2.5 a −1.0) and children aged 7–10 years (AAPC − 5.9; 95% CI, −6.7 a −5.2).
ConclusionsThe rate of hospitalization related to UTI in Spain in patients aged up to 14 years decreased during the 2000–2015 period. The highest hospitalization rates occurred in female patients and in the 0-to-1 year age group.
Analizar las tendencias en la hospitalización por infección del tracto urinario (ITU) en menores de 0−14 años en España en el período 2000–2015.
MétodosEstudio retrospectivo observacional realizado por medio del conjunto mínimo básico de datos (CMBD) hospitalario con códigos de la Clasificación Internacional de Enfermedades (CIE-9). Se incluyeron todos los ingresos por cistitis, pielonefritis e ITU de localización no especificada en niños menores de 15 años. Se recogieron datos sobre el sexo, edad, tipo de alta, diagnóstico principal, comorbilidades, estancia hospitalaria y coste total. Se calcularon tasas crudas de hospitalización por 1000 habitantes menores de 15 años y se llevó a cabo un análisis de regresión segmentada para identificar tendencias temporales.
ResultadosEn el período 2000–2015, hubo 124 696 ingresos en niños menores de 15 años. De este total, el 72,97% tenían de 0 a 1 año y el 60,12% recibió un diagnóstico de ITU no especificada, el 39,27% de pielonefritis, y el 0,52% de cistitis. La tasa cruda de hospitalización por ITU osciló entre 1,24 en 2000 y 0,98 en 2015. La tasa de hospitalización por ITU fue mayor en niñas que en niños. El análisis de regresión segmentada mostró una tendencia decreciente en la tasa de hospitalización por ITU, con un porcentaje de cambio anual medio (PCAM) en la −1,5% (IC 95%: −2,4 a −0,6). Los cambios observados fueron mayores en niñas (PCAM − 1,8; IC 95%: −2,5 a −1,0) y en el grupo de 7 a 10 años (PCAM − 5,9; IC 95%: −6,7 a −5,2).
ConclusionesLa tasa de hospitalización asociada a infección urinaria en pacientes menores de 15 años en España descendió durante el período 2000–2015. Las mayores tasas se dieron en niñas y en menores de 2 años.
Urinary tract infections (UTIs) are one of the most frequent, recurrent and severe bacterial infections in paediatrics.1–4 Their prevalence and incidence vary according to age, sex, race, presence of anatomical or functional abnormalities, circumcision and immunity status.2,5,6
The clinical presentations of UTIs vary in severity from asymptomatic forms to severe presentations with bacteraemia, including acute pyelonephritis, acute cystitis or asymptomatic bacteriuria. This classification has been useful for diagnostic and treatment purposes. Although there are cases that cannot be easily categorized, this subdivision has been helpful for the purposes of diagnosis and clinical decision-making.7,8 However, in practice, these categories are difficult to assess clinically, especially in children aged less than 2 years.2,9,10
The prevalence of UTIs varies with age, peaking in young infants, toddlers and older adolescents.10 The global prevalence of UTIs in the paediatric population has been estimated at 5%, with an annual incidence of 3.1 cases per 1000 girls aged 0–14 years and 1.7 cases per 1000 in boys aged 0–14 years.11
Until 2 months post birth, the incidence of UTIs is approximately 5% in girls and 20% in uncircumcised boys.12,13 Thereafter, the age distribution of new cases of UTI is bimodal. The first incidence peak occurs in the first year of life (0.7% in girls and 2.7% in boys)12,13 and is related to the increase in the concentration of the bacterial flora in the skin that comes into contact with diapers and may enter and ascend the urethra.6 The other peak appears between ages 2 and 4 years, which corresponds to the toilet training stage.14–16 By 7 years, approximately 8% of girls and 2% of boys have had a urinary infection5,14,17,18 and at 16 years, 11.3% of girls and 3.6% of boys have had a urinary infection, a finding that is explained by the fact that sexual activity alters the bacteria near the urethral orifice and produces a maximum peak in prevalence.6,14,17,18 Over 30% of children that contract a UTI will have recurrent UTIs,10 a condition that is most frequent in children aged 2–4 year and especially in boys with high-grade vesicoureteral reflux.
The high prevalence of these infections, the difficulty in their diagnosis and the detection of underlying genitourinary anomalies make UTIs one of the main indications for paediatric hospitalization (45 000 admissions per year in the United States) and responsible for significant health care costs that have been increasing since 2000.4 Over the last few years, new recommendations have been introduced in diagnostic and therapeutic guidelines for paediatric UTI that may have achieved a decrease in hospitalizations.7
Although hospitalizations due to UTIs have been studied in the adult population,19 there are few epidemiological studies at the global level and none in Spain on the frequency of hospital admission due to UTI in the paediatric population. Our study aimed to analyse trends in hospitalization related to UTI among children aged 0–14 years, calculating the mean length of stay, associated costs and associated mortality in the 2000–2015 period in Spain.
Material and methodsWe conducted a retrospective observational study using the uniform hospital discharge dataset records of Spain, known as the Conjunto Mínimo Básico de Datos (CMBD), obtained through the Spanish Ministry of Health,20 a source widely used in epidemiological research.21–23 The CMBD database is a registry for Spanish hospitals that has collected data for up to 97.7% of discharges from public hospitals from the time it was instituted and gradually included data for private hospital discharges from 2005, reaching an overall coverage of 92% out of all hospitals in Spain by 2014. The study also applied the REporting of studies Conducted using Observational Routinely collected health Data (RECORD) guidelines (online supplemental material 1). This study in the population aged 0–14 years was part of a larger study in which hospitalization due to UTI was analysed in different age groups, so both share the same methodology.19
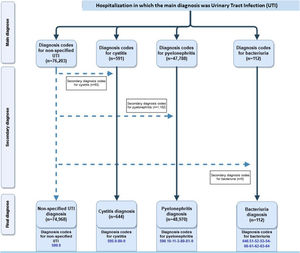
We searched the CMBD database to select hospitalizations between 2000 and 2015 in which the principal diagnosis was a UTI. For the purpose of the study, the term UTI encompassed the diagnostic codes for pyelonephritis (590.10-11-3-80-81-9), cystitis (595.0-89-9), bacteriuria (646.51-52-53-54-60-61-62-63-64) and UTI, site not specified (599.0) in the International Classification of Diseases, ninth version (ICD-9). Those hospitalizations with a principal diagnosis of unspecified UTI with a secondary diagnosis of pyelonephritis, cystitis or bacteriuria were reclassified as the latter to maximize the chances of identifying specific UTI diagnoses. For each hospitalization, we collected data on the patient’s sex and age, type of discharge, dates of admission and discharge, principal diagnosis, length of stay, and total cost. We classified all included patients according to age into 4 categories: 0–1 year, 2–6 years, 7–10 years and 11–14 years. We excluded cases of readmission, defined as admission to the same hospital within 30 days of discharge.19
We have expressed quantitative data as mean and standard deviation (SD) or median and interquartile range (IQR) and categorical data as absolute frequencies and percentages. We expressed crude hospitalization rates as hospitalizations per 1000 inhabitants aged 0–14 years, based on current population data as of July 1st each study year, obtained from the Instituto Nacional de Estadística (National Institute of Statistics) of Spain.19
We analysed temporal trends in the study variables by means of joinpoint regression, using age-adjusted UTI rates, with the 2015 population as the reference population. We estimated the annual percent change (APC) in each linear segment and the average annual percent change (AAPC), calculated as a weighted average of the model's APCs. When no join points were identified, the AAPC accurately reflected the APC. The analyses were conducted with the software Stata, version 14, and the National Cancer Institute joinpoint regression software, version 4.5.0.1.24
ResultsBetween 2000 and 2015, there were 124 694 hospitalizations among children under 15 years with a diagnosis of UTI; the diagnosis was UTI, site not specified in 60.12% of cases, pyelonephritis in 39.27% and cystitis in 0.52%. We revised these results by reviewing the records for hospitalizations with a principal diagnosis of unspecified UTI, taking into account the secondary diagnoses. Fig. 1 presents a flowchart of the hospitalizations and the diagnoses remaining at each data collection point, in accordance with the RECORD reporting guidelines.
Sociodemographic characteristics and clinical featuresOf the 124 694 hospitalizations, 72.97% corresponded to patients aged 0–1 year of age, and 57.49% to female patients. Unspecified UTI and pyelonephritis were more frequent in children aged 0–1 year and cystitis in children aged 2–6 years. Comorbidities accounted for less than 1% of each pathology. Neoplasia was the most frequent comorbidity (0.54%), followed by renal failure (0.13%), diabetes mellitus (0.09%) and vesicoureteral reflux (0.01%). The median length of stay was 5 days (IQR, 3−6). The median cost was 2272 euros (IQR, 1658−3078), with the highest costs corresponding to pyelonephritis and unspecified UTI. Table 1 presents the characteristics of the patients, overall and by disease.
Characteristics of patients and hospitalizations by type of UTI.
| Total (n = 124 694) | Unspecified (n = 74 968) | Pyelonephritis (n = 48 970) | Cystitis (n = 644) | ||||
|---|---|---|---|---|---|---|---|
| Male | Female | Male | Female | Male | Female | ||
| Age group* | |||||||
| 0−1 year | 90 987 (72.97%) | 32 420 (91.04%) | 28 778 (73.12%) | 13 632 (79.40%) | 16 006 (50.33%) | 75 (32.75%) | 76 (18.31%) |
| 2–6 years | 20 814 (16.69%) | 2164 (6.08%) | 6890 (17.51%) | 2114 (12.31%) | 9394 (29.54%) | 81 (35.37%) | 171 (41.20%) |
| 7−10 years | 8606 (6.90%) | 588 (1.65%) | 2618 (6.65%) | 859 (5.00%) | 4366 (13.73%) | 44 (19.21%) | 131 (31.57%) |
| 11−14 years | 4287 (3.44%) | 439 (1.23%) | 1071 (2.72%) | 564 (3.28%) | 2035 (6.40%) | 29 (16.66%) | 37 (8.92%) |
| Type of admission* | |||||||
| Urgent | 122 766 (98.45%) | 34 962 (98.18%) | 38 719 (98.38%) | 16 926 (98.58%) | 31 420 (98.80%) | 226 (98.69%) | 403 (97.11%) |
| Scheduled | 1900 (1.52%) | 642 (1.80%) | 629 (1.60%) | 240 (1.40%) | 372 (1.17%) | 3 (1.31%) | 12 (2.89%) |
| Comorbidity* | |||||||
| Neoplasm | 677 (0.54%) | 186 (0.52%) | 231 (0.59%) | 90 (0.52%) | 160 (0.50%) | 4 (1.75%) | 6 (1.45%) |
| Renal Failure | 157 (0.13%) | 51 (0.14%) | 28 (0.07%) | 48 (0.28%) | 28 (0.09%) | 1 (0.44%) | 1 (0.24%) |
| Diabetes mellitus | 114 (0.09%) | 12 (0.03%) | 38 (0.10%) | 9 (0.05%) | 53 (0.17%) | 1 (0.44%) | 1 (0.24%) |
| Vesicoureteral reflux | 15 (0.01%) | 3 (0.01%) | 2 (0.01%) | – | 7 (0.02%) | 3 (0.02%) | – |
| Length of stay** | 5 (3−6) | 5 (3−7) | 4 (3−6) | 5 (4−7) | 5 (4−6) | 3 (2−4) | 3 (2−4) |
| Length of stay* | |||||||
| 0−3 days | 35 249 (28.27%) | 10 128 (28.44%) | 13 387 (34.01%) | 3739 (21.78%) | 7544 (23.72%) | 140 (61.14%) | 263 (63.37%) |
| 4−7 days | 70 333 (56.40%) | 18 989 (53.32%) | 21 240 (53.97%) | 10 093 (58.79%) | 19 748 (62.10%) | 76 (33.19%) | 129 (31.08%) |
| 8−11 days | 15 836 (12.70%) | 5342 (15.00%) | 3992 (10.14%) | 2652 (15.45%) | 3820 (12.01%) | 7 (3.06%) | 18 (4.34%) |
| ≥12 days | 3276 (2.63%) | 1152 (3.23%) | 738 (1.88%) | 685 (3.99%) | 689 (2.17%) | 6 (2.62%) | 5 (1.20%) |
| Cost in euro** | 2272 (1658−3078) | 2313 (1658−3078) | 2075 (1620−3078) | 2313 (1658−3088) | 2075 (1658−3078) | 2075 (1658−2933) | 2002 (1619−2933) |
| Type of discharge* | |||||||
| Home | 123 589 (99.11%) | 35 308 (99.15%) | 39 024 (99.15%) | 16 971 (98.85%) | 31 540 (98.18%) | 229 (100%) | 412 (98.28%) |
| Transfer/Other/Unknown | 1080 (0.86%) | 295 (0.83%) | 322 (0.81%) | 195 (1.13%) | 258 (0.81%) | – | 3 (0.72%) |
| Fatality rate* | 25 (0.02%) | 8 (0.02%) | 11 (0.03%) | 3 (0.02%) | 3 (0.01%) | – | – |
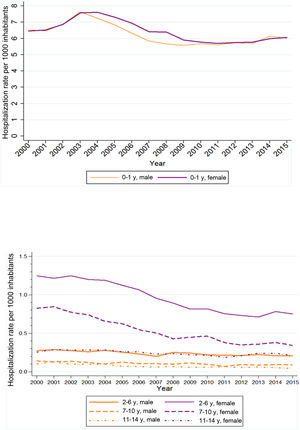
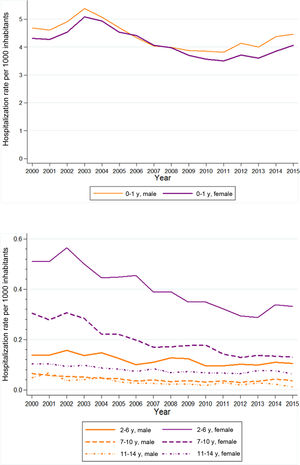
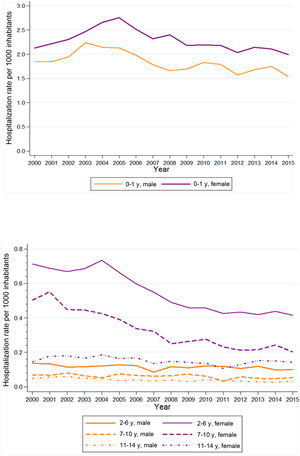
The crude rate of hospitalization due to UTIs in the 2000–2015 period ranged from 1.24 in 2000 to 0.98 in 2015. The rates were higher in female versus male patients in every age group except children aged 0–1 year (Fig. 2). In addition, when we analysed hospitalization rates by age group, we found the highest rates in the 0–1 year group, which also exhibited the greatest overall decrease in hospitalization rates of all age groups over the study period (Table 2).
Rate of hospitalization due to UTI by sex and age (2000–2015).
| TOTAL | 0–1-year-old | 2−6 years old | 7−10 years old | 11−14 years old | |||||
|---|---|---|---|---|---|---|---|---|---|
| Year | Male | Female | Male | Female | Male | Female | Male | Female | |
| 2000 | 1.24 | 6.54 | 6.45 | 0.28 | 1.25 | 0.14 | 0.83 | 0.10 | 0.25 |
| 2001 | 1.28 | 6.47 | 6.52 | 0.28 | 1.22 | 0.13 | 0.85 | 0.13 | 0.29 |
| 2002 | 1.35 | 6.88 | 6.86 | 0.28 | 1.25 | 0.13 | 0.77 | 0.10 | 0.28 |
| 2003 | 1.45 | 7.63 | 7.57 | 0.26 | 1.20 | 0.12 | 0.74 | 0.09 | 0.28 |
| 2004 | 1.44 | 7.24 | 7.61 | 0.28 | 1.19 | 0.10 | 0.66 | 0.10 | 0.28 |
| 2005 | 1.38 | 6.84 | 7.31 | 0.25 | 1.12 | 0.12 | 0.62 | 0.07 | 0.26 |
| 2006 | 1.30 | 6.33 | 6.94 | 0.23 | 1.06 | 0.10 | 0.55 | 0.07 | 0.26 |
| 2007 | 1.20 | 5.84 | 6.41 | 0.20 | 0.95 | 0.10 | 0.50 | 0.06 | 0.23 |
| 2008 | 1.19 | 5.66 | 6.39 | 0.25 | 0.89 | 0.10 | 0.43 | 0.06 | 0.24 |
| 2009 | 1.13 | 5.57 | 5.90 | 0.24 | 0.81 | 0.11 | 0.45 | 0.06 | 0.22 |
| 2010 | 1.10 | 5.69 | 5.77 | 0.22 | 0.82 | 0.10 | 0.46 | 0.06 | 0.21 |
| 2011 | 1.03 | 5.61 | 5.70 | 0.22 | 0.75 | 0.07 | 0.38 | 0.07 | 0.19 |
| 2012 | 1.02 | 5.73 | 5.75 | 0.21 | 0.73 | 0.09 | 0.35 | 0.05 | 0.21 |
| 2013 | 0.99 | 5.70 | 5.77 | 0.22 | 0.71 | 0.09 | 0.36 | 0.06 | 0.24 |
| 2014 | 1.01 | 6.14 | 5.98 | 0.21 | 0.78 | 0.09 | 0.38 | 0.05 | 0.24 |
| 2015 | 0.98 | 6.00 | 6.07 | 0.21 | 0.75 | 0.09 | 0.34 | 0.04 | 0.21 |
Rate of hospitalization given as cases per 1000 inhabitants.
As regards the different types of UTI, we found a decreasing trend in the hospitalization rate for each of them. In the case of unspecified UTIs, the rate per 1000 inhabitants decreased from 0.74 in 2000 to 0.62 in 2015. When it came to hospitalizations related to cystitis, the rate per 1000 inhabitants decreased from 0.01 in 2000 to 0.003 in 2015, while the rate of hospitalization related to pyelonephritis decreased from 0.48 in year 2000 to 0.35 in 2015 (online supplemental material 2).
Temporal trends in SpainJoinpoint regression analysis showed an AAPC of −1.5% in the frequency of hospitalization due to UTI (95% confidence interval [CI], −2.4 to −0.6). We observed 3 changes in the trend: a 1.8% increase between 2000 and 2004 (95% CI, −0.4 to 4.1), a −6.0% decrease between 2004 and 2009 (95% CI, −8.1 to −4.0) and a 0.3% increase between 2009 and 2015 (95% CI, −0.9 to 1.6) (online supplemental material 3).
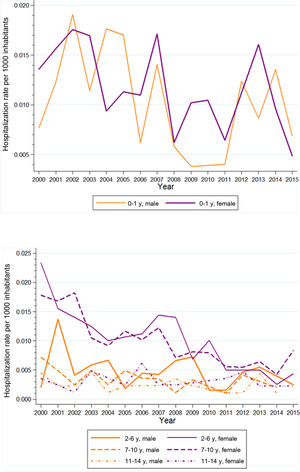
When it came to the types of infection, we found changing trends in hospitalizations related to unspecified UTI (Fig. 3) and related to pyelonephritis (Fig. 4). The APC for hospitalizations due to unspecified UTI was 3.7% between 2000 and 2003 (95% CI, −0.1 to 7.6), −5.2% between 2003 and 2010 (95% CI, −6.3 to −4.0) and 2.5% between 2010 and 2015 (95% CI, 0.7–4.2). On the other hand, the APC for hospitalizations due to pyelonephritis was 1.3% between 2000 and 2005 (95% CI, −0.6 to 3.3), −7.9% between 2005 and 2008 (95% CI, −15.5 to 0.3) and −1.5% between 2008 and 2015 (95% CI, −2.7 to −0.3). However, when it came to cystitis-related hospitalizations, we did not find any join points in the trend observed during the study period (Fig. 5) (online supplemental material 3).
The joinpoint analysis in which we used age-adjusted rates showed a decrease in the frequency of hospitalization due to UTI in both male and female patients, which was greater and only statistically significant in female patients (Fig. 2). The AAPC between 2000 and 2015 was −0.7% in male patients (95% CI, −1.5 to 0.0) and −1.8% in female patients (95% CI, −2.5 to −1.0) (online supplemental material 3).
When it came to the hospitalization rate for unspecified UTI, the AAPC from 2000 to 2015 was −0.5% in male patients (95% CI, −1.7 to 0.7) and −1.3% in female patients (95% CI, −2.2 to −0.4), and was only statistically significant in the latter (Fig. 3) (online supplemental material 3).
As for pyelonephritis-related hospitalizations, we also found a decreasing trend in patients of both sexes that was only significant in female patients (Fig. 4) (supplemental material 3). The AAPC from 2000 to 2015 was −1.3 in male patients (95% CI, −2.9 to 0.4) and −2.2%, a significant decreasing trend, in female patients (95% CI, −3.3 to −1.1).
In cystitis-related hospitalizations, the decreasing trend was statistically significant in patients of both sexes (Fig. 5) (supplemental material 3). The AAPC from 2000 to 2015 was −5.3% in male patients (95% CI, −8.8 to −1.6) and −7.5% in female patients (95% CI, −9.3 to −5.7).
Temporal analysis by age groupIn the period under study, we found the greatest decrease in the rate of hospitalization due to UTIs in children aged 7–10 years, with an AAPC of −5.9% (95% CI, −6.7 to −5.2). The decreasing trends corresponded to AAPCs of −0.3% in the 0–1 year age group (95% CI − 1.1 to 0.4), −0.3% in the 2–6 years group (95% CI, −1.1 to 0.4), −3.0% in the 7–10 years group (95% CI, −4.0 to −2.0) and −2.9% in the 11–14 years group (95% CI, −3.8 to −2.0). All the decreases were statistically significant except in the 0–1 year age group (online supplemental material 4).
Throughout the study period, the trends in hospitalization due to unspecified UTIs in different age groups were very similar, with a decreasing trend of −0.9% (AAPC − 0.2% in children aged 0−1 years [95% CI, −1.2 to 0.8], −2.4% in children aged 2−6 years [95% CI, −4.0 to −0.7], −5.8% in children aged 7−10 years [95% CI, −6.7 to −4.8] and −4.3% in children aged 11−14 years [95% CI, −5.6 to −3.0]), and the decrease was statistically significant in every age group except children aged 0–1 year (Fig. 3). The analysis identified 2 join points in the trends of hospitalization due to unspecified UTI in the 0-to-1 and 2-to-6 year age groups (in 2003 and 2010 and in 2002 and 2012, respectively) (supplemental material 4).
The trends by age group in hospitalization due to pyelonephritis were very similar, with a decreasing trend of −1.9% (AAPC of −0.4% in children aged 0−1 years [95% CI, −2.0; 1.2], −3.1% in children aged 2−6 years [95% CI, −4.9 to −1.3], −6.0% in children aged 7−10 years [95% CI, −6.8 to −5.1] and −0.7% in children aged 11−14 years [95% CI, −3.7 to 2.3]), changes that were statistically significant only in the 2-to-6 and 7-to-10 year age groups (Fig. 4). The analysis of the trends of hospitalization due to pyelonephritis identified 2 join points in the 0-to-1 and 2-to-6-year age groups (in 2004 and 2008 and in 2005 and 2008, respectively) (online supplemental material 4).
The trends by age group in hospitalization due to cystitis were very similar, with a decreasing trend of −6.9% (Fig. 5). The AAPCs from 2000 to 2015 were −4.5% in children aged 0–1 year (95% CI, −8.2 to −0.6), −8.0% in children aged 2–6 years (95% CI, −11.0 to −4.8) and −7.7% in children aged 7–10 years (95% CI − 9.5 to −5.8) with statistically significant changes in all 3 age groups. There were no AAPC data for the group aged 11–14 years (online supplemental material 4).
DiscussionMain findingsIn the 2000–2015 period, there were 124 694 recorded hospitalizations in children under 15 years of age, and we found a decrease in the hospitalization rate due UTIs, overall and for each type of UTI under consideration. Children aged 0–1 year were the age group with the highest hospitalization rate. Different guidelines on the management of UTI management in children under 2 years published throughout the study period agree on the criteria for hospitalization due to UTIs in children: age less than 2 or 3 months, presence of urinary system malformations or impaired renal function, septic appearance or dehydration (suspected or laboratory-confirmed), and intolerance of oral route of drug administration or lack of response to oral antibiotics within 48 h.25,26
Comparison with other studiesIn our study, the rate of hospitalization due to UTI was higher in female versus male patients than males through nearly the entire study period, except in the 0-to-1 year age group, in which the hospitalization rate was similar for both sexes during several periods.6 This finding is in agreement with other studies that found an increased incidence of UTIs in uncircumcised boys in the first year of life due to an increased risk of infection from foreskin contamination.4,6,27
The crude hospitalization rate decreased over time for all types of UTIs, with the most significant trend change taking place between 2003 and 2010. This trend is similar to what has been described in other countries, such as the United States,28 where a decrease in hospitalizations for UTIs has also been observed since 2003, although it was only statistically significant in the 2009–2012 period. This decrease in hospital admissions may be due to multiple causes, including changes in its management and a decrease in the incidence of ITUs.
In recent decades, febrile UTIs in children have been generally managed at the inpatient level. This practice is founded on the assumption that early intravenous antibiotic treatment offers an advantage in terms of rapid infection control. Since 1999, different clinical trials have demonstrated that oral antibiotic treatment of children with febrile UTIs is as effective as intravenous treatment in terms of clinical and bacteriological control of the infection29 and that oral and intravenous antibiotherapy is equally effective for treatment of pyelonephritis in children aged more than 1 month,30 leading to the recommendation of administering oral antibiotherapy between ages 1 and 24 months. Later, in 2011, the American Academy of Pediatrics included these recommendations in its guideline, thus reducing the number of cases in which the use of antibiotics delivered parenterally would be recommended.25 The same year, these recommendations were also included in the guidelines published by the Ministry of Health of Spain.31 Based on this evidence, the recommendation in favour of hospital admission for the management of paediatric patients with febrile UTIs has been restricted. The availability of a much less aggressive route of administration, such as the oral route, which allows outpatient treatment, is one of the causes that may explain the decreased rate of hospitalization observed in the study period. This directly affected children under 2 years, who were the target population of the updated recommendation but also probably, although to a lesser extent, all other age groups, by promoting the treatment of UTIs at the outpatient level.28 The authors of the study conducted in the United States after the changes made in 2011 proposed the same hypothesis to explain the greatest decrease in hospital admissions, observed in the oldest age group (15–17 years).
Another reason for the decreased hospitalization rate is the decreased incidence of UTIs, resulting from the change in diagnostic criteria, which have become more restrictive, and from improved prenatal diagnosis of urinary anomalies. In 2009, the diagnosis of UTI was based on a positive urine culture.7 Similarly, it is possible that improved prenatal detection of urinary anomalies and earlier detection of vesicoureteral reflux (VUR) have led to a decrease in UTIs in the paediatric population. In these cases, which carry a high risk of infection, antibiotic prophylaxis can be initiated early, which may have contributed to the decrease in UTIs in this group of patients. In our series, there were very few children with VUR.
From an epidemiological point of view, VUR is an important cause of UTI, although it is only an indication for hospital admission in the most severe cases (grades IV-V),1 a fact that may partly justify the low frequency of UTI associated with VUR in our study. We should also bear in mind potential documentation issues that may arise from the particular features of the CMBD database.
The CMBD is a secondary data source, and its quality may be conditioned by the quality of the hospital discharge reports and the accuracy of the coding, which can vary among health care facilities. However, the coding process has improved markedly since 2001, and the CMBD registry is considered valid for epidemiological studies such as this one. A limitation derived from the CMBD is that it does not allow identifying the type of treatment received by the patient or recurrent readmissions, as readmissions are only recorded in the first 30 days after discharge. As regards comorbidities, the CMDB allows a maximum of 14 diagnoses per patient (one main diagnosis and 13 secondary diagnoses). We do not expect that this limit would result in missing information in the paediatric age group.
We consider that the results obtained in this study are representative of hospitalizations for UTIs in Spain and show the temporal trends of UTIs at the national level over a period of 16 years, allowing an estimate of the burden of this disease in children aged less than 15 years and its impact on the national health system.
FundingThis study was funded by the Instituto de Salud Carlos III within the project PI19/01 700 in the framework of the National Plan of R+D+I 2017-2020, co-funded by the “A way of shaping Europe” European Regional Development Fund (ERDF). In addition, JRS has received a grant for the translation of this paper from the Fundación para la Investigación e Innovación Biosanitaria en Atención Primaria (FIIBAP).
Conflicts of interestThe authors declare not having any conflicts of interest to disclose.
Ethical considerations: approval and consentThe study was approved by the Ethics Research Committee of Hospital Fundación Alcorcon (20/125) and received a positive evaluation from the Central Research Commission of the Primary Care Administration of Madrid (57/20). The need for consent was waived by the ethics committee (20/125). The CMBD data were fully anonymized by the Ministry of Health before investigators gained access to them. The processing, communication and transfer of data was carried out in accordance with the pertinent guidelines and current regulations.
Author contributionsJRS and IDC conceived of the study and contributed to its design, acquired, analysed and interpreted data and directed the writing of the manuscript. RRR and ADL participated in the study design, the analysis and the drafting of the manuscript. JBC, ASS and JBA participated in the discussion of results and the drafting of the manuscript. All authors read and approved the final manuscript.
We thank Angel Gil de Miguel for his support in the acquisition of the data and in the development of the research.
We thank Laura Llamosas-Falco for her support in the analysis of the data and the elaboration and presentation of the manuscript.