Subungual exostosis is a benign bone tumour that develops in children and young adults. The slow growth of the spongy bone of the distal phalanx of the toe protrudes under the nail bed resulting in nail dystrophy. Clinically, it presents as a subungual hyperkeratotic tumour, which may or may not be painful, with inflammation or superinfection around the affected area. It develops in the toes, usually in sites subject to repeated trauma, such as the distal phalanx of the hallux or great toe.1
The differential diagnosis comprehends a range of conditions associated with onychodystrophy, such as onychomycosis, plantar warts or ingrown toenails. The mere suspicion of a tumour as the cause of ungual abnormalities can streamline the diagnosis and treatment. The diagnosis is made by plain radiography with two orthogonal projections, which allows visualization of the bony overgrowth (Fig. 1).
The treatment usually consists of the surgical excision of the exostosis from the distal phalanx under local anaesthesia combined with onychoplasty of the nail matrix. The patient was allowed to walk immediately after surgery and active rest was prescribed during recovery. The possible postoperative complications include wound infection or discomfort calling for the use of wider footwear until the sutures are removed.
We present our experience with this condition with the aim of offering paediatricians an action plan, including the recognition of the typical presentation, the required diagnostic tests and appropriate treatment and referral. To this end, we analysed a retrospective cohort of patients manage din our hospital between 2000 and 2022 through the review of health records, collecting data on the location of the tumour, time elapsed to diagnosis, number of specialists consulted, previous misdiagnoses and the histological findings in the surgical specimen. We also analysed the scores obtained one in an anonymous patient satisfaction and postoperative functioning survey (using the American Orthopaedic Foot And Ankle Society score) conducted by telephone, during which the patient (or the parents in the case of underage patients) provided verbal consent to participation in the study.
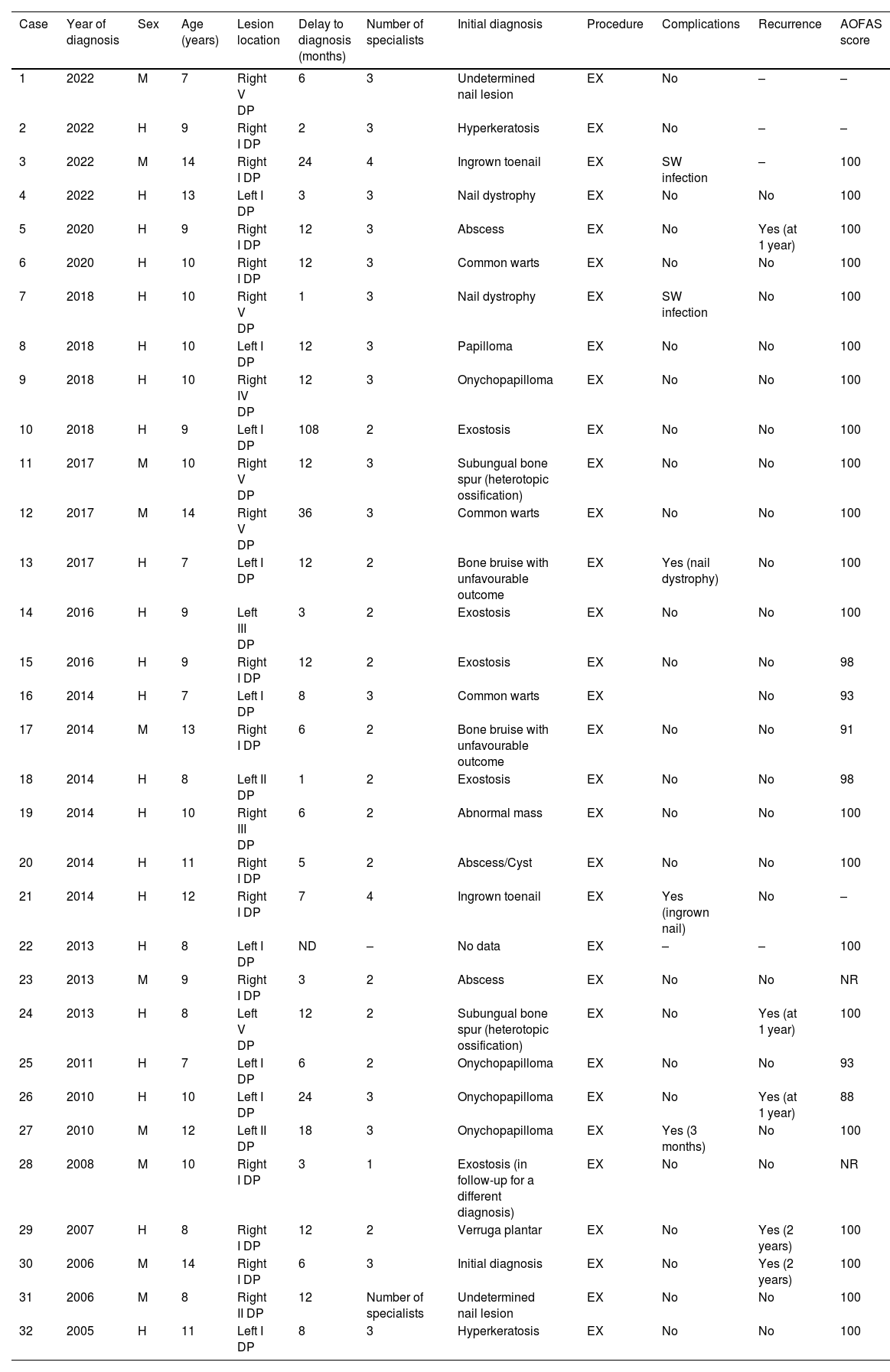
We entered the anonymised data for the 32 included patients in a table (Table 1). There was a predominance of male patients, lesions involving the right foot and lesions involving the first toe, with a mean age at the time of surgery of 9.88 years. The mean time elapsed to referral to the trauma department and the definitive diagnosis was 13.02 months.
Main characteristics of the patients.
| Case | Year of diagnosis | Sex | Age (years) | Lesion location | Delay to diagnosis (months) | Number of specialists | Initial diagnosis | Procedure | Complications | Recurrence | AOFAS score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2022 | M | 7 | Right V DP | 6 | 3 | Undetermined nail lesion | EX | No | – | – |
| 2 | 2022 | H | 9 | Right I DP | 2 | 3 | Hyperkeratosis | EX | No | – | – |
| 3 | 2022 | M | 14 | Right I DP | 24 | 4 | Ingrown toenail | EX | SW infection | – | 100 |
| 4 | 2022 | H | 13 | Left I DP | 3 | 3 | Nail dystrophy | EX | No | No | 100 |
| 5 | 2020 | H | 9 | Right I DP | 12 | 3 | Abscess | EX | No | Yes (at 1 year) | 100 |
| 6 | 2020 | H | 10 | Right I DP | 12 | 3 | Common warts | EX | No | No | 100 |
| 7 | 2018 | H | 10 | Right V DP | 1 | 3 | Nail dystrophy | EX | SW infection | No | 100 |
| 8 | 2018 | H | 10 | Left I DP | 12 | 3 | Papilloma | EX | No | No | 100 |
| 9 | 2018 | H | 10 | Right IV DP | 12 | 3 | Onychopapilloma | EX | No | No | 100 |
| 10 | 2018 | H | 9 | Left I DP | 108 | 2 | Exostosis | EX | No | No | 100 |
| 11 | 2017 | M | 10 | Right V DP | 12 | 3 | Subungual bone spur (heterotopic ossification) | EX | No | No | 100 |
| 12 | 2017 | M | 14 | Right V DP | 36 | 3 | Common warts | EX | No | No | 100 |
| 13 | 2017 | H | 7 | Left I DP | 12 | 2 | Bone bruise with unfavourable outcome | EX | Yes (nail dystrophy) | No | 100 |
| 14 | 2016 | H | 9 | Left III DP | 3 | 2 | Exostosis | EX | No | No | 100 |
| 15 | 2016 | H | 9 | Right I DP | 12 | 2 | Exostosis | EX | No | No | 98 |
| 16 | 2014 | H | 7 | Left I DP | 8 | 3 | Common warts | EX | No | 93 | |
| 17 | 2014 | M | 13 | Right I DP | 6 | 2 | Bone bruise with unfavourable outcome | EX | No | No | 91 |
| 18 | 2014 | H | 8 | Left II DP | 1 | 2 | Exostosis | EX | No | No | 98 |
| 19 | 2014 | H | 10 | Right III DP | 6 | 2 | Abnormal mass | EX | No | No | 100 |
| 20 | 2014 | H | 11 | Right I DP | 5 | 2 | Abscess/Cyst | EX | No | No | 100 |
| 21 | 2014 | H | 12 | Right I DP | 7 | 4 | Ingrown toenail | EX | Yes (ingrown nail) | No | – |
| 22 | 2013 | H | 8 | Left I DP | ND | – | No data | EX | – | – | 100 |
| 23 | 2013 | M | 9 | Right I DP | 3 | 2 | Abscess | EX | No | No | NR |
| 24 | 2013 | H | 8 | Left V DP | 12 | 2 | Subungual bone spur (heterotopic ossification) | EX | No | Yes (at 1 year) | 100 |
| 25 | 2011 | H | 7 | Left I DP | 6 | 2 | Onychopapilloma | EX | No | No | 93 |
| 26 | 2010 | H | 10 | Left I DP | 24 | 3 | Onychopapilloma | EX | No | Yes (at 1 year) | 88 |
| 27 | 2010 | M | 12 | Left II DP | 18 | 3 | Onychopapilloma | EX | Yes (3 months) | No | 100 |
| 28 | 2008 | M | 10 | Right I DP | 3 | 1 | Exostosis (in follow-up for a different diagnosis) | EX | No | No | NR |
| 29 | 2007 | H | 8 | Right I DP | 12 | 2 | Verruga plantar | EX | No | Yes (2 years) | 100 |
| 30 | 2006 | M | 14 | Right I DP | 6 | 3 | Initial diagnosis | EX | No | Yes (2 years) | 100 |
| 31 | 2006 | M | 8 | Right II DP | 12 | Number of specialists | Undetermined nail lesion | EX | No | No | 100 |
| 32 | 2005 | H | 11 | Left I DP | 8 | 3 | Hyperkeratosis | EX | No | No | 100 |
DP, distal phalanx (involved toe expressed in roman numerals); EX, excision-onychoplasty; SW, surgical wound.
Missing data noted with the symbol –.
The telephonic survey included a total of 27 participants, corresponding to 84.37% of the patients identified in the review. The mean score in the clinical rating scale was 98.55 (over 100), reflecting a good outcome in a majority of patients. None of the patients reported pain. Five reported deformities in nail growth during the follow-up that did not have an impact on postoperative functioning or patient satisfaction. All surgical specimens were diagnosed as osteochondroma resulting from bizarre parosteal osteochondromatous proliferation.2
Osteochondroma accounts for 33.4% of benign skeletal tumours and 10.1% of all bone tumours. When the tumour arises from the distal phalanx, it is more likely to affect the toes3 and present with subungual involvement, typically in children or adolescents, with a 2:1 male-to-female ratio. They most frequently involve the great toe, followed by the fifth toe, and are usually isolated lesions.4 It has been hypothesised that they are congenital tumours of very small size at birth5 whose presence becomes apparent as they develop during childhood. Subungual exostoses chiefly have a distal location and their cortical bone is continuous with the distal phalanx.6 Although the diagnosis and treatment were correct, the time elapsed from the initial related visit at the primary care level to the initial visit to the traumatologist was long, with a mean delay of more than 1 year.
Subungual exostosis is a condition that needs to be taken into account in paediatric primary care practice. Due to the nail changes that it entails, its morphological characteristics or the mere unawareness of the disease, the diagnosis may be delayed, involving several specialists, if it is not correctly suspected at the outset. If there is awareness and suspicion, a mere plain radiograph of the lesion with two orthogonal projections suffices to confirm the diagnosis. Once it is diagnosed, referral to a trauma specialist facilitates early treatment, which can achieve satisfactory clinical and cosmetic outcomes. Since these tumours are benign, the follow-up is relatively short (until approximately 1 month after the patient has resumed normal activity, scheduling of subsequent check-ups as needed), with early resolution of the clinical manifestations.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the Section on Paediatric Trauma of the Hospital Universitario Miguel Servet and their valuable work in collaboration with the Department of Paediatrics of the Hospital Materno Infantil de Zaragoza.