We present the case of an infant aged 8 months who had received a diagnosis through imaging of muscular ventricular septal defect (VSD) of large size, measuring approximately 10 mm in diameter (Fig. 1 A–D), with slow weight gain (25th percentile) and features of congestion requiring treatment with diuretics. Despite the size of the defect and the young age of the patient, due to the difficulties posed by surgical closure, we attempted percutaneous closure with a self-expandable Konar MF occluder (Lifetech, China), the use of which is associated with lower incidence of atrioventricular block due to its flexibility and lower radial stress.1,2
(A)–(C) Transthoracic echocardiography images showing the muscular ventricular septal defect (arrows). (A) Parasternal long axis view. (B) Parasternal short axis view. (C) Apical 5 chamber view. (D) Computed tomography axial images obtained for planning the procedure. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; VSD, ventricular septal defect.
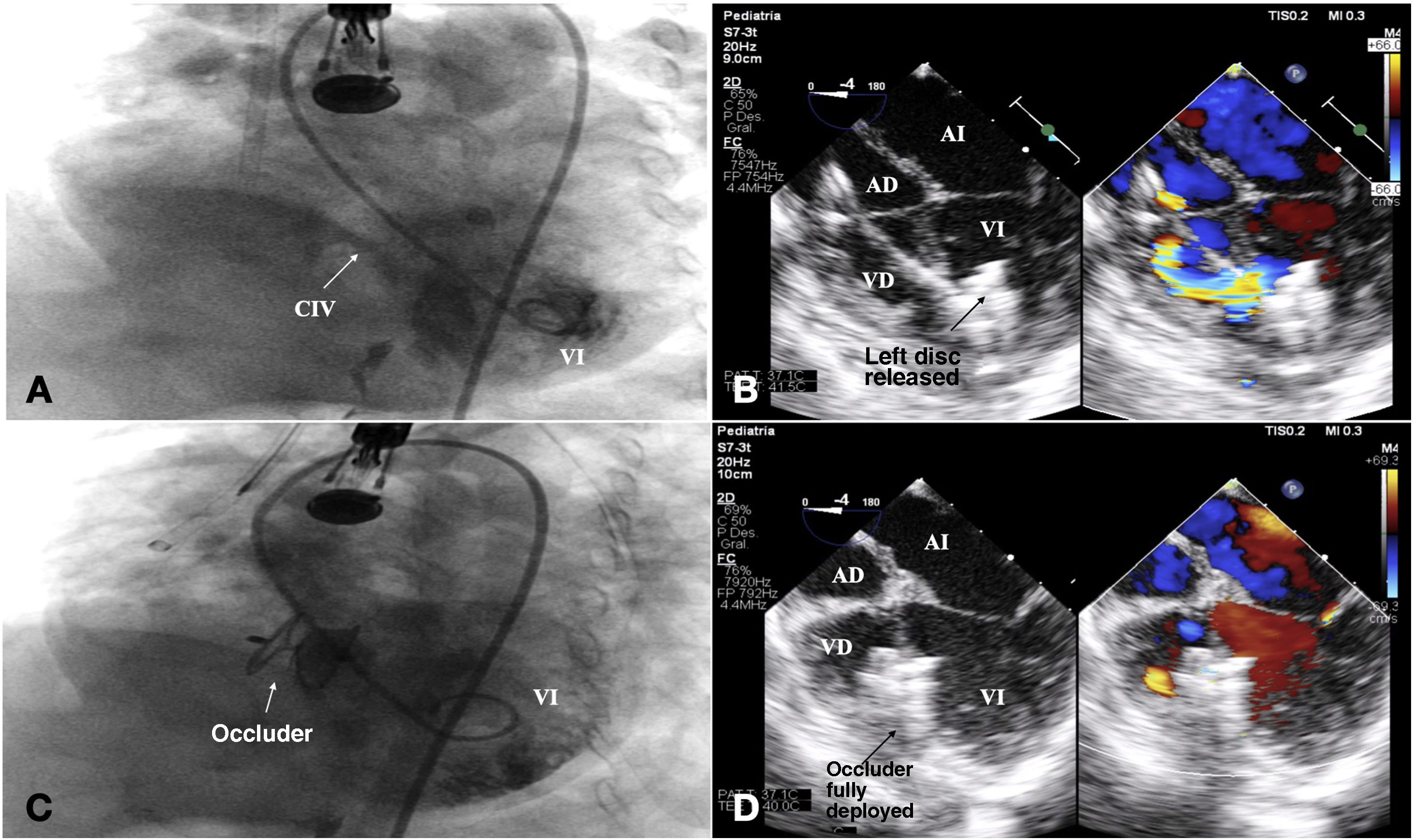
Access was obtained through the femoral artery and, the wire was advanced, crossing the defect with subsequent externalization to establish an arteriovenous loop was established. Then, a 7 F sheath was advanced to the ascending aorta, guided by transoesophageal echocardiography, through which a 14-mm Konar MF device was released gradually, achieving correct positioning and a stable fit over the ventricular defect without affecting adjacent structures (Fig. 2 A–D; Appendix A, video 1).
Percutaneous closure procedure. (A) Preoperative angiogram showing the muscular defect and flowing of contrast into the right cavities (arrows). (B) Transoesophageal echocardiogram 4-chamber view showing the release of the retention disc of the device. (C) Angiogram after the release of the device. (D) Transoesophageal echocardiogram 4-chamber view after implantation of the device showing mild residual shunt. LA, left atrium; LV, left ventricle; RA, right atrium; RV, right ventricle; VSD, ventricular septal defect.
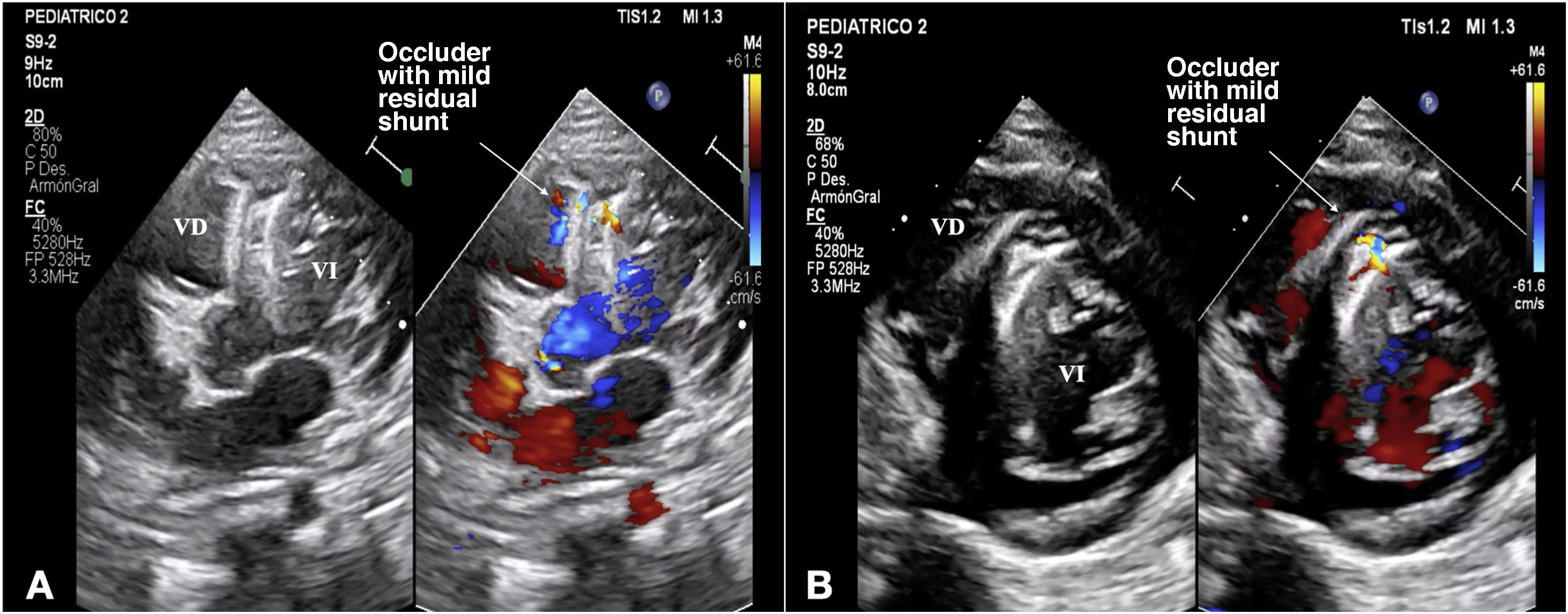
At 1 year of follow-up with repeated echocardiographic evaluations, imaging showed a small residual shunt (Fig. 3 A and B; Appendix A, videos 2 and 3), and the patient has exhibited significant clinical improvement, with catch-up growth (50th percentile) and no need of treatment with diuretics or hospitalization.