A female patient aged 15 years presented with epigastric pain and heartburn and evidence of gastro-oesophageal reflux (reflux index of 10.5% in pH monitoring) and oesophagitis grade A in the upper gastrointestinal (GI) endoscopy, compatible with peptic oesophagitis. Treatment was initiated with proton pump inhibitors (PPIs) at a dose of 40 mg/day for 2 months, which achieved improvement of symptoms.
The patient dropped out of follow-up and discontinued treatment, but made another visit 8 months later. She underwent an upper GI endoscopy that revealed, in the upper third of the oesophagus and 20 cm from the dental arch, an area of sloughing, whitish mucosa extending over ¼ of the oesophageal circumference (Fig. 1). The histological features (Fig. 2) were compatible with compatible con oesophagitis dissecans superficialis (ODS), prompting prescription of a 1-month course of high-dose PPIs (40 mg every 12 hours). Two months later, the follow-up upper GI endoscopy confirmed full macroscopic and histological normalization.
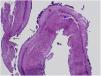
Histological section of proximal oesophagus (haematoxylin-eosin stain, ×4 magnification). Visualization of sloughed-off superficial mucosal layer composed of parakeratotic material with coagulative necrosis (red star), with space between the viable and the necrotic mucosa (blue star). The arrows point at bacteria adhered to the surface of the mucosa.
No evidence of viral inclusion bodies or fungal infection. The intraepithelial eosinophil count was greater than 15 per high-power field in every biopsy sample.
Oesophagitis dissecans superficialis is rare in children, and the paediatric literature on the subject is scarce. Its development has been associated with the use of certain medications1 and recent studies have found an association with oesophageal food impaction in the context of eosinophilic esophagitis.2,3 Whether ODS is a disease in itself or a histological sequela of toxic or contact injury has yet to be established.3
In conclusion, ODS could be considered a nonspecific endoscopic finding that can be found in the context of different forms of oesophageal mucosal damage and which has a benign natural history.