Childhood obesity is a high prevalence health problem. Although there are clinical guidelines for its management, there is variability in its clinical approach. The aim of this study is to describe the usual clinical practice in Paediatric Endocrinology Units in Spain and to evaluate if it resembles the recommended guidelines.
Material and methodsAn observational, cross-sectional and descriptive study was carried out by means of a questionnaire sent to paediatric endocrinologists of the Spanish Society of Paediatric Endocrinology. The questions were formulated based on the recommendations of “Clinical Practice Guidelines on the Prevention and Treatment of Childhood Obesity” issued by the Spanish Ministry of Health.
ResultsA total of 125 completed questionnaires were obtained from all Autonomous Communities. Variability was observed both in the number of patients attended and in the frequency of the visits. The majority (70%) of the paediatricians who responded did not have a dietitian, psychologist or psychiatrist, in their centre to share the treatment for obese children. As regards treatment, dietary advice is the most used, and 69% have never prescribed weight-loss drugs. Of those who have prescribed them, 52.6% did not use informed consent as a prior step to them being used.
ConclusionsThere are few centres that comply with the recommendations of the clinical practice guidelines on prevention and treatment of childhood obesity as an established quality plan. Clinical practice differs widely among the paediatric endocrinologists surveyed. There are no uniform protocols of action, and in general there is limited availability of resources for the multidisciplinary treatment required by this condition.
La obesidad infantil es un problema de salud de alta prevalencia. Aunque existen guías clínicas para su manejo, la variabilidad en su abordaje clínico es un hecho. El objetivo de este estudio es describir la práctica clínica habitual en unidades de Endocrinología Pediátrica y evaluar su adecuación a la guía recomendada.
Material y métodosSe realizó un estudio observacional, transversal y descriptivo mediante encuesta a endocrinólogos infantiles de la Sociedad Española de Endocrinología Pediátrica. Las preguntas fueron formuladas en base a las recomendaciones de la «Guía de Práctica Clínica sobre la Prevención y el Tratamiento de la Obesidad Infantojuvenil» del Ministerio de Sanidad español.
ResultadosSe obtuvieron 125 encuestas de todas la Comunidades Autónomas. Se observó variabilidad en el número de pacientes atendidos al mes y en la frecuencia de las visitas. El 70% de los encuestados no dispone de un nutricionista ni de psicólogo o psiquiatra al que derivar los pacientes. En el tratamiento, las medidas dietéticas son las más empleadas; un 69% nunca ha prescrito fármacos para perder peso. De los que prescriben, el 52,6% no utilizan el consentimiento informado como paso previo a su empleo.
ConclusionesPocos centros cumplen las recomendaciones de la Guía de Práctica Clínica sobre la Prevención y el Tratamiento de la Obesidad Infantil en un plan de calidad establecido. La práctica clínica difiere mucho entre los endocrinólogos pediátricos encuestados, sin existir protocolos unificados de actuación, y con escasa disponibilidad de recursos para el tratamiento integral que precisa esta enfermedad.
The World Health Organization has labelled obesity as “the 21st century epidemic.” In recent decades, there has been a progressive increase in the prevalence of obesity with a negative impact on morbidity, mortality, quality of life and health care costs,1,2 and childhood obesity is associated with an increased risk of obesity in adulthood.3,4 Comorbidities may be present from the first years of life, and patients often present with several risk factors for cardiovascular disease.5,6 Furthermore, obese children use health care services more than children with normal weight.7 Therefore, preventive interventions must be implemented at the family, school, health care and community levels to promote healthy lifestyle habits and behavioural changes in regards to diet and physical activity, along with the measures taken to manage obesity and its comorbidities.8–10
While evidence-based guidelines and protocols for the management of childhood obesity have been developed, there is insufficient data on the challenges met in their implementation, which will vary by health care setting. The aim of our study was to describe the approach of paediatric endocrinologists to the clinical management of childhood obesity, with emphasis on differences in management between levels of care.
Materials and methodsStudy design and participantsWe conducted a cross-sectional observational and descriptive study on the approach to the management of childhood obesity in clinical practice using a 20-item questionnaire with multiple choice answers. The questionnaire was distributed through the webpage of the Sociedad Española de Endocrinología Pediátrica (Spanish Society of Paediatric Endocrinology [SEEP]), and we sent a message to all members through its mailing list explaining the purpose of the study and emphasising the importance of their participation. The target population comprised 253 paediatricians members of the SEEP and engaged in clinical practice in Spain. Questionnaires were completed in November and December 2014. Participation required the consent of respondents, for which we informed potential participants of the purpose of the study, its methodology, and the anonymization of all collected data.
Variables under studyThe dependent, independent and confounding variables were included in the 20 items of the survey, following the recommendation of the Clinical Practice Guideline for the Prevention and Treatment of Obesity in Children and Adolescents of the Ministry of Health.8 We grouped them in six modules: health care setting (items 1 and 2), initial assessment and follow-up visits (items 3–6), lifestyle and dietary measures (items 7, 8 and 9), psychological intervention (items 10, 11 and 12), pharmacological treatment (items 13–16) and failure of conservative treatment/surgical intervention (items 17–20). Depending on their nature, variables were quantitative or categorical, and depending on how they were measured, nominal polytomous, nominal dichotomous or ordinal. Table 1 shows the possible values assigned to each variable and their division into different modules.
Variables included in the survey addressed to paediatricians members of the Sociedad Española de Endocrinología Pediátrica.
| Variable | Answer options |
|---|---|
| Type of health care setting | Private clinic, primary care, secondary or tertiary care level hospital |
| Autonomous community where you practise | Andalusia, Aragon, Asturias, Balearic Islands, Canary Islands, Cantab ria, Castilla La Mancha, Castilla Leon, Catalonia, Extremadura, Galicia, La Rioja, Madrid, Murcia, Navarre, Basque Country, Autonomous Community of Valencia |
| Average number of patients with obesity you manage per month | Fewer than 10, 11–20, 21–30, more than 30 |
| On average, how many patients a month do you see for the first time in relation to obesity? | Fewer than 10, 11–20, 21–30, more than 30 |
| How many minutes do you devote to a patient that is having their first visit related to obesity? | Fewer than 10, 11–20, 21–30, more than 30 |
| How frequently do you schedule subsequent evaluations with your obese patients? | More than once a month, monthly, every 3 months, every 4 months, every 6 months, every 9 months, depends on the condition of the patient |
| What type of dietary intervention do you use most often? | Depends on type of obesity, individualised diet, low-calorie diet, restriction of carbohydrates with a high glycaemic index, modifications to the usual diet, all of the above |
| Is there a licensed nutritionist you can refer your patients to? | Yes/No |
| Who is responsible for providing nutrition education? | Paediatrician, paediatric endocrinologist, nurse, paediatrician and nurse, paediatrician and nutritionist, health educator, no one |
| Is a psychologist or psychiatrist available to provide care to patients with obesity? | Yes/No |
| Is there a protocol for behavioural therapy? | Yes/No |
| Who provides behavioural therapy? | Paediatrician, psychologist or psychiatrist, paediatrician and psychologist/psychiatrist, nurse, educator, multidisciplinary team, no one |
| Have you ever prescribed pharmacological treatment to your patients to help them lose weight? | Yes/No |
| If you answered yes to the previous question, check which of the following you use or have used | Metformin, orlistat, topiramate, antidepressants |
| Do you obtain informed consent when you prescribe these drugs? | Yes/No |
| What other types of nutritional intervention do you use, if any? | Dietary fibre, conjugated linoleic acid (CLA), multivitamins, guidelines of the Niñ@s en movimiento (“Children on the move”) programme, tryptophan, none |
| When the above measures are ineffective, what other types of intervention do you use? | Discharge, hospital admission for multidisciplinary treatment, referral to psychology or psychiatry, referral to different facility, referral to social services, persist in current treatment, referral to surgery, change in strategy, use of specific programme, none |
| Does your facility offer the option of bariatric surgery? | Yes/No |
| If so, which is the surgical intervention used most frequently in your facility? | Gastric balloon insertion, adjustable gastric band, gastric bypass, sleeve gastrectomy, does not know/does not answer |
| How many patients have you referred for bariatric surgery? | None, 1–3, 4–6 |
We performed the descriptive analysis with SPSS (version 18.0). We used the contingency tables and the chi square test to compare the percentage distribution of different categories between qualitative variables, or, if the assumptions for testing were not met, the Fisher exact test. The null hypothesis that the variables were independent was rejected if the P-value was less than or equal to .05. We also calculated likelihood ratios as an alternative to the chi square statistic, with statistical significance still defined as a P-value of .05 or less. These two statistics may lead to the same conclusion, but in cases where they did not coincide, we opted to use the most conservative statistic (the one with the lowest P-value).
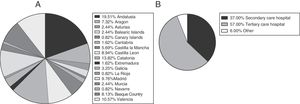
ResultsWe received 125 completed questionnaires, with representation of every autonomous community in Spain (Fig. 1A); 94% of respondents were employed in secondary or tertiary care level hospitals (Fig. 1B). The primary level of care is the point of entry to the health care system, the secondary level of care is the care delivered at regional hospitals (general medicine, general dental care, clinical laboratories, radiology, emergency care, inpatient care and low-complexity maternity care) and general hospitals (medical clinics, inpatient wards, basic emergency care, intermediate-complexity maternity care and caesarean sections, general and specialised dental care, outpatient nutrition, psychology and rehabilitation services), and the tertiary level of care is the care delivered in referral hospitals (advanced diagnosis and treatment of patients with complex diseases referred from primary and secondary level facilities).
The distribution of the number of visits related to obesity per month was similar for every level of care (Fig. 2A). We found differences between levels of care in the proportion of facilities that received more than 20 visits by patients with a new diagnosis of obesity. None of the respondents employed in a secondary level hospital reported having more than 20 new obesity patients a month, compared to 5.5% of respondents in tertiary level hospitals (P=.02) (Fig. 2B).
When it came to new patients, most respondents (67.2%) reported devoting between 15 and 30min to the first visit, and there were no differences based on level of care (Fig. 3A). As for the frequency of follow-up visits, 34% reported scheduling them “every 3 months”, 17% “every 6 months”, 15% “every 2 months”, 14% “monthly or more than once a month” and 11% “based on the patient's condition”.
We found a significant association between level of care and the frequency of follow-up evaluation of obese patients (P=.036). The proportion of respondents that scheduled monthly follow-up visits was 67% at the primary care level (with follow-up visits more than once a month in 11%), 15% at the secondary care level and 7% at the tertiary care level, while the proportion of respondents that scheduled follow-up visits every 6 months was 11% at the secondary care level and 23% at the tertiary care level (none of the primary care paediatricians reported scheduling follow-up evaluations at 6-month intervals).
Dietary interventionMost respondents adhered to current recommendations (Table 2), and we found no differences between levels of care, as almost all respondents reported making “modifications to the usual diet” and very few reported using “fixed low-calorie diets”.
Analysis of the adherence to the recommendations given in the sections “Intervention in Paediatrics”, “Psychological intervention” and “Bariatric surgery” of the Clinical Practice Guideline for the Prevention and Treatment of Obesity in Children and Adolescents.
| Recommendation | Secondary care | Tertiary care | P | ||
|---|---|---|---|---|---|
| Yes (%) | No (%) | Yes (%) | No (%) | ||
| Maintain a healthy and balanced diet in conforming to the healthy eating pyramid | 95.65 | 4.35 | 95.71 | 4.29 | .788 |
| The use of restrictive diets is not recommended | 4.35 | 95.65 | 4.29 | 95.71 | .788 |
| Guidance on dietary changes should be provided by health professionals habitually serving children and adolescents | 97.92 | 2.08 | 95.65 | 4.35 | .538 |
| Supportive psychological treatment (behavioural or cognitive-behavioural therapy) | 19.56 | 80.44 | 12.68 | 87.32 | .455 |
| Interventions for stress management and other psychological approaches Use of individual or group therapya | 27.66 | 72.34 | 35.29 | 64.71 | .389 |
| Informed consent must be obtained before prescribing treatment with any of the drugs included in the guideline | 35.71 | 64.29 | 54.17 | 45.83 | .272 |
| The use of alternative therapies is not recommended | 77.78 | 22.22 | 86.36 | 13.64 | .466 |
| Bariatric surgery may be suitable in adolescents with severe obesity (BMI>40kg/m2) and severe comorbidities, or with a BMI>50kg/m2, after failure of initial treatment with or without pharmacological treatmentb | 30.95 | 69.05 | 10 | 90 | .127 |
Seventy percent of respondents reported that a nutritionist was not available in their facility for referral of patients with obesity, and nutritionists were available more frequently in tertiary care hospitals compared to secondary care hospitals (Fig. 3B). We also found a statistically significant association between level of care and the availability of a nutritionist (P=.02). At any rate, in almost every facility, nutritional guidance was provided by staff devoted to the paediatric population (Fig. 3C and Table 2), although a small number of respondents reported that “no one” was tasked with providing nutritional guidance to these patients.
Psychological interventionOur findings were very discouraging, as most facilities (including tertiary care hospitals) lacked a specific protocol for behavioural therapy (Fig. 3D), with the further barrier of lacking staff trained in psychology to deliver such treatment (Fig. 3E). We also found no differences between levels of care in this variable (Table 2).
Pharmacological treatmentMost respondents (n=87) had never prescribed medication for weight loss, and we did not find differences on this aspect between levels of care. Orlistat and metformin, were used occasionally by 30.4% of respondents. Table 2 shows our findings regarding the adherence to the recommendation of obtaining informed consent before prescribing these drugs.
Surgical managementBased on the recommendations of the clinical practice guideline, surgery would only be indicated in very specific cases, and the decision to operate should be preceded by a multidisciplinary evaluation of the patient and take into account the subsequent need for lifelong follow-up. Our survey only explored the availability of bariatric surgery in the facilities under study and the respondents’ experience in referring patients, but we did not attempt to assess whether referral to surgery was made in adherence to recommendations. Sixty-five percent of respondents reported that bariatric surgery was not performed in their facility, while this option was available more frequently in tertiary care hospitals (Fig. 3F), although this trend was not statistically significant (P=.097). Of the 43 respondents that reported bariatric surgery was available in their facilities, 26 did not know the surgical technique used for the procedure. Only 21 of respondents reported having referred patients for surgery, and we found it interesting that the proportion of paediatricians that did so was greater in secondary level hospitals (13 of the 29 respondents employed in secondary care hospitals compared to 8 out of 72 employed in tertiary care hospitals), although the difference in proportions was not statistically significant (Table 2).
Alternative therapiesMost respondents adhered to the recommendation of abstaining from using alternative therapies, although 13% of respondents in tertiary care facilities and 22% in secondary care facilities reported using them (Table 2). Table 3 summarises the use of alternative therapies.
When it came to the approach to cases in which treatment was not effective, the majority of respondents reported taking no action (Table 4).
Approach to patients that do not respond to initial treatment.
| Type of intervention | Number of respondents that selected this option |
|---|---|
| Social services | 2 |
| Mental Health care unit health/psychologist/psychiatrist | 22 |
| I persist in the chosen treatment approach | 2 |
| Shift in approach | 16 |
| Referred to another facility | 11 |
| Admitted to hospital for multidisciplinary management | 20 |
| Admitted to specific programme in my facility | 1 |
| Referred to surgery | 2 |
| Discharge | 13 |
| No specific intervention | 42 |
| Does not know/answer | 12 |
Successful treatment of obesity depends on the training and approach of health care professionals as well as the availability of health care resources and the involvement of multidisciplinary teams.11 Despite the availability of clinical practice guidelines published in Spain and abroad with the aim of optimising health care for paediatric patients with obesity, we found considerable variability in the management of this condition among respondents.
The surveys found in the literature, such as the Encuesta Nacional de Salud (National Health Survey), were designed to determine the prevalence and incidence of obesity12 or addressed to general paediatricians and physicians.13,14 However, there are no studies describing real-life clinical practice in the management of paediatric patients with obesity by paediatricians specialised in endocrinology.
The response rate usually achieved in surveys of health care professionals by means of online questionnaires ranges between 17% and 51%.15,16 In our study, it was 49.4%, which is considered adequate based on studies regarding the response rate obtained in this type of online survey.17 Thus, we obtained a representative sample of paediatric endocrinologists in Spain, with respondents from every autonomous community and employed in every level of care.
Nearly 50% of respondents met with 10–30 patients a month for follow-up of overweight or obesity. These data were consistent with the increased prevalence of this disease in Spanish children and adolescents.18 There was variability in the number of patients managed by respondents, which may have been due to differences in the size of the catchment population, population density or health care infrastructure between autonomous communities.19,20
Most respondents reported spending 15–30min with each patient (67.5%), and 6% reported spending fewer than 10min. Based on current recommendations8–10 for the initial assessment and followup of these patients, which include a comprehensive anthropometric evaluation, psychological evaluation with exploration of family dynamics, and administration of questionnaires regarding dietary, physical activity and other lifestyle habits, an appointment duration of fewer than 30min seems insufficient, although there are no specific recommendations on the duration of appointments.
Few facilities had nutritionists on staff (29%), and these specialists were more frequently available in tertiary care hospitals. A nutritional assessment by professionals specialising in children with chronic disease is essential,1,10,21 and should be included in management protocols. This assessment is key to prevent potential complications, such as malnutrition, and to develop an appropriate treatment plan for each patient.
Our survey found very small differences in dietary management. Almost 89% of paediatricians made modifications to the current diet of the patient, and paediatricians were most frequently responsible for providing nutritional guidance. Studies on the effectiveness of dietary management have generally been of poor methodological quality, had short durations of followup, and had not assessed long-term weight loss,22 so at present we do not know which diet is most effective for management of overweight and obesity in the paediatric population,23–25 and low-glycaemic index diets with carbohydrate restriction seem to be as effective as low-calorie diets for short-term weight loss.26 In adults, a 15–30% reduction in energy intake compared to the previous diet is recommended based on baseline energy requirements.27 Actual clinical practice adhered to recommendations,28 as only 4% of respondents used fixed low-calorie diets, and 6.4% customised low-calorie diets for each patient.
Based on level B evidence, psychological support is recommended for the management of overweight and obesity in children and adolescents, as is the use of stress management interventions and other psychological approaches.29,30 However, in our survey, only 30% of respondents reported such support being available, and only 13.6% worked in facilities that had a behavioural therapy protocol. Contrary to what we expected, the proportion of paediatric endocrinologists that could refer patients to cognitive behavioural therapy was greater in those employed in secondary care hospitals, although we found no differences between levels of care in the proportion of facilities that had a child psychologist or psychiatrist on staff.
Psychotherapy is probably the area in which the management and follow-up of these patients is most deficient. It would be helpful to assess whether the recent official recognition of child psychiatry as a distinct specialty31 helps remediate this lack and raise awareness on the care needs of this population. In fact, an expert psychological evaluation is absolutely indispensable in morbidly obese adolescents in whom surgical treatment is being considered. Furthermore, recent studies have shown that the use of stress management interventions in the treatment of these patients is associated with a reduction in BMI and an improvement in depression and anxiety symptoms.32,33
Clinical practice guidelines do not recommend routine use of pharmacotherapy for treatment of obesity in children aged less than 12 years.8–10 In our study, 30% of respondents had prescribed drugs for treatment of childhood obesity. The drug prescribed most frequently was metformin, which has been found to achieve reductions in BMI of less than 5% in children with obesity and insulin resistance aged 10–14 years.34 Both metformin and orlistat are off-label drugs. The law35 stipulates that physicians must inform patients or their legal guardians of the benefits and risks of off-label drug use and obtain written informed consent for such treatment. However, 67% of respondents that prescribed drugs did not seek informed consent. Our findings were consistent with the 2012–2013 national survey on the use of these drugs in paediatrics practice.36
Based on our data, treatment of childhood obesity with bariatric surgery is nearly incidental, as few patients fulfil the eligibility criteria.37 Indeed, clinical practice guidelines both in Spain and abroad assert that bariatric surgery in the paediatric age group should be restricted to very specific and carefully selected cases.8–10 In addition, only 36% of facilities in our survey offered this surgery, which would explain why most paediatricians were not acquainted with the different bariatric surgery techniques. The technique used most frequently to date is gastric bypass, which achieves the greatest weight loss and on which the evidence is of higher quality.38 Some autonomous communities have stated a need to regulate bariatric surgery, including specific stipulations for surgery in adolescents.39
We also found differences as to the management of patients that do not respond to initial treatment: hospital admission (14.2%), referral to psychiatry or mental health services (12.8%) or discharge (43.2%), depending on the availability of different resources. However, only 12.8% reported referring these patients to psychiatry or mental health services, when one third report that these services are available to their patients. It is worth wondering whether there is any other disease in which over 40% of patients that do not respond to initial treatment would be discharged and considered to be treatment failures. Perhaps this percentage is this high because obesity is not quite considered a disease and because paediatricians may feel ineffective and discouraged in the treatment of obesity.13,40
Selection bias is one of the potential limitations affecting the relevance of our study, as we only analysed responses submitted by paediatricians members of the SEEP that chose to complete the questionnaire, and not having included other paediatricians specialised in the management of childhood obesity in other health care settings (primary care, gastroenterology or nutrition services, etc.).
There is also a risk of information bias due to the presence of incomplete responses and the limited number of variables under study. Thus, our study did not specifically assess interventions involving physical activity, as the Spanish health care system does not offer any services in this area, and such interventions are usually organised in the community, and sports activities offered by educational and recreational facilities.
Future research on this subject could include performance of the same survey on SEEP members to assess changes in current clinical practice, surveys of other paediatricians devoted to the management of obesity, who usually remain in the field, and also assessment of the success rate of treatment and the recommendations on physical activity or other interventions related to obesity that were not included in this study.
In conclusion, few paediatric endocrinology units adhere to the recommendations of the Clinical Practice Guideline for the Prevention and Treatment of Obesity in Children and Adolescents included in the quality assurance plan of the Public Health System of the Ministry of Health and Social Policy of Spain. The heterogeneity of clinical practice is probably due to a lack of standardised protocols and resources for the multidisciplinary management of these patients. Pharmacological treatment is rarely used in childhood obesity, and there is limited experience in bariatric surgery. We did not find many differences in the approach to childhood obesity between secondary and tertiary level hospitals, although the latter usually had larger caseloads of these patients and (at least reportedly) had nutritionists and/or psychologists on staff more frequently than secondary level hospitals. Thus, the care of paediatric patients with obesity falls to the paediatrician, as the multidisciplinary treatment approach has yet to be truly established in Spain.
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank the members of the Sociedad Española de Endocrinología Pediátrica (SEEP) for the trust bestowed on the Working Group on Childhood Obesity. We also thank the remaining members of the Working Group for their collaboration in writing this article: Albert Feliu, Francisco Javier Núñez, Rafael Ruiz, María Consuelo Sánchez and Amaia Vela.
Please cite this article as: Lechuga Sancho A, Palomo Atance E, Rivero Martin MJ, Gil-Campos M, Leis Trabazo R, Bahíllo Curieses MP, et al. Estudio colaborativo español: descripción de la práctica clínica habitual en obesidad infantil. An Pediatr (Barc). 2018;88:340–349.