In group A streptococcal (GAS) pharyngitis, a ten-day course of amoxicillin is recommended. However, short-course treatments seem to be equally effective. The aim of this study was to retrospectively evaluate and compare the outcome of patients treated with 7-day course and 10-day course of amoxicillin.
Materials and methodsRetrospective analysis of all GAS pharyngitis admitted to a pediatric emergency department in 2014. Demographic variables, the application and results of the rapid antigenic diagnostic test (RADT), treatment, complications and return in the next 30 days were analyzed. Two groups were defined for comparative analysis according to the duration of treatment with amoxicillin: A) short-course (up to 7 days) and B) long-course (10 days).
ResultsWere included 989 GAS pharyngitis. The median age was 5.2 years, 50.1% male. Amoxicillin was the most prescribed antibiotic (94.9%) with a median duration of 7 days. 10-day course therapy was prescribed in 31.9% of the cases. There were no differences between short and long-course treatment groups regarding age (p=0.600), gender (p=0.429) and complications (p=0.436). Considering the endpoint “return to the emergency department”, we concluded that up to 7 days of treatment was non-inferior to 10 days of treatment.
ConclusionThe most commonly prescribed antibiotic was amoxicillin, but a 10-day course was prescribed in few cases. In our analysis there seems to be no benefit with long-course treatments with amoxicillin in GAS pharyngitis.
En casos de faringitis por estreptococo grupo A (EGA) se recomienda una pauta de 10 días de amoxicilina. No obstante, parece que pautas de menor duración resultan igualmente efectivas. El objeto de este estudio fue evaluar y comparar de manera retrospectiva la evolución de pacientes tratados con pautas de amoxicilina de 7 y 10 días de duración.
Materiales y métodosAnálisis retrospectivo de todos los casos de faringitis por EGA atendidos en un servicio de urgencias en 2014. Se analizaron variables demográficas, uso y resultados de pruebas de detección rápida de antígeno (PDRA), tratamiento, complicaciones y reingreso en un plazo de 30 días. Se definieron 2 grupos para el análisis comparativo basados en la duración del tratamiento con amoxicilina: A) pauta corta (hasta 7 días), y B) pauta larga (10 días).
ResultadosSe incluyó a 989 casos de faringitis por EGA. La edad mediana fue 5,2 años, el 50,1% fue de sexo masculino. La amoxicilina fue el antibiótico más prescrito (94,9%), con una duración media de 7 días. Se prescribieron pautas de 10 días al 31,9% de los pacientes. No se encontraron diferencias entre los grupos con pautas cortas y largas en cuanto a la edad (p=0,600), el género (p=0,429) o las complicaciones (p=0,436). Concluimos que en lo referente a la variable de resultado «regreso al servicio de urgencias», la pauta de 7 días no es inferior a la de 10 días.
ConclusiónEl antibiótico prescrito con mayor frecuencia fue la amoxicilina, aunque solo se prescribió pauta de 10 días en unos pocos casos. Nuestro análisis no encontró beneficio aparente del tratamiento de larga duración con amoxicilina en casos de faringitis por EGA.
Acute pharyngitis is a very common upper respiratory tract infection in children. Its etiology is, in most cases and at any age, of viral origin, however it may have a bacterial cause. Group A streptococcus (GAS) is the most common bacterial agent, being responsible for about 20–30% of the total cases of acute pharyngitis in the pediatric age.1,2
The diagnosis of GAS pharyngitis based only on clinical criteria is unreliable.1 For a correct diagnosis of GAS pharyngitis, in order to avoid the inadequate prescription of antibiotics (AB), the rapid antigenic diagnostic test (RADT) or the oropharyngeal culture is recommended, except for cases of scarlet fever with the typical rash.3–5 Despite sensitivity of 70–90%, the RADT has a specificity of 95% or greater, so a positive result can obviate the need for culture which takes hours or even days to be available.1
Most international guidelines recommend the prescription of AB when GAS pharyngitis are confirmed by RADT and/or culture. Most of them advocate amoxicillin or penicillin as a first-line AB, since GAS has been universally susceptible to β-lactams.3 However, treatment failures have been reported from 12% to almost 40% in some regions of the world, perhaps because of the presence of β-lactamase-producing bacteria presented in the oral environment such as Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis, and anaerobes.6
Regarding the therapeutic with amoxicillin, a 10-day course therapy is recommended in order to obtain the highest rate of GAS eradication in the oropharynx, with a symptomatic improvement after 24–48h of treatment.3 However, there is evidence that short-course treatments, up to 7 days, seem to be equally effective with both clinical and bacteriological cure. These schemes seem to have more advantages such as increased therapeutic adherence and smaller costs of treatment.2,4,7–10
The aim of this study was to retrospectively evaluate and compare the outcome of patients treated with 7-day course and 10-day course of amoxicillin.
Material and methodsAn exploratory study was performed, with a retrospective analysis, through the consultation of the clinical processes, using SClínico® and PEM® (Electronic Medical Prescription). We included all GAS pharyngitis admitted to a pediatric emergency department (PED), during a 12 month period (January to December 2014). This general PED is the reference emergency for the central region of Portugal, with about 60 thousand attendances annually and with admission allowed until the age of 18 years.
All patients with the diagnosis of GAS pharyngitis or scarlet fever were included. A diagnosis of GAS pharyngitis was considered when there was a positive test or culture or in the presence of scarlet fever.
Patients with another concomitant diagnosis that justified the beginning of AB therapy and patients taking AB at the time of diagnosis were excluded.
We analyzed demographic variables, the application and results of the RADT, treatment with AB (type and duration), complications in the 5 weeks following the diagnosis (peritonsillar, parapharyngeal or retropharyngeal abscess, acute otitis media, sinusitis, acute rheumatic fever, poststreptococcal glomerulonephritis, Sydenham's chorea, poststreptococcal reactive arthritis or autoimmune neuropsychiatric disorder associated with GAS infections) and return to the PED in the next 30 days with a new episode of GAS pharyngitis and/or scarlet fever. Two groups were defined for comparative analysis according to the duration of treatment with amoxicillin: A) long-course (10 days) and B) short-course (up to 7 days).
Statistical analysis was performed using the SPSS® software version 23. The characterization of the population was performed by calculating measures of central tendency and dispersion for quantitative variables and by determining absolute and relative frequencies for qualitative variables. To compare nominal variables, chi-square or Fisher's exact tests were used respecting the Cochran rules. Regarding the numerical variables, the t-student (parametric sample) or U-Mann–Whitney tests (non-parametric sample) were performed after a normality test (Kolmogorov–Smirnov test). A level of statistical significance of 5% was considered.
Non-inferiority analysis for difference between proportions was made to compare group A and group B in regard to the number of patients that returned to PED, using a confidence intervals (CI) at the 95% confidence level and with the non-inferiority margin set to 10%.
ResultsDuring the study period, 2845 cases of acute pharyngitis were diagnosed. Of these, 1448 were excluded because they were considered viral pharyngitis, 103 were already under antibiotic therapy, 38 were diagnosed as having non-bacterial recurrent pharyngitis, 35 had another concomitant diagnosis requiring antibiotics, 25 due to incomplete medical records, and 6 due to chronic pathology with infectious risk.
There were 989 cases of GAS pharyngitis, of which 636 had positive RADT. In 185 cases there was a scarlet fever rash reported and in 168 cases, despite the rash, a RADT was performed being positive.
The median age was 5.2 years (IQR 8.4–3.3), 50.1% of male gender (n=495).
An oropharyngeal culture was done in a patient with allergy to amoxicillin in order to determine an alternative therapy based on the sensitivity test.
Amoxicillin was the most prescribed antibiotic, in 94.9% of the sample (n=939). The association amoxicillin-clavulanic acid was prescribed in 2.0% (n=20), macrolide (clarithromycin or azithromycin) in 1.9% (n=19) and cefuroxime in 0.6% (n=6). Clindamycin was prescribed to only one patient. The remainder were treated intravenously (n=4).
Amoxicillin treatment was prescribed for a median duration of 7 days (IQR10–7). In 52.6% (n=494) of the patients the treatment lasted for less or equal than 7 days. In 31.9% (n=300) of the cases it was prescribed for10 days.
According to the duration of treatment with amoxicillin, we separated the cases into two groups: group A) 10 days of treatment and group B) up to 7 days of treatment. Thus, 300 cases were included in group A and 494 cases in group B.
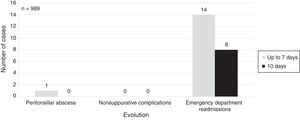
There was no differences regarding age (p=0.600), gender (p=0.429) or complications (p=0.436) – Fig. 1. A peritonsillar abscess was recorded in a patient of group B and no patient was subsequently admitted with acute rheumatic fever.
The number of patients that returned to the PED in the next 30 days by another episode of GAS pharyngitis was 22, being 2.7% (p1) of group A and 2.8% (p2) of group B – Fig. 1.
These 22 patients (50% male) had a median age of 5.0 years (IQR 6.6–3.8). They returned to the PED within a median of 6 days from the diagnosis (IQR 18–4) and all had a positive RADT in the second visit.
Amoxicillin was also the most prescribed antibiotic, in 77.3% (n=17), while amoxicillin-clavulanic acid was prescribed in 4 patients and a first generation cephalosporin in 1 case. Regarding those taking amoxicillin, the antibiotic was prescribed for 10 days in 11 cases, while in the remaining a 7 day course of antibiotic was recommended. In none of the cases, a new episode of GAS pharyngitis was reported in the following 30 days.
A non-inferiority analysis showed a CI (95%)=(−2.5%; 2.1%) for difference between proportions (p1–p2). Considering the non-inferiority margin of 10% and the lowest margin of −2.5%, we concluded that up to 7 days of treatment was no less effective than 10 days of treatment.
DiscussionIn the present study, the antibiotic of choice was amoxicillin, as recommended. Penicillin G, given as a single dose by intramuscular route, was never prescribed perhaps because of the good adherence and palatability of amoxicillin. In Portugal, oral penicillin is not available.3
The frequent prescription of AB by physicians is probably due to its effect on decreasing the duration of the symptoms, on reducing the infection transmission and decreasing the incidence of suppurative complications (otitis, sinusitis and peritonsilar abscess) and of acute rheumatic fever.1–3,7
However, contrary to what is recommended by international guidelines, a 10-day course with amoxicillin was only prescribed in 31.9% of cases. Despite this, when comparing the prescription of short and long amoxicillin regimens, there were no differences in the development of complications and in the return to PED due to a new episode of GAS pharyngitis.
In the literature, there are few studies comparing these two different amoxicillin regimens. A study published in 1981, performed by Schwarts et al., concluded that 10 days of treatment with penicillin was preferable because patients treated for 7 days had a significantly greater failure rate (31% vs 18%).11 In another study, Stromberg et al., concluded that within 1 week after completion of the antibiotic treatment there were significantly more failure treatment cases in the 5-day treatment group (27%) as compared with the 10-day group (6%).12 These authors did not evaluate a 7-day course of treatment. These studies had greater failure rates than ours.
In addition, a meta-analysis by Fagalas et al., in 2008, found that short antibiotic treatments for GAS pharyngitis were associated with lower rates of bacterial eradication than the ones found in the 10-day course treatment.13
However, other studies support our findings. In 1996, Cohen et al. compared the therapeutic regimen of amoxicillin for 6 days with penicillin V for 10 days in children with GAS pharyngitis, without statistically significant differences between the two regimens in relation to bacteriological relapse or GAS eradication rate at the end of four days. In addition, therapeutic adherence was significantly better within the amoxicillin group.10 Cochrane also published a review in 2012 that involved 20 studies and a total of 13.102 cases of GAS pharyngitis, with the objective of comparing short-course therapy (3–6 days) with 10-day course. Excluding studies with low doses of azithromycin, there was no significant difference in bacteriological or clinical recurrence, and short-course therapy presented a lower risk of early clinical failure. In this review there was also no statistical difference in the rate of long-term complications (acute rheumatic fever and post-infectious glomerulonephritis) between the two groups.9 However, these results were criticized for not including relevant trials and a meta-analysis. There were also methodological failures and insufficient statistical power to draw conclusions regarding the prevention of acute rheumatic fever.3,14
In our study, acute rheumatic fever was not observed, which is not surprising given the low incidence of this pathology in developed countries, and only one patient developed peritonsillar abscess following an episode of acute pharyngitis.
Other authors, as Petersen et al., attempted to evaluate the risk of developing acute rheumatic fever but failed because there were virtually no cases.15
There are several reasons that may explain why a new GAS pharyngitis occurred in the 22 patients who returned to the PED, such as non-adherence to previous treatment, a new contact with GAS or persistence of carrier state of GAS. The treatment failure is also a possibility.7 In this cases, we expected more frequent use of amoxicillin-clavulanic acid or a cephalosporin because recent administration of amoxicillin may increase the prevalence of beta-lactamase-producing bacteria, which may lead to treatment failure.6 The physicians must be alert to this results.
As limitations, we pointed out that the data collection was retrospective, being impossible to confirm if there was a strict compliance of the treatment's duration or if the patients looked for other appointments outside the hospital. Besides that, the studies presented in the literature are few and have different methods. Prospective studies are necessary.
ConclusionIn the present study, the antibiotic of choice was amoxicillin, but in few cases a 10-day course was prescribed. Considering the development of complications and the return to PED with new GAS pharyngitis in the next 30 days, there were no significant differences regarding the prescription of short or long amoxicillin courses. Thus, in this sample we can verify that there was no apparent benefit in the use of long-course of amoxicillin.
Conflict of interestsThe authors declare to have no conflict of interest.
Please cite this article as: Oliveira Pereira C, Ramos D, Mação P, Januário G, Januário L. Diagnóstico y tratamiento de la faringitis aguda. ¿Hay alguna ventaja en la pauta de antibióticos de 10 días?. An Pediatr (Barc). 2018;88:335–339.
Previous presentations: 34th Annual Meeting of the European Society for Paediatric Infectious Diseases, Brighton, United Kingdom, 12 May 2016.