Somatic complaints are common in childhood. Research has shown their relationship with emotional awareness and maladjustment. The study had three objectives: 1) to analyse the prevalence of somatic complaints; 2) to explore the relationships between the variables evaluated: somatic complaints, differentiating emotions, verbal sharing of emotions, not hiding emotions, body awareness, attending to others’ emotions, analysis of emotions, and personal, social, family, and school maladjustments; and 3) to identify predictors of somatic complaints.
Patients and methodsThe study included a total of 1134 randomly selected schoolchildren of both sexes between 10 and 12 years old (M=10.99; SD=0.88). The Somatic Complaint List, Emotional Awareness Questionnaire, and Self-Reported Multifactor Test of Childhood Adaptation were used to gather information.
ResultsThe results showed that the prevalence of somatic complaints was 90.2%, with fatigue, headache and stomachache being the most frequent. Dizziness and headache were more common in girls, and the frequency of complaints decreases with age. Somatic complaints are negatively related to emotional awareness, and positively related to maladjustment. The variables that contribute the most to the prediction of somatic complaints are personal maladjustment (25.1%) and differentiating emotions (2.5%).
ConclusionsThe study shows that personal maladjustment is the best predictor of somatic complaints; the more emotional awareness and better adapted the child, the fewer somatic complaints they lodge. Childhood is a stage with significant physical discomfort.
Las quejas somáticas son frecuentes en la infancia. La investigación ha puesto de manifiesto su relación con la conciencia emocional y la inadaptación. El estudio tuvo 3 objetivos: 1) analizar la prevalencia de las quejas somáticas; 2) explorar las relaciones entre las variables evaluadas: quejas somáticas, diferenciar emociones, comunicar verbalmente emociones, no esconder emociones, conciencia corporal, atender emociones de otros, análisis de las propias emociones, inadaptación personal, inadaptación social, inadaptación familiar e inadaptación escolar, y 3) identificar variables predictoras de las quejas somáticas.
Pacientes y métodosLos participantes, seleccionados aleatoriamente, fueron 1.134 escolares de 10–12 años (media±desviación típica=10,99±0,88), de ambos sexos. Se aplicaron el Listado de quejas somáticas, cuestionario de conciencia emocional y el Test autoevaluativo multifactorial de adaptación infantil.
ResultadosLos resultados indicaron que la prevalencia de quejas somáticas es del 90,2%, siendo el cansancio, el dolor de cabeza y el dolor de estómago los más frecuentes. Los mareos y el dolor de cabeza son superiores en niñas y las quejas disminuyen con la edad. Las quejas somáticas se relacionan negativamente con la conciencia emocional y positivamente con la inadaptación. Las variables que más contribuyen en la predicción de las quejas somáticas son la inadaptación personal (25.1%) y diferenciar emociones (2.5%).
ConclusionesEl trabajo permite concluir que la inadaptación personal es la mejor predictora de las quejas somáticas, así a mayor conciencia emocional y mejor adaptación, menor es el número de quejas somáticas presentadas, siendo la infancia una etapa evolutiva con importante malestar físico.
Somatic complaints (SCs) are body-related perceptions with subjectively experienced unpleasant qualities.1,2 Twenty-five percent of children seen at the paediatrician's office have physical symptoms that are better explained as psychosomatic manifestations rather than medical conditions.3 Epidemiology studies show an increase in the prevalence of SCs, with 5–30% of children 8–16 years of age affected by them.3,6,7 Some studies identify stomachache as the most common SC, with a prevalence that ranges between 8% and 25% of schoolchildren,8 while others reported fatigue (12.1%)1 or headache (58.5%) as the most prevalent.9,10 When we consider sex and age, the prevalence of SCs is higher in girls than in boys,1,8,10,11 and in early childhood and early adolescence.12
In the absence of identifiable organic causes, there is growing interest in the processes at play in psychosocial factors.2,5,10–14 This study analysed two possible factors: emotional functioning as manifested by emotion awareness, and the maladjustment of the child in various settings.
The association between emotional functioning and SCs2,15,16 suggests that alexithymia, a limited ability to identify and express emotions, is the main characteristic of individuals with SCs.17,18 There is evidence of this association in the paediatric population,13,19 as it has been observed that an inability to differentiate emotions and a strong bodily awareness in the course of experiencing emotion are predictors for SCs.13,20 Van der Veek et al2 noted that children with poor emotional awareness have difficulty recognising the emotions they experience and coping effectively with them. The use of maladaptive coping strategies leads to an increase in somatisation in response to the unresolved emotional conflict.21
Recurrent SCs can lead to psychosocial impairment and have a negative impact on the child's family life, ability to concentrate, cognitive development and academic achievement.4,9,16,21,22 Furthermore, children with SCs have poorer school attendance, participate less in extracurricular activities, and have poorer interpersonal relationships.4,5,9,10,22 Vila et al22 observed that 47% of children with SCs had difficulty concentrating, 30% missed school, and 24% spent time with friends less frequently. The presence of SCs as a result of personal maladjustment and social problems has also been studied. In this regard, conflict with peers or in the family environment leads to negative moods that in turn increase the likelihood of SCs.6,15,23,24
In conclusion, SCs are common in childhood, yet there is little research on the subject.25 There is evidence that the aetiology of SCs involves psychosocial factors in addition to medical factors. This underscores the importance of knowing the variables that may influence SCs in order to develop effective interventions.
In this context, we established three objectives: (1) to analyse the prevalence of SCs; (2) to explore the relationship between the variables under study; and (3) to identify predictor for SCs. Based on the findings of previous studies, we formulated the following hypotheses: (1) the prevalence of SCs is between 5% and 30%, and the most prevalent complaints are headache and stomachache; (2) SCs correlates negatively to emotional awareness variables and positively to maladjustment variables; and (3) the variables that can predict SCs are differentiating emotions, verbal sharing of emotions, bodily awareness and social maladjustment.
Patients and methodsParticipantsThe participants were 1134 children between 10 and 12 years of age (mean±SD=10.99±0.80), with a homogeneous sex and age distribution (53.4% female; 46.6% male; 371 age 10 years; 401 age 11 years; 362 age 12 years), enrolled in 12 public and charter schools in the autonomous community of Valencia (Spain). We used cluster sampling, taking into account the cities and their number of inhabitants, the type of institution (public or charter school), the number of students in each school, and the age groups.
Measurement instrumentsWe evaluated SCs by means of the Somatic Complaint List (SCL).26 This instrument assesses how frequently the individual has experienced pain in the preceding 4 weeks. It consists of 11 items with three answer choices (1=never; 2=sometimes; 3=often) that add to an overall score. Of these items in the scale, one refers to overall pain and eight to specific SCs: tiredness, stomachache, weakness, dizziness, headache, nausea, feeling faint, and chest pain. Two are contrasting items and refer to wellness: “I feel healthy” and “I feel well”. This questionnaire has shown good reliability (α=.81) and good psychometric properties (NFI=.95; CFI=.94; IFI=.94; RMSEA=.07) (P<.001) in previous studies.27
Emotional awareness was measured by means of the Emotion Awareness Questionnaire (EAQ),13 which has 30 items with 3 answer choices (1=not true; 2=sometimes true; 3=true). It assesses 6 dimensions: differentiating emotions (ability to identify, differentiate and understand the cause of emotions, 7 items); verbal sharing of emotions (sharing own feelings with others, 3 items); not hiding emotions (open and appropriate expression of emotions, 5 items); bodily awareness (ability to make the connection between physical sensations and emotions, 5 items); attending to others’ emotions (an interest in listening to and/or perceiving others’ emotions, 5 items); and analysing emotions (an interest in perceiving and understanding own emotions, 5 items). The higher the score in a given dimension, the higher the ability is supposed to be in that area. The factors have shown acceptable reliability (between α=0.63 and α=0.68) and the factor structure has been confirmed for the Spanish version (maximum likelihood method): NFI=0.92; CFI=0.91; IFI=0.91; RMSEA=0.03 (P<.001)27.
Maladjustment was assessed by means of the Test autoevaluativo multifactorial de adaptación infantil (Multifactor Self-Assessment Test of Child Adjustment [TAMAI]).28 It evaluates maladjustment and consists of 172 dichotomous items (0=no, 1=yes). In every dimension, higher scores correspond to higher levels of maladjustment. We used four of its scales: personal (distorted view of oneself and difficulty facing reality, range 0–35), social (lack of control, respect and consideration towards others, reduced social interaction and mistrust, range 0–35), family (dissatisfaction with the family environment and the relationship with parents, range 0–5) and school (low achievement, disruptive behaviours and negative attitude, range 0–30). The reliability of the used scales was adequate (α=0.82, α=0.78, α=0.69 and α=0.88, respectively), reaching a reliability of α=0.89 in the sample of the authors.28
These self-assessment tools were designed to be used from 8 years of age, once the child is capable of reporting his or her feelings and experiences.29
Study design and protocolThe study had a descriptive cross-sectional design. We contacted the schools to explain the objectives of the study, seek their collaboration, and request their consent. We sent a letter to parents explaining the study and requesting their consent for participation.
We performed the statistical analysis of the data with the SPSS software (version 21). We calculated descriptive statistics for the variables under study and Pearson's bivariate correlations to study the association between the variables, performed Student's t tests and multivariate analyses of variance to study the differences between groups, and finally did stepwise hierarchical regression analyses, testing the necessary assumptions.30
Ethical considerationsThis study was approved by the ethics committee of the Conselleria d’Educació de la Comunitat Valenciana (Education Department of the Autonomous Community of Valencia), adhering to the principles of the Declaration of Helsinki and the current law. Self-administered questionnaires were given out by teachers to entire classes of students during school hours in two sessions of 45min each.
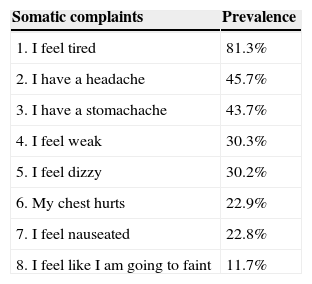
ResultsPrevalenceThe most prevalent complaint was tiredness, reported by 81.3% of the assessed children; followed by headache (45.7%) and stomach ache (43.7%), while feeling faint was the least prevalent complaint (11.7%) (Table 1).
Prevalence of somatic complaints (from highest to lowest).
| Somatic complaints | Prevalence |
|---|---|
| 1. I feel tired | 81.3% |
| 2. I have a headache | 45.7% |
| 3. I have a stomachache | 43.7% |
| 4. I feel weak | 30.3% |
| 5. I feel dizzy | 30.2% |
| 6. My chest hurts | 22.9% |
| 7. I feel nauseated | 22.8% |
| 8. I feel like I am going to faint | 11.7% |
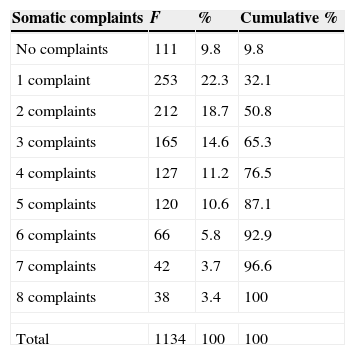
When we considered the number of reported SCs, we found that only 9.8% of the assessed children reported none; 40% of children reported one or two; and 12.9% six or more complaints (Table 2). For the purpose of this analysis, a complaint existed if the participant answered “sometimes” or “often” for it.
Frequency of somatic complaints.
| Somatic complaints | F | % | Cumulative % |
|---|---|---|---|
| No complaints | 111 | 9.8 | 9.8 |
| 1 complaint | 253 | 22.3 | 32.1 |
| 2 complaints | 212 | 18.7 | 50.8 |
| 3 complaints | 165 | 14.6 | 65.3 |
| 4 complaints | 127 | 11.2 | 76.5 |
| 5 complaints | 120 | 10.6 | 87.1 |
| 6 complaints | 66 | 5.8 | 92.9 |
| 7 complaints | 42 | 3.7 | 96.6 |
| 8 complaints | 38 | 3.4 | 100 |
| Total | 1134 | 100 | 100 |
Our results showed statistically significant differences between the sexes, with girls reporting a higher prevalence of SCs such as “I feel weak” (P≤.004) and “I have a headache” (P≤.006). They also scored higher in EAQ subscales like bodily awareness (P≤.001), attending to others’ emotions (P≤.001) and analyses of emotions (P≤.001). Boys scored higher in the TAMAI scale for social maladjustment (P≤.001) and school maladjustment (P≤.001).
We also found statistically significant differences by age in some SCs: “I feel weak” (P≤.003), “I feel dizzy” (P≤.008) and “I feel nauseated” (P≤.032). There were also differences in the differentiating emotions (P≤.001) and bodily awareness (P≤.009) variables of the EAQ, and in the personal maladjustment (P≤.001) and family maladjustment (P≤.001) of the TAMAI, suggesting that the older the child, the lower the level of SCs correlated to every variable, except for differentiating emotions. The effect size was small in all instances.
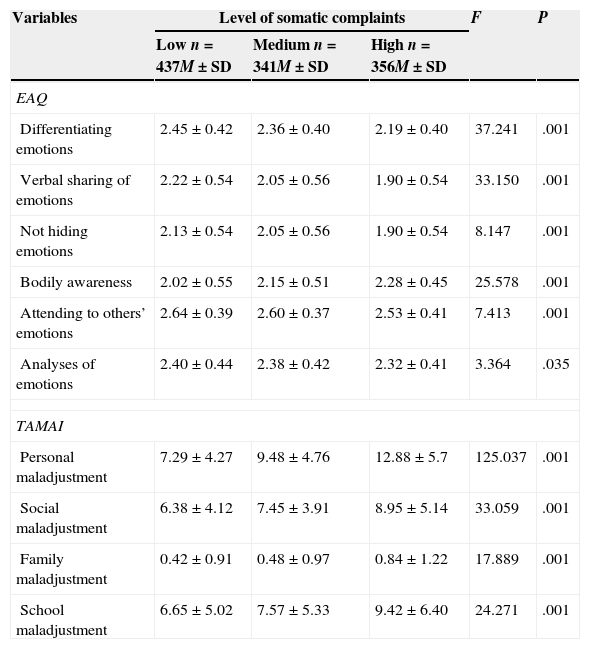
Emotional awareness and maladjustment: differences by somatic complaintTo analyse the differences in emotional awareness and maladjustment in relation to somatic complaints, we divided the participants into groups by the score obtained in the SCL, stratified by tertiles. The results of the analysis showed statistically significant differences in every analysed variable except for analyses of emotions (Table 3), as children with low levels of SCs had higher scores in differentiating emotions (P≤.001), verbal sharing of emotions (P≤.001), not hiding emotions (P≤.001), attending to others’ emotions (P≤.001) and analyses of own emotions (P≤.035). Meanwhile, they scored lower in bodily awareness (P≤.001) and in personal (P≤.001), social (P≤.001), family (P≤.001) and school maladjustment (P≤.001). Although post hoc Tukey's tests confirmed the differences between the three groups, the effect size was low.
Differences in means in the analysed variables by level of somatic complaints (ANOVA).
| Variables | Level of somatic complaints | F | P | ||
|---|---|---|---|---|---|
| Low n=437M±SD | Medium n=341M±SD | High n=356M±SD | |||
| EAQ | |||||
| Differentiating emotions | 2.45±0.42 | 2.36±0.40 | 2.19±0.40 | 37.241 | .001 |
| Verbal sharing of emotions | 2.22±0.54 | 2.05±0.56 | 1.90±0.54 | 33.150 | .001 |
| Not hiding emotions | 2.13±0.54 | 2.05±0.56 | 1.90±0.54 | 8.147 | .001 |
| Bodily awareness | 2.02±0.55 | 2.15±0.51 | 2.28±0.45 | 25.578 | .001 |
| Attending to others’ emotions | 2.64±0.39 | 2.60±0.37 | 2.53±0.41 | 7.413 | .001 |
| Analyses of emotions | 2.40±0.44 | 2.38±0.42 | 2.32±0.41 | 3.364 | .035 |
| TAMAI | |||||
| Personal maladjustment | 7.29±4.27 | 9.48±4.76 | 12.88±5.7 | 125.037 | .001 |
| Social maladjustment | 6.38±4.12 | 7.45±3.91 | 8.95±5.14 | 33.059 | .001 |
| Family maladjustment | 0.42±0.91 | 0.48±0.97 | 0.84±1.22 | 17.889 | .001 |
| School maladjustment | 6.65±5.02 | 7.57±5.33 | 9.42±6.40 | 24.271 | .001 |
M: mean; SD: standard deviation.
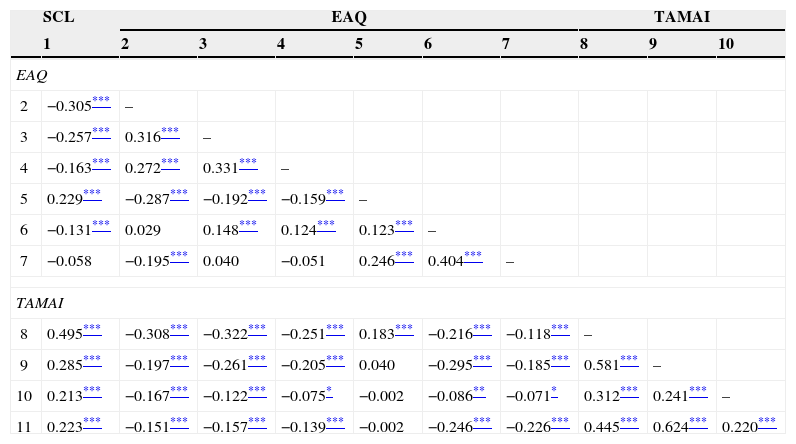
The correlation analyses (Table 4) showed inverse correlations between SCs and the variables differentiating emotions (r=−0.305; P≤.001), verbal sharing of emotions (r=−0.257; P≤.001) and attending to others’ emotions (r=−0.131; P≤.001), and positive correlations between SCs and bodily awareness (r=0.229; P≤.001), personal (r=0.495; P≤.001), social (r=0.285; P≤.001), family (r=0.213; P≤.001) and school maladjustment (r=0.223; P≤.001).
Pearson's correlation between the different analysed variables (n=1134).
| SCL | EAQ | TAMAI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
| EAQ | ||||||||||
| 2 | −0.305*** | – | ||||||||
| 3 | −0.257*** | 0.316*** | – | |||||||
| 4 | −0.163*** | 0.272*** | 0.331*** | – | ||||||
| 5 | 0.229*** | −0.287*** | −0.192*** | −0.159*** | – | |||||
| 6 | −0.131*** | 0.029 | 0.148*** | 0.124*** | 0.123*** | – | ||||
| 7 | −0.058 | −0.195*** | 0.040 | −0.051 | 0.246*** | 0.404*** | – | |||
| TAMAI | ||||||||||
| 8 | 0.495*** | −0.308*** | −0.322*** | −0.251*** | 0.183*** | −0.216*** | −0.118*** | – | ||
| 9 | 0.285*** | −0.197*** | −0.261*** | −0.205*** | 0.040 | −0.295*** | −0.185*** | 0.581*** | – | |
| 10 | 0.213*** | −0.167*** | −0.122*** | −0.075* | −0.002 | −0.086** | −0.071* | 0.312*** | 0.241*** | – |
| 11 | 0.223*** | −0.151*** | −0.157*** | −0.139*** | −0.002 | −0.246*** | −0.226*** | 0.445*** | 0.624*** | 0.220*** |
1: somatic complaints; 2: differentiating emotions; 3: verbal sharing of emotions; 4: not hiding emotions; 5: bodily awareness; 6: attending to others’ emotions; 7: analyses of emotions; 8: personal maladjustment; 9: social maladjustment; 10: family maladjustment; 11: school maladjustment.
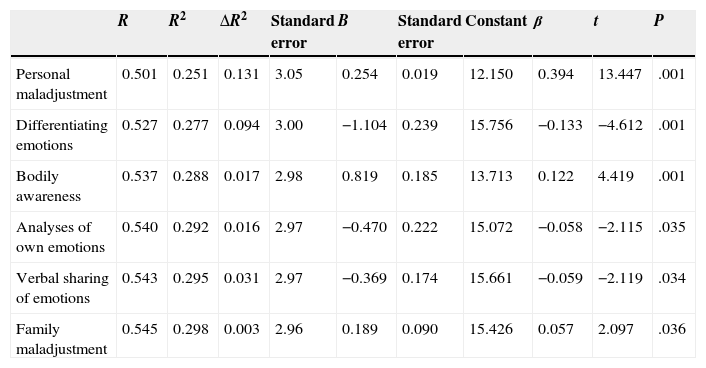
The linear regression analysis with SCs as the criterion variable and emotional awareness and maladjustment as predictors (Table 5) showed that six of the predictor variables were statistically significant: personal maladjustment (β=0.394; ΔR2=0.251), differentiating emotions (β=−0.133; ΔR2=0.026), bodily awareness (β=0.122; ΔR2=0.011), analyses of own emotions (β=−0.058; ΔR2=0.004), verbal sharing of emotions (β=−0.059; ΔR2=0.003) and family maladjustment (β=0.057; ΔR2=0.003). The beta standardised regression coefficients suggest that the influence of these variables on SCs in small, except for personal maladjustment. This group of variables explains 29.4% of the SC variance.
Regression analysis of the variables evaluated concerning somatic complaints.
| R | R2 | ΔR2 | Standard error | B | Standard error | Constant | β | t | P | |
|---|---|---|---|---|---|---|---|---|---|---|
| Personal maladjustment | 0.501 | 0.251 | 0.131 | 3.05 | 0.254 | 0.019 | 12.150 | 0.394 | 13.447 | .001 |
| Differentiating emotions | 0.527 | 0.277 | 0.094 | 3.00 | −1.104 | 0.239 | 15.756 | −0.133 | −4.612 | .001 |
| Bodily awareness | 0.537 | 0.288 | 0.017 | 2.98 | 0.819 | 0.185 | 13.713 | 0.122 | 4.419 | .001 |
| Analyses of own emotions | 0.540 | 0.292 | 0.016 | 2.97 | −0.470 | 0.222 | 15.072 | −0.058 | −2.115 | .035 |
| Verbal sharing of emotions | 0.543 | 0.295 | 0.031 | 2.97 | −0.369 | 0.174 | 15.661 | −0.059 | −2.119 | .034 |
| Family maladjustment | 0.545 | 0.298 | 0.003 | 2.96 | 0.189 | 0.090 | 15.426 | 0.057 | 2.097 | .036 |
Our objectives were to analyse the prevalence of SCs, explore their relationship with emotional awareness and maladjustment, and identify predictor variables. The results showed differences between sexes and age groups, but these variables were not included in subsequent analyses due to their small effect size. The results we obtained were not consistent with the existing literature,9,10 as girls only scored higher than boys in having a headache and feeling nauseated. When it came to age, we observed an inverse correlation with SCs, rather than the increase in frequency described in the previous literature,1,9,12 and we also did not find a greater prevalence of headache in older children.
Based on our initial hypotheses, we expected the prevalence of SCs to be between 5% and 30%.3,6 Only 9.8% of participants reported being free from SCs, which means that 90.2% had experienced some type of pain in the past few weeks. And while 22.3% of participants reported a single SC, this was not the usual pattern, as 67.9% of participants reported having two or more. In this sense, our results showed a greater prevalence of SCs in childhood,4,5 and were alarming due to the high rates reported and the sample not being a clinical but a community sample. The data showed similar prevalences of headache and stomachache (45.7% and 43.7%, respectively), which were the most prevalent SCs in the literature we reviewed.8,9 However, the most prevalent SC was tiredness (81.3%), similar to the fatigue reported by Barkmann et al.1 When we consider the pace of life in current society, it makes sense for children to feel tired, as it is difficult to balance work and family life. The daily routine includes the school day and coordinating the parents’ work schedules with homework and extracurricular activities (foreign language study, music, sports). This situation results in longer days, delayed bedtimes, and a reduction in the hours of sleep. The high prevalence we observed may also be due to characteristics of our sample or to the self-reporting nature of the instruments used in our assessment. However, the fact that these self-reporting tools have been used in the past and that the observed results are consistent with the literature supports this hypothesis.
Our second hypothesis stated that SCs would be negatively correlated with emotional awareness variables and positively correlated to maladjustment variables. On this point, as expected, SCs were negatively correlated to the differentiating emotions, verbal sharing of emotions, not hiding emotions, and attending to others’ emotional variables.2,15,21 We would like to underscore the positive correlation between SCs and bodily awareness. Similar to previous studies that used the EAQ2,21 and with the purpose of making a homogeneous interpretation of the analyses of every aspect of emotional awareness, we computed the score of the bodily awareness subscale without reversing the items. The results seem confusing, as being aware of the physical sensations that accompany emotions should be a good thing, but it is associated to SCs. However, they are similar to results obtained in previous studies,13,14 in which children that were more aware of the relationship between bodily sensations and emotions reported more somatic symptoms. One possible explanation is that these children are very aware of their sensations and are therefore more nervous, manifesting anxiety through SCs. On the other hand, the correlation between SCs and personal, social, family and school maladjustment was positive.4–6,9,10,16,21 We ought to note that the positive correlation between SCs and personal maladjustment was the highest we found in our results. This is relevant given how little evidence is available on the association of these variables, although there are studies that analyse the association of SCs with maladjustment and social, school, and family problems.4,6,9,16,23,24 Previous studies may have underestimated the importance of intrapersonal variables in favour of interpersonal variables due to the difficulties inherent in evaluating the former.
Our third hypothesis stated that aspects of emotion awareness associated with alexithymia would contribute most to explaining SCs 2,13 along with social maladjustment.4,16,23 Yet, the variable that explained the greatest amount of variance was personal maladjustment; while the other variables contributed less to it. As we noted above, few studies have analysed the association between SCs and personal maladjustment, although SCs have been associated with variables like self-esteem, quality of life, wellbeing, mood, and adjustment.2,4–6,9,15 The personal maladjustment scale of the TAMAI refers to the adjustment and balance of the individual with him or herself; it is a complex construct, but it can be used to observe the relevance of the child's inner life in his or her physical wellbeing. Considering our results, the study of personal aspects is important to understand what is happening to the child, how it is affecting him or her, and the ensuing consequences. From an early age, children have personal feelings and thoughts about what is happening in their environment, and it is important that we understand how they function at a personal level and how they face everyday conflicts. Thus, the more effective their coping mechanisms, the better their adjustment is, and the lesser their health and social problems.
One of the main limitations of our study is the exclusive use of self-reporting tools, although from 8 years of age children start having direct knowledge of their thoughts and feelings, and their answers can be reliable.29 It is also worth noting that the effect size was small in every case; however, we did observe significant differences, so we must consider what these results are pointing at, and explore it more thoroughly in future research. Lastly, it would be interesting to include different informants, like parents, paediatricians and teachers, to gain a broader understanding of the issue and its scope.
To conclude, the prevalence of SCs in children 10–12 years of age (community sample) was high, as 90.2% of participants reported having at least one SC. Furthermore, emotional awareness was important in explaining SCs, although the variable that contributed most to the presence of SCs was personal maladjustment. Thus, focusing exclusively on the association between emotional awareness and SCs is an oversimplified approach to the issue, as SCs are not only the result of poor emotional regulation through the day, but a physical response of the body to personal problems and conflicts.
Our study is relevant in that it contributes a new perspective to the understanding of SCs. Childhood is a developmental stage in which there is considerable physical pain requiring more attention.10,27 Collective interventions implemented in schools27 for the development of emotional skills and coping strategies may contribute to wellbeing, reducing the prevalence of SCs, the use of primary care healthcare services, and parental absences from work.
FundingThis study has been funded by:
- –
The Ministerio de Ciencia e Innovación (Ministry of Science and Innovation, project PSI2010-18742).
- –
The Consellería d’Educació de la Generalitat Valenciana (Department of Education of the Autonomous Community of Valencia, PROMETEO/2011/009).
- –
The Universitat de València (Atracció de Talent fellowship for predoctoral researchers).
- –
Departamento de Educación, Política Lingüística y Cultura (Department of Education, Political Linguistics and Culture) of the Autonomous Community of the Basque Country (IT638-13).
- –
The Unidad de Formación e Investigación (Department of Training and Investigation) of the Universidad del País Vasco (UFIPSIXXI-11/04).
The authors have no conflicts of interest to declare.
Please cite this article as: Ordóñez A, Maganto C, González R. Quejas somáticas, conciencia emocional e inadaptación en población escolar. An Pediatr (Barc). 2015;82:308–315.