An increase in the number of internationally adopted children has been observed in the last few years. The country of origin that has experienced a greater increase is Ethiopia. The health of internationally adopted children from Ethiopia has not been extensively assessed to date.
The main objective of the study is to determine the prevalence of infectious diseases in children adopted from Ethiopia, and to assess their nutritional status.
MethodA prospective, observational cohort study was conducted using the medical records of 251 children adopted from Ethiopia to Spain in the period from January 1, 2006 to December 31, 2010.
ResultsThe mean age of the children was 7 months (range 1–120). Abnormalities were detected on physical examination in 56.6%. In 90% of cases the child was less than 5 years old. Half of the sample had a weight below the third percentile, with some degree of malnutrition in 65% of the children. HIV exposure was not uncommon (4.8%).
ConclusionsLow weight and acute gastroenteritis were the main findings in this cohort. Infectious diseases should be systematically assessed.
La adopción internacional (AI) en nuestro país es un fenómeno reciente, siendo Etiopía uno de los países de origen más frecuentes.
El objetivo principal del estudio es determinar la prevalencia de enfermedades infecciosas en los niños adoptados procedentes de Etiopía y valorar su estado nutricional.
MétodoEstudio de cohortes prospectivo, observacional. Se evalúa una cohorte de 251 niños adoptados en España procedentes de Etiopía (período del 1 de enero del 2006 y al 31 de diciembre del 2010).
ResultadosLa edad media fue de 7 meses (90% de ellos menores de 5 años). Se detectó alguna anomalía en la exploración física en el 56.6%. La mitad de la muestra presentó un peso por debajo del tercer percentil, encontrándose algún grado de malnutrición en el 65% de los niños.
Desde el punto de vista infeccioso, el hallazgo más frecuente fue la afectación cutánea. El 15.1% de los pacientes presentaba diarrea en el momento de la exploración.
En las pruebas analíticas destacan: leucocitosis > 15.000/μL en el 8.8% e hipertransaminasemia en el 29% de los pacientes. La serología de VIH fue positiva en el 4.8% de los casos, mientras que la PCR-VIH fue positiva en el 0.8%.
ConclusionesPredomina la adopción en los 5 primeros años de la vida. El bajo peso fue el hallazgo más frecuente en esta muestra. Las enfermedades infecciosas deberían ser sistemáticamente descartadas, incluso con la utilización de PCR-VIH dado que la exposición al virus no es infrecuente.
In recent years, international adoption (IA) has increased in Spain, although the number of adoptions has decreased gradually after peaking in 2004. International adoption is a recent phenomenon in our country, and Ethiopia is one of the most frequent countries of origin. According to data from the Spanish Ministry of Health, the number of internationally adopted children has decreased in recent years between 2008 (3156 adoptions) and 2012 (1669 adoptions). Adoptions from Ethiopia have ranked third in Spain (following Russia and China), although at the international level Ethiopia ranked second as the country of origin of adopted children in 2008.1 Children from IAs require specialised medical attention upon arriving to Spain, as their actual health and nutritional status are unknown (many of them have spent long periods in orphanages, where malnutrition is common). All children from IAs have been exposed to potential health risk factors, so most problems affecting their physical health, neurodevelopment and social adjustment at the time of arrival (or emerging at a later point) may result from a combination of these factors.2
Ethiopia is one of the three poorest countries in the world. Its per capita income is $100, the life expectancy is 40.5 and the child mortality rate is 124.6 per 1000. There are serious deficiencies in health care, and endemic droughts occur in many regions leading to cyclical famines.
It is a misconception that these children have undergone full medical evaluations and are thus free from health problems. At any rate, there are few data on the health status of internationally adopted children in Spain.
MethodsWe conducted an observational cohort study by reviewing the medical records of 251 children adopted from Ethiopia in Spain between January 1, 2006 and December 31, 2010. The children had been evaluated in Ethiopia during the preadoption stage.
The children and their corresponding reports were analysed independently by two doctors experienced in IA. The analysed variables were: age (official), weight, height, weight-for-height, weight-for-age, height-for-age, and head circumference-for-age. The basic laboratory tests used included: complete blood count, and liver (transaminases and bilirubin) and kidney (creatinine) function tests. The microbiology tests performed included: serology for hepatitis B and C; HIV, confirmed by 2 PCR assays in seroreactive patients (one at the country of origin and one on samples submitted for confirmation to Spain); and syphilis. All patients were evaluated at an adoption clinic in Addis Ababa.
All children underwent a full physical exploration, which included taking anthropometric measurements and finding their corresponding percentiles in the WHO growth charts. Based on this physical examination, additional evaluations were performed, such as a vision screening, cardiovascular assessment (with echocardiography if needed due to the presence of a pathological murmur) or neurological assessment (including a computed tomography of the brain when needed). All children were evaluated, irrespective of the presence or absence of disabilities.
Applying the WHO criteria, anaemia was defined as a haemoglobin level below 11mg/dL in children younger than 5 years, below 11.5g/L from 5 to 12 years of age, and below 12mg/dL in older individuals.3
We used a conventional statistical package (SPSS v17) to do the statistical analysis. We used Student's t for hypothesis tests involving continuous or continuous and categorical variables, and the chi squared to compare qualitative variables. We calculated z-scores for nutritional indices (weight-for-age, height-for-age, weight-for-height and head circumference-for-age) by means of macros designed for the statistics software provided by the WHO (http://www.who.int/childgrowth/software/en/).
ResultsThe mean age was 7 months (range 1–120 months). There were no significant differences between sexes in our cohort (P>.05).
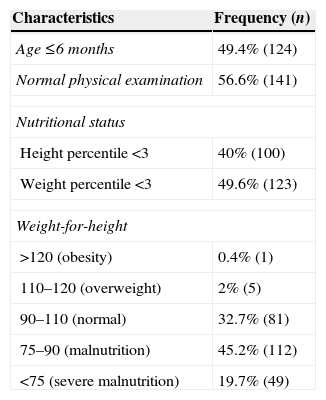
Abnormalities were detected during the physical examination of 141 children (56.6%). Sixty percent of the sample were 6 months of age or younger, and ninety percent were younger than 5 years (Table 1).
Sample characteristics and assessment of nutritional status.
| Characteristics | Frequency (n) |
|---|---|
| Age ≤6 months | 49.4% (124) |
| Normal physical examination | 56.6% (141) |
| Nutritional status | |
| Height percentile <3 | 40% (100) |
| Weight percentile <3 | 49.6% (123) |
| Weight-for-height | |
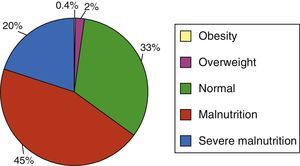
| >120 (obesity) | 0.4% (1) |
| 110–120 (overweight) | 2% (5) |
| 90–110 (normal) | 32.7% (81) |
| 75–90 (malnutrition) | 45.2% (112) |
| <75 (severe malnutrition) | 19.7% (49) |
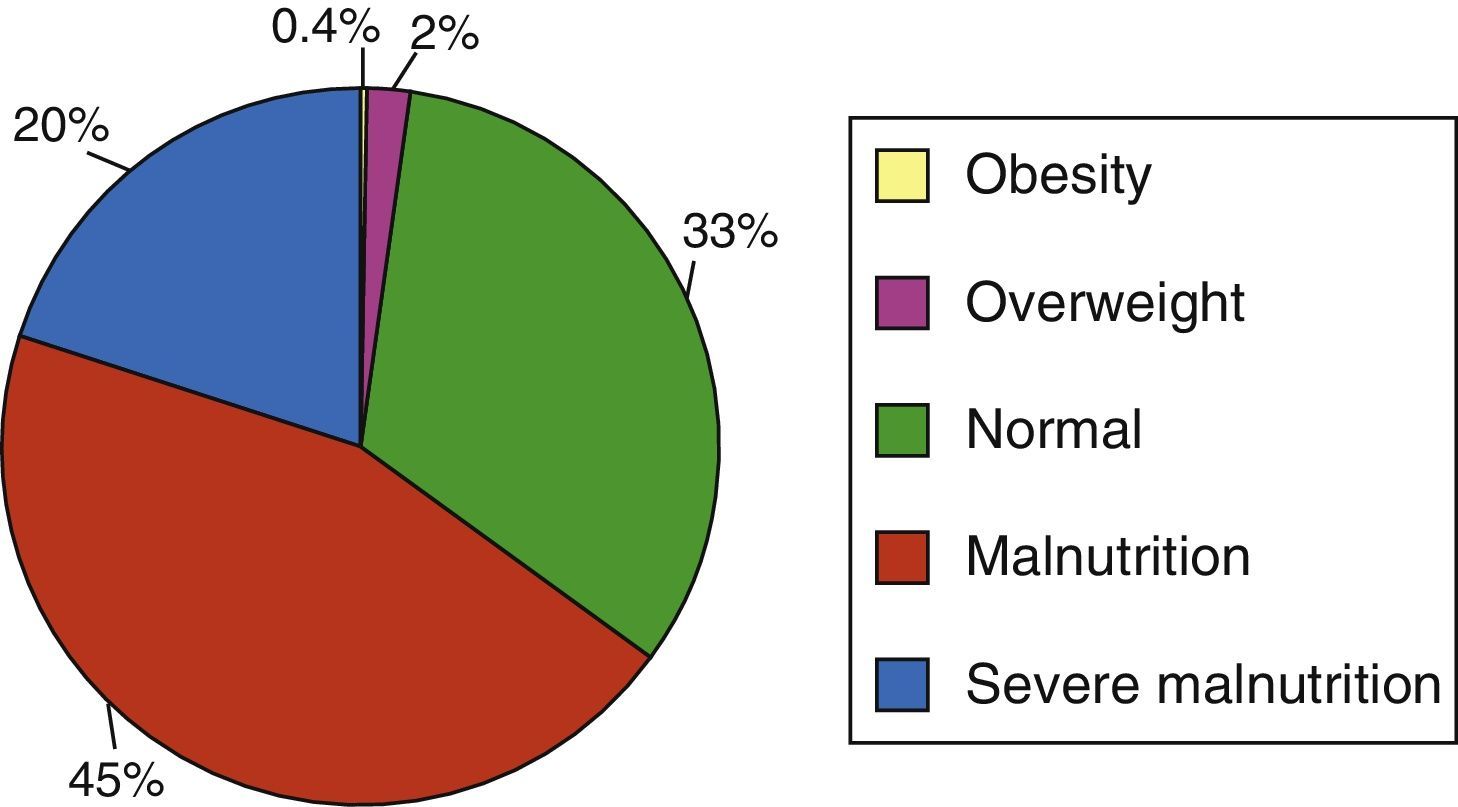
From a nutritional standpoint, 123 children (49%) had a weight below the 3rd percentile, and 40% were below the 3rd percentile for height. The assessment of malnutrition found some degree of it in 65% of the sample (Fig. 1).
We proceed to summarise our results regarding the presence of common diseases.
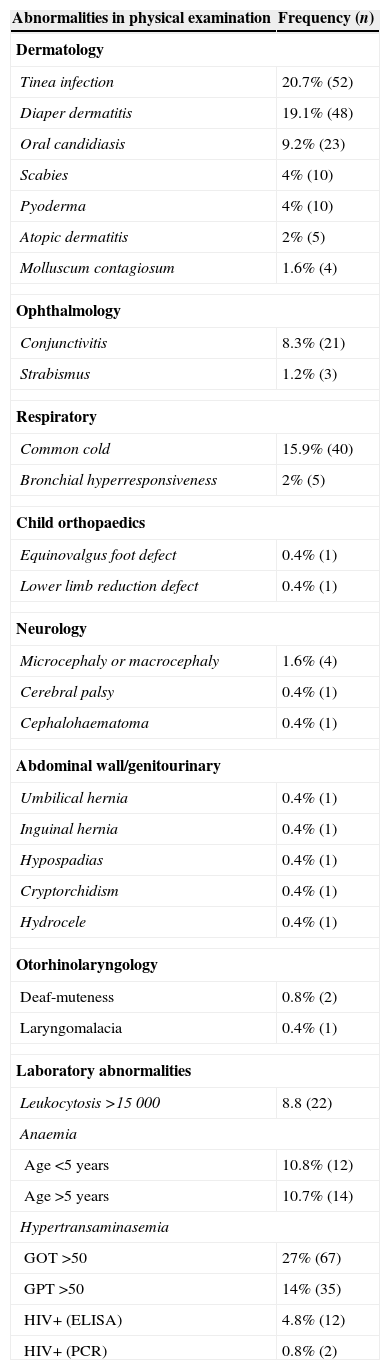
Skin lesions were found in 129 patients, which amounts to more than half of the sample, (51.4%), and the most common skin conditions were tinea infections (20.7%) and diaper dermatitis (19.1%). The least frequent diseases (<5%) were heart anomalies, cavities, deaf-muteness and hepatosplenomegaly (Table 2).
Findings of the physical examination and laboratory tests.
| Abnormalities in physical examination | Frequency (n) |
|---|---|
| Dermatology | |
| Tinea infection | 20.7% (52) |
| Diaper dermatitis | 19.1% (48) |
| Oral candidiasis | 9.2% (23) |
| Scabies | 4% (10) |
| Pyoderma | 4% (10) |
| Atopic dermatitis | 2% (5) |
| Molluscum contagiosum | 1.6% (4) |
| Ophthalmology | |
| Conjunctivitis | 8.3% (21) |
| Strabismus | 1.2% (3) |
| Respiratory | |
| Common cold | 15.9% (40) |
| Bronchial hyperresponsiveness | 2% (5) |
| Child orthopaedics | |
| Equinovalgus foot defect | 0.4% (1) |
| Lower limb reduction defect | 0.4% (1) |
| Neurology | |
| Microcephaly or macrocephaly | 1.6% (4) |
| Cerebral palsy | 0.4% (1) |
| Cephalohaematoma | 0.4% (1) |
| Abdominal wall/genitourinary | |
| Umbilical hernia | 0.4% (1) |
| Inguinal hernia | 0.4% (1) |
| Hypospadias | 0.4% (1) |
| Cryptorchidism | 0.4% (1) |
| Hydrocele | 0.4% (1) |
| Otorhinolaryngology | |
| Deaf-muteness | 0.8% (2) |
| Laryngomalacia | 0.4% (1) |
| Laboratory abnormalities | |
| Leukocytosis >15000 | 8.8 (22) |
| Anaemia | |
| Age <5 years | 10.8% (12) |
| Age >5 years | 10.7% (14) |
| Hypertransaminasemia | |
| GOT >50 | 27% (67) |
| GPT >50 | 14% (35) |
| HIV+ (ELISA) | 4.8% (12) |
| HIV+ (PCR) | 0.8% (2) |
The most frequently found infections were skin infections, which affected 50 patients (20%). Besides tinea infections, scabies and pyoderma affected 10 children. Oral candidiasis was found in 9.1%. Seventeen percent of patients had acute gastroenteritis at the time of the physical examination. Cysts caused by Giardia lamblia were found in 1.4%.
The vision screening was abnormal in 2% (3 cases of strabismus). Other minor abnormalities were found, such as conjunctivitis (21 children; 8.3%). Also, Lisch nodules were found in one child (suspected neurofibromatosis type 1).
Hearing problems were detected in 0.9% of children.
Of all children, 6.4% had been circumcised.
Respiratory conditions included the presence of common colds in 15.9% of the children and bronchial hyperresponsiveness in 2%.
The orthopaedic assessment found an equinovalgus foot deformity in one child and a lower limb reduction defect in another.
We found 2 cases of microcephaly and 2 of macrocephaly. One patient had cerebral palsy and another had a cephalohaematoma.
The ear, nose and throat assessment identified two deaf-mute children and one with laryngomalacia.
There were isolated instances of conditions such as umbilical and inguinal hernia and other genitourinary abnormalities, such as hypospadias, cryptorchidism or hydrocele.
There were 3 cases of systolic murmur (echocardiography was available for two of these children, revealing a ventricular septal defect in one, and a patent foramen ovale in the other).
The most relevant findings of laboratory tests included a white blood cell count above 15000/μL in 8.8% (22 children), which was usually associated to upper respiratory tract infections, and hypertransaminasemia in 29% of the patients. Twenty-seven percent had GOT levels above 50U/L and fourteen percent had GPT levels 50U/L. The elevation of GPT or GOT never exceeded 10 times the upper bound of the normal range.
Anaemia was found in 10.8% of children younger than 5 years, and in 10.7% of older children (Table 2).
The HIV serology test was positive in 4.8% of the children, while the PCR assay for HIV was positive in 0.8%. Hepatitis B (HBsAg) and C (HCV IgG) were not detected in any children. One child was diagnosed with congenital syphilis (0.4%). The disease was identified in the patient at 15 days by a positive RPR result (1:8 titre) and a positive FTA-ABS result. The diagnosis was made without knowing the RPR/VDRL status of the mother at birth (which is extremely common in IA children from Ethiopia). We do not know whether the child received treatment at birth. Ethiopia adheres to international treatment guidelines, with symptomatic patients with unknown maternal status receiving treatment if syphilis is suspected: 50000units/kg of intramuscular benzylpenicillin every 12h for 7 days, then every 8h for another 3 days until the 10-day treatment course is completed.
DiscussionIn this study we evaluated the health status of 251 Ethiopian children adopted internationally.
The 7-month mean age reflects, on one hand, the need to find a responsible adult to care for the children that are up for adoption as soon as possible, and on the other hand the preferences of adopting families. In fact, most of these children (90%) are adopted before age 5 years. Compared to the mean age at adoption of children from other countries, these children are adopted considerably earlier, as opposed to children from countries like China, Guatemala o Russia, with mean ages at the time of adoption of 14, 16 and 26 months, respectively.4,5
Since the study had a criterion sample, its representativeness is limited. However, this study is relevant in that it involves the largest cohort of children from IA (for a single country of origin and overall) studied in Spain to date.
The preadoption physical examination found abnormalities in a high percentage of the sample (59.5%). Most of them were banal findings that posed no health risks to the children, such as skin fungal infections or upper respiratory tract infections.
Given its severity and contagiousness, it is important to make a working diagnosis of hepatitis or hypertransaminasemia as a first step to the definitive diagnosis. The prevalence of hypertransaminasemia (29%) in the sample was greater than the prevalence reported by the literature for Spain (6.7%).4 Ruling out this disease is important to prevent horizontal transmission to the adoptive parents of the infected child.6 Another potential cause of hypertransaminasemia is malnutrition.7
The prevalence of anaemia is much lower than the one reported in the longest cohort study published before8 (data for 50 children) and nationwide data for Spain (20%).
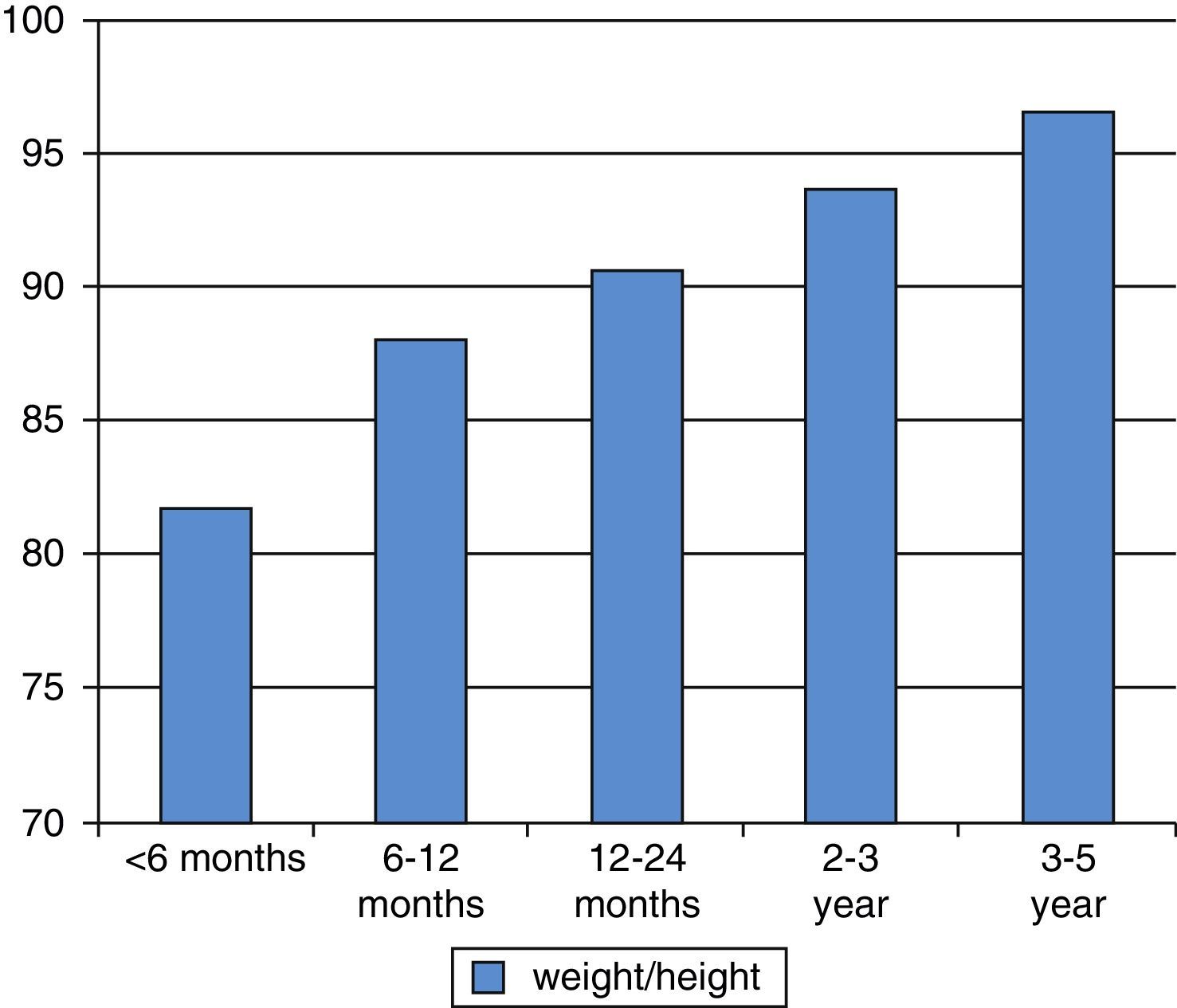
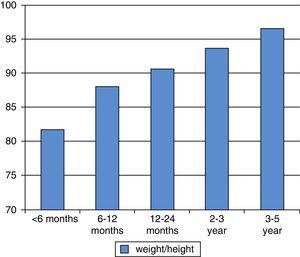
The most frequent finding related to nutritional status in our study was low weight, with the youngest children being most at risk for nutritional problems (Fig. 2).
Delayed growth and lower height are the most frequent findings reported in the IA literature. However, previous data show that compared to other countries like Russia,9 China10 or Guatemala,11 delays in the weight-for-age, height-for-age and head circumference-for-age indices were not as significant in children from Ethiopia.8 Meanwhile, the data found in this study are very different, as nearly 20% of the children younger than 5 years had a z-score for head circumference below −2 SD.
The weight, height and head circumference z-scores we found may have been due to institutionalisation. The length of time spent in an orphanage is proportional to the height and weight delays, and to impaired development.12 The ERA study described a linear correlation between the duration of institutionalisation and the prevalence of cognitive delay: 2.3%, 12.0% and 32.6% of children had cognitive delays at the time of evaluation after spending less than 6 months, 6–24 months, or 24–42 months institutionalised, respectively, prior to adoption.13
Nutritional problems may be caused by neglect, emotional deprivation or abandonment experienced before adoption. As happens with other groups of adopted children, there is evidence that cognitive delay in Ethiopian children is directly proportional to the age they arrive at the receiving country. Since many of them are adopted at an early age, the developmental and growth delays are mild when they arrive in Spain, so a full recovery can be expected.
The percentage of giardiasis cases stands in contrast to the high percentage found in a Spanish study on IA (with children mostly from China, Russia and Romania), although the presence of intestinal parasites was evaluated in all 127 children of that study.4 In our study, only symptomatic children were assessed for them, and we believe this is the reason for the lower prevalence.
We found no cases of hepatitis B infection, in contrast to the approximately 10% reported in France in a study of 60 children adopted from various countries.11,14 A study of 1282 internationally adopted children conducted in the United States between 1999 and 2006 to estimate the prevalence of infection by hepatitis B found a prevalence of 4%, consisting of 1.1% of chronic or acute infections and 2.9% of past infections.15 Overall, there is evidence of immunisation against hepatitis B virus in 64% of international adopted children, as they have antibodies for it.
Conversely, the prevalence of other infectious diseases was higher in our sample. We found 2 cases of HIV (0.8%). Infection by HIV is rare in children adopted in the United States (<1% has an HIV infection), and is most commonly acquired by perinatal transmission.16 Without prophylactic treatment, the risk of vertical transmission from an HIV-infected mother to the newborn is approximately 15%.17
We also found one case of congenital syphilis and one of hepatitis C (0.4%). Syphilis continues to be a rare infection in internationally adopted children, but it can cause severe complications if it goes untreated.
Infection by hepatitis C (HCV) is one of the main causes of liver disease worldwide. In our study, the only patient with HCV was not coinfected with HIV.
The most frequent laboratory finding was neutropaenia, found in 12.5% of the sample, which may reflect an ethnic trait rather than a medical issue.18
It is worth noting that we found no cases of foetal alcohol syndrome in this sample, as maternal alcohol intake is the most frequent cause of nonsyndromic intellectual disability, which has a high prevalence of approximately 23% in children adopted from Eastern Europe and Russia.19 We also found no cases of girls subjected to a clitoridectomy (a form of female genital mutilation that is still practised in some countries, including Ethiopia).
Results from the Mantoux test were not available in the preadoption evaluations of children from Ethiopia. We believe that once this simple test is introduced, we will be able to determine the prevalence of latent tuberculosis infections. A second PPD test should be done in these patients at least one month after arriving to the receiving country, as an approximate additional 20% of them get a positive result in this test following nutritional recovery.20 One of the limitations of our study is that no PPD tests were performed. Thus, we could not determine the rate of latent tuberculosis infection in our sample.
ConclusionsThe high prevalence of clinical and laboratory abnormalities shows that the health problems of internationally adopted children from Ethiopia are complex. Thus, these children need to be evaluated by paediatricians or teams familiar with AI.
Children from IAs are at higher risk of infection. Thus, they must undergo serology testing for viruses (hepatitis A, B and C, and HIV) and bacterial infections (syphilis), parasite infections (intestinal helminths, Giardia) and latent tuberculosis.
The data contributed by this study can guide both primary care paediatricians and professionals that specialise in IA.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Martínez Ortiz A, Domínguez Pinilla N, Wudineh M, González-Granado LI. Adopción internacional de Etiopía en un período de 5 años. An Pediatr (Barc). 2015;82:302–307.