To describe the ophthalmological conditions seen in children adopted internationally by Spanish families, and to assess the influence of the region of origin and the preadoption period of institutional care on these conditions.
Materials and methodsA descriptive, observational, cross-sectional study was conducted on 232 children divided into four groups according to region of origin: Group 1, Eastern Europe (n=95); Group 2, Asia (n=95); Group 3, Central and South America (n=26); and Group 4, Africa (n=16). A complete ophthalmological study was carried out and the groups were compared for the prevalence of ophthalmological conditions.
ResultsAmong the total, 57.8% (134) of children presented ophthalmological abnormalities. The prevalence of ametropia was strongly correlated with the region of origin, and was significantly higher in Group 3 (65.4%) compared to the remaining groups. Strabismus and optic nerve hypoplasia (15.8% and 3.2%, respectively) were more prevalent in Group 1. The preadoption institutional care period was longer in children in Groups 1 and 3 (24.5 and 27.7 months, respectively).
ConclusionsChildren adopted from Central and South America had the highest prevalence of ametropia. Adopted children from Eastern Europe showed a weak tendency to present strabismus and optic nerve hypoplasia. Adoptive parents, paediatricians and ophthalmologists should be aware of the high prevalence of ophthalmologic conditions in internationally adopted children and provide the means for a prompt diagnosis and appropriate treatment.
Los niños adoptados tienen una mayor prevalencia de patología oftalmológica. El objetivo es estudiar la patología oftalmológica en niños españoles procedentes de adopción internacional, valorando la influencia de la región geográfica de origen y del periodo institucional preadoptivo.
Material y métodosSe realizó un estudio prospectivo en 232 niños. Se establecieron 4 grupos según la región geográfica de origen: grupo 1: Europa del Este (n=95); grupo 2: Asia (n=95); grupo 3: América Central y Sudamérica (n=26), y grupo 4: África (n=16). Se realizó un estudio oftalmológico completo.
ResultadosEl 57,8% (134) de los niños presentaron patología oftalmológica. La prevalencia de ametropía se correlacionó significativamente con la región geográfica de origen, siendo estadísticamente superior en el grupo 3 (65,4%) con respecto a la del resto de grupos. El estrabismo y la hipoplasia del nervio óptico fueron más prevalentes en el grupo 1 (el 15,8 y el 3,2%, respectivamente). El periodo institucional preadoptivo fue significativamente mayor en los niños de los grupos 1 y 3 (24,5 y 27,7 meses, respectivamente).
ConclusionesLos niños procedentes de adopción internacional de América Central y Sudamérica son el grupo con mayor prevalencia de ametropía. A pesar de no existir diferencias estadísticamente significativas, los niños procedentes de Europa del Este presentaron una mayor tendencia a presentar estrabismo e hipoplasia de nervio óptico. Los padres adoptivos, pediatras y oftalmólogos deben conocer la elevada prevalencia de problemas oftalmológicos y velar por un diagnóstico precoz y un tratamiento adecuado.
International adoption has increased exponentially in the past two decades.1 In Spain, international adoptions are increasingly frequent.2
Internationally adopted children have specific characteristics that may lead to disease: prenatal exposure to alcohol, drugs, tobacco or other substances. They usually live in overcrowded quarters, with poor hygiene conditions, inadequate or insufficient nutrition and a limited number of caregivers. Many of them come from regions endemic for specific infectious diseases.3
Children at a severe disadvantage receive deficient health care, so they are susceptible to developing a greater number of diseases.4
Many of these factors may affect immature visual pathways and developing eyes.
Although there are some references to the visual and ocular status of internationally adopted children in the literature,1 only one study has been published specifically on this subject. There is a high prevalence of ophthalmological findings in children adopted from Eastern Europe.5 Little is known about ophthalmological pathology in these children. A recent study has correlated ophthalmological and neuropaediatric findings in children adopted from Eastern Europe.6
This paper presents the first systematic study on the ocular and visual status of children adopted from different regions.
Materials and methodsFrom January 2010 to January 2012, the ophthalmology department of the Fundació Hospital de Nens of Barcelona studied 232 internationally adopted children. This prospective study was approved by the research council of the Fundació Hospital de Nens de Barcelona (University of Barcelona).
All patients were assessed by the same multidisciplinary team consisting of a paediatric ophthalmologist, a paediatric optometrist and a paediatrician specialised in international adoption.
Characteristics of participantsThe study included all children assessed by the adopted children's unit, irrespective of the presence or absence of ophthalmological symptoms.
The 232 children in our study had been adopted by 216 families.
The female to male ratio was 1.37 (134 girls; 98 boys). The mean age±standard deviation was 4.4±2.9 years.
We classified children into four groups by geographical region of origin: Group 1: Eastern Europe (n=95); Group 2, Asia (n=95); Group 3, Central and South America (n=26); and Group 4, Africa (n=16).
Group 1 included children from Russia, Kazakhstan, Ukraine and Bulgaria. Group 2 included children from China, India, Nepal and Cambodia. Group 3 included children from Guatemala, Peru, Colombia, Mexico, Dominican Republic, Haiti and Panama. Group 4 included children from Ethiopia, Morocco, Mali, Ivory Coast and Madagascar.
China was the most frequent country of origin (n=73), followed by Russia (n=63).
The routine ophthalmological evaluation included the following.
Measurement of visual acuityVisual acuity (VA) was measured in all patients after refractive correction.
Visual acuity for far vision was measured at a distance of 6m using Snellen charts.
We used the Pigassou chart with young children that were not cooperative with the Snellen chart.
We defined amblyopia as a corrected VA at least two lines below the standard criteria for age, based on the Snellen chart, that could not be explained by structural abnormalities of the eyeball.
RefractionWe performed cycloplegic and noncycloplegic retinoscopy.
We defined hyperopia as an error of 1.25 dioptres (D) or more in either of the eyes, myopia as an error of 0.5D or more in either of the eyes, and astigmatism as a difference of at least 0.75D between the two principal meridians of the cornea in either of the eyes.
Testing for strabismus and ocular motilityOcular alignment was assessed by means of the Hirschberg test. We documented the type of strabismus found (esotropia, exotropia and vertical misalignment). We analysed the esotropia to exotropia ratio. We documented anomalous movements and deficiencies in versions and ductions.
Examination of the anterior segment, ocular media and fundusThe anterior segment of the eye was evaluated by slit lamp biomicroscopy.
The fundus of the eye was explored by binocular indirect ophthalmoscopy.
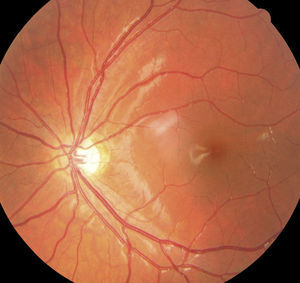
RetinographyWe performed retinographies to optimise the diagnosis of optic nerve hypoplasia (ONH) and retinal vascular tortuosity (RVT). To diagnose ONH we calculated the ratio of the distance from the fovea to the centre of the optic disc and the largest optic disc diameter. ONH was defined as a ratio greater than 3.7
For RVT we used the indices for tortuosity of arteries (ITA) and for tortuosity of veins (ITV). These indices were defined as path length of the vessel divided by the linear distance from the vessel origin to the reference circle, the radius of which was half the distance between the centre of the optic disc and the fovea. The presence of RVT was defined as an ITA and/or an ITV greater than 1.17 and 1.09, respectively.6
Ocular and visual pathology was categorised into three groups:
- 1.
Amblyopia.
- 2.
Refractive ocular pathology: ametropia.
- 3.
Nonrefractive ocular pathology.
To classify nonrefractive ocular pathology, we established 11 nosological groups: (1) disorders of lids and lashes; (2) nasolacrimal duct obstruction; (3) infection; (4) inflammation; (5) disorders of the cornea; (6) congenital malformations; (7) neoplasias; (8) strabismus; (9) neuro-ophthalmic disorders; (10) retinopathy; and (11) reading difficulties.
We considered that reading difficulties existed when one or the following criteria were met:
- 1.
Performance in reading speed test below results expected for age. We used the Developmental Eye Movement test, which allows the quantification of the relationship between vertical and horizontal reading speed.
- 2.
Fixation in near vision lasting less than 10s.
- 3.
Saccadic movements of great amplitude, rigid and/or imprecise and/or with intermediate fixations.
We started the study without knowing how many children from each region of origin would be included in the study. For this reason, we did not calculate the minimum sample size. However, the final sample size corresponds to a power of 80% for an odds ratio of 2.4 to be statistically significant in the larger groups.
Statistical analysisWe present continuous variables as means±standard deviations, and categorical variables as frequencies and percentages. We used Student's t test for the comparison of continuous variables and Pearson's chi square test for the comparison of categorical variables. We used a multivariate logistical regression method to estimate odds ratios and 95% confidence intervals.
All the statistical analyses were done using R: A language and environment for statistical computing (R Foundation for Statistical Computing, Vienna, Austria).
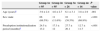
ResultsSample characteristicsTable 1 summarises the general characteristics of the sample.
The age of the children from Central and South America was significantly higher than the age of children in other groups (P<.001).
The preadoption institutionalisation period was significantly longer in children adopted from Eastern Europe and Central and South America (P<.001).
A duration of institutionalisation longer than 24 months in the preadoption period was associated with age (P=.028), sex (P<.034) and the geographical region of origin (P<.001). Institutionalisation lasted longer than 24 months in 57.4% of children from Eastern Europe (Table 2).
Factors related to a preadoption institutionalisation period longer than 24 months.
| PIP>24 months | P value | ||
|---|---|---|---|
| Non=164 | Yesn=68 | ||
| Age (years)a | 4.2±2.6 | 5.0±2.7 | .028 |
| Sex: male | 62 (37.8%) | 36 (52.9%) | .034 |
| GRO | <.001 | ||
| Eastern Europe | 56 (34.1%) | 39 (57.4%) | |
| Asia | 82 (5.0%) | 13 (19.1%) | |
| Central and South America | 13 (7.9%) | 13 (19.1%) | |
| Africa | 13 (7.9%) | 3 (4.4%) | |
| Ametropia | 68 (41.5%) | 26 (38.2%) | .648 |
| Hyperopia | 44 (26.8%) | 15 (22.1%) | .448 |
| Myopia | 6 (3.7%) | 5 (7.4%) | .307 |
| Astigmatism | 36 (22%) | 12 (17.6%) | .648 |
| Amblyopia | 11 (6.7%) | 7 (1.3%) | .353 |
| NROP | 56 (34.1%) | 30 (44.1%) | .152 |
GRO, geographical region of origin; NROP, nonrefractive ocular pathology; PIP, preadoption institutionalisation period.
We found ophthalmological abnormalities in 134 of the internationally adopted children (57.8%).
The results for amblyopia and ametropia are summarised in Table 3.
Amblyopia and ametropia results.
| Group 1n=95 | Group 2n=95 | Group 3n=26 | Group 4n=16 | P value | |
|---|---|---|---|---|---|
| Amblyopia | 5 (5.3%) | 11 (11.6%) | 2 (7.7%) | 0 (0.0%) | |
| Ametropia | 34 (35.8%) | 39 (41.1%) | 17 (65.4%) | 4 (25.0%) | .027 |
| Type of ametropiaa | |||||
| Hyperopia | 14 (14.7%) | 20 (21.1%) | 5 (19.2%) | 2 (12.5%) | |
| Myopia | 1 (1.1%) | 1 (1.1%) | 3 (11.5%) | 0 (0.0%) | |
| Astigmatism | 12 (12.6%) | 8 (8.4%) | 4 (15.4%) | 0 (0.0%) | |
The mean uncorrected monocular VA was 0.81. The mean corrected VA was 0.86. We detected amblyopia in 18 patients (7.8%).
RefractionRefraction errors were diagnosed in 94 patients (40.5%).
Of all patients, 25.4% had hyperopia, 4.7% myopia, and 20.7% astigmatism. We found statistically significant differences in the prevalence of refractive errors between geographical regions of origin (P<.027), even after adjusting for age and sex (polychotomous logistic regression) (Table 4).
Adjustment for potential confounding factors like age, preadoption institutionalisation period, sex and nonrefractive ocular pathology. Children from Central and South America were the group at highest risk of having ametropia.
| Odds ratio | 95% CI | P value | ||
|---|---|---|---|---|
| Lower | Upper | |||
| Geographical region of origin | ||||
| Africa | Reference | |||
| Eastern Europe | 1.81 | 0.51 | 6.46 | 0.363 |
| Asia | 3.2 | 0.85 | 12.09 | 0.086 |
| Central and South America | 10.2 | 2.22 | 46.81 | 0.003 |
| Age (years) | 1.01 | 0.91 | 1.13 | 0.816 |
| Sex: male | 1.86 | 0.92 | 3.79 | 0.085 |
| Preadoption institutionalisation period | 0.99 | 0.96 | 1.01 | 0.201 |
| Nonrefractive ocular pathology | 2.77 | 1.55 | 4.96 | 0.001 |
Ametropia was significantly more prevalent in children adopted from Central and South America (P<.027). Hyperopia and myopia were most prevalent in children from Central and South America (30.8% and 19.2%, respectively). Astigmatism was most prevalent in children from Central and South America and from Eastern Europe (34.6 and 20%, respectively), and the differences between these groups did not reach statistical significance (P=.3).
The presence of ametropia correlated significantly with the geographical region of origin (P=.027) and with the presence of nonrefractive ocular pathology (P=.002) (Table 5).
Factors associated with the presence of ametropia.
| Ametropia | P value | ||
|---|---|---|---|
| Non=138 | Yesn=94 | ||
| Age (years) | 4.4 (2.6) | 4.5 (2.8) | 0.756 |
| Sex (male) | 55 (39.9%) | 43 (45.7%) | 0.373 |
| PIP | 21.4 (15.0) | 20.6 (13.1) | 0.679 |
| GRO | 0.027 | ||
| Eastern Europe | 61 (44.2%) | 34 (36.2%) | |
| Asia | 56 (40.6%) | 39 (41.5%) | |
| Central and South America | 9 (6.5%) | 17 (18.1%) | |
| Africa | 12 (8.7%) | 4 (4.3%) | |
| NROP | 40 (29.0%) | 46 (48.9%) | 0.002 |
| Palpebral pathology | 10 (7.2%) | 7 (7.4%) | 0.954 |
| Tear duct obstruction | 6 (4.3%) | 1 (1.1%) | 0.246 |
| Infection | 1 (0.7%) | 2 (2.1%) | 0.567 |
| Inflammation | 0 (0.0%) | 3 (3.2%) | 0.065 |
| Corneal pathology | 0 (0.0%) | 1 (1.1%) | 0.405 |
| Congenital malformations | 5 (3.6%) | 5 (5.3%) | 0.531 |
| Neoplasias | 1 (0.7%) | 0 (0.0%) | 1 |
| Strabismus | 16 (11.6%) | 24 (25.5%) | 0.006 |
| Neuro-ophthalmic pathology | 2 (1.4%) | 4 (4.3%) | 0.226 |
| Retinal pathology | 3 (2.2%) | 1 (1.1%) | 0.649 |
| Reading difficulties | 5 (3.6%) | 5 (5.3%) | 0.531 |
GRO: geographical region of origin; NROP, nonrefractive ocular pathology; PIP: preadoption institutionalisation period.
Table 6 summarises the results for this category.
Results for nonrefractive ocular pathology.
| Group 1n=95 | Group 2n=95 | Group 3n=26 | Group 4n=16 | P value | |
|---|---|---|---|---|---|
| NROP | 41 (43.2%) | 34 (35.8%) | 6 (23.1%) | 5 (31.2%) | 0.262 |
| Palpebral pathology | 2 (2.1%) | 9 (9.5%) | 0 (0.0%) | 1 (6.2%) | a |
| Tear duct obstruction | 2 (2.1%) | 2 (2.1%) | 0 (0.0%) | 1 (6.2%) | a |
| Infection | 0 (0.0%) | 2 (2.1%) | 1 (3.8%) | 0 (0.0%) | a |
| Inflammation | 2 (2.1%) | 0 (0.0%) | 1 (3.8%) | 0 (0.0%) | a |
| Corneal pathology | 0 (0.0%) | 1 (1.1%) | 0 (0.0%) | 0 (0.0%) | a |
| Congenital malformations | 3 (3.2%) | 1 (1.1%) | 0 (0.0%) | 0 (0.0%) | a |
| Neoplasiasa | |||||
| Strabismus | 15 (15.8%) | (14.7%) | 1 (3.8%) | 2 (12.5%) | a |
| Neuro-ophthalmic pathology | 2 (2.1%) | 1 (1.1%) | 0 (0.0%) | 0 (0.0%) | a |
| Retinal pathology | 4 (4.2%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | a |
| Reading difficulties | 2 (2.1%) | 2 (2.1%) | 2 (7.7%) | 1 (6.2%) | a |
NROP: nonrefractive ocular pathology.
We did not find statistically significant differences in the prevalence of nonrefractive ocular pathology between the groups by geographical region of origin (P=.26).
Palpebral conditions were most prevalent in children from Asia, but the difference was not statistically significant (P=.17). Palpebral abnormalities were found in 17 children: ptosis (n=10), entropion (n=4), euryblepharon (n=2) and trichomegaly (n=2).
Nasolacrimal duct obstruction was diagnosed in five children.
Eye infection was diagnosed in three children.
Eye inflammation was diagnosed in three patients: phlyctenular keratoconjunctivitis, allergic conjunctivitis and toxoplasmic chorioretinitis.
One boy from China had paracentral corneal leukoma.
Ten children had congenital ocular anomalies. Eight of them were from Group 1.
Hypertelorism was diagnosed in two children. One boy from Bulgaria had congenital nonmalignant bilateral exophthalmos.
Dyschromatopsia was diagnosed in one patient.
We found four cases of ONH among the children adopted from Russia (Fig. 1). Septo-optic dysplasia was ruled out in every case, and only one had a clear history of maternal alcohol consumption during pregnancy.
A child from China was diagnosed with optic disc dysplasia.
A patient with neurofibromatosis type 1 had an optic nerve glioma.
The total percentage of strabismus was 13.8% (n=32).
The esotropia to exotropia ratio was 1.21:1. Strabismus was more prevalent in the group from Eastern Europe (22.1%), although the difference was not statistically significant (P=.35).
Six children were diagnosed with neuro-ophthalmic disorders. They all came from Russia.
Bernard-Horner syndrome was diagnosed in three children after ruling out neuroblastoma in all of them. Congenital nystagmus was diagnosed in two children, and slow pupillary light reflex in one patient.
Retinal vascular tortuosity was diagnosed in four children from Group 1 (4.2%) (Fig. 2).
Ten children were diagnosed with reading difficulties. The highest proportion of reading difficulties was found in children from Group 3 (11.5%).
DiscussionWe found ocular and vision disorders in 57.8% of the children under study. Few studies have assessed ophthalmological disorders in internationally adopted children. Grönlund et al.5 described a high frequency of ophthalmological findings (78%) in a population of children adopted from Eastern Europe. An association between these ophthalmological findings and neuropaediatric pathology has been established recently.6
When it comes to non-ophthalmological disorders, different studies show a greater prevalence of systemic pathology in internationally adopted children compared to non-adopted children and different prevalences depending on ethnic group and geographical region of origin.8,9 Children adopted from Ethiopia, who live with relatives for longer periods of time before being institutionalised, have fewer developmental delays and better growth.10 There is agreement that the longer the period of institutionalisation, the greater the incidence of pathology in adopted children.
In our study, the preadoption institutionalisation period was significantly longer in children from Groups 1 and 3. Institutionalisation lasting more than 24 months correlated with age, sex, and geographical region of origin. The preadoption institutionalisation period was longer in older children, in boys, and in children from Eastern Europe. In Group 1, the preadoption institutionalisation period was longer than 24 months in 57.4% of the children.
In our study, the prevalence of ametropia was 40.5%, while it is 7.7% in populations of non-adopted children.11
Although small differences between ethnic groups have been described in the prevalence of refraction errors in non-adopted children,12 our study found that ametropia was significantly more prevalent in children adopted from Central and South America.
Children from Central and South America had the highest prevalence of hyperopia. Myopia was most prevalent in children from Central and South America. Astigmatism was most prevalent in children from Central and South America and Eastern Europe. The presence of ametropia correlated significantly with the geographical region of origin and with the presence of nonrefractive ocular pathology.
Malnutrition in the early stages of life interferes with vision development. There is evidence that children affected by severe malnutrition in the first six months of life have a higher prevalence of ametropia (astigmatism and myopia), increased optic nerve cupping and RVT.13 In our series, we found RVT in four children from Group 1. Grönlund et al.6 found an 11% increase in the ITA and a 9% increase in the ITV in their sample of adopted children.
Vitamins and minerals, especially zinc, are essential to the development of the ocular globe and vision. Zinc is an essential cofactor in the metabolism of neurotransmitters, fatty acids, prostaglandins and melatonin.14 The most frequent ophthalmological manifestation of severe zinc deficiency is periocular vesiculopustular rash,15 which we did not find in any of our patients.
In populations that suffer from malnutrition, 45% of children develop iron deficiency anaemia.16 Iron is essential to the development of the central nervous system, cellular differentiation, protein and hormone synthesis and different pathways of cellular metabolism,17 even in the optic pathways. There is evidence that suggests that myelination may be partially dependent on iron.18 Given the importance of nutrition in the early months of life, prospective studies need to be conducted to assess the relationship between the nutritional status of these children and ophthalmological pathology.
Maternal smoking during pregnancy has a negative impact on the foetus and the child.19 The higher mean hyperopia values in children exposed to tobacco smoke during gestation and childhood suggests that environmental factors related to tobacco use may have long-term effects on refraction.20 A study published recently21 demonstrated that patients that smoke are at higher risk of recurrence of ocular inflammatory diseases.
In our study, children adopted from Eastern Europe (Group 1) had the highest prevalence of strabismus and optic nerve hypoplasia, although the difference did not reach statistical significance. The total percentage of children that had strabismus in our series was 13.8%. The prevalence of strabismus in another series of adopted children was 32%,5 while the prevalence in non-adopted children ranges from 3% to 8%.22
In our study, esotropia was more prevalent than exotropia (esotropia to exotropia ratio, 1.21). Other authors have reported ratios greater than 2 in studies of adopted5 and non-adopted11 children.
We found four cases of ONH among the children adopted from Russia. A history of maternal alcohol consumption during pregnancy was only verified in one, probably because this fact is usually not known or not reported by adoptive parents. Grönlund et al.5 reported a similar prevalence of ONH (4/72; 5.5%) in a group of children adopted from Eastern Europe.
We did not find optic neuritis caused by lead in children from China, even though 14% of these children had high serum levels of this metal.23
The high prevalence of strabismus and ONH in children adopted from Eastern Europe may be related to alcohol and substance use. Russia has a high rate of alcohol consumption per capita, and the use of illegal drugs has been increasing. Alcohol affects synaptogenesis in the foetal brain,24 inducing neuronal degeneration.
The prevalence of prenatal exposure to illegal drugs in internationally adopted children is unknown. Many countries do not document this information to avoid unflattering publicity.25
In our study, amblyopia was diagnosed in 18 children (7.8%). In the general paediatric population, 2% of the children develop amblyopia, while Grönlund et al.5 found a prevalence of 15% in their series of children adopted from Russia. We found the highest frequency of amblyopia in children from Group 2 (11/95; 11.6%), although this finding was not statistically significant.
The higher prevalence of amblyopia in children from Group 2 may be due to malnutrition and visual understimulation. Most of the problems found in adopted children upon arrival to Spain have been attributed to deficient institutional care in early stages of development.26 A few institutionalised children had never been outdoors and had not been exposed to the visual stimulation required for the normal development of the optic pathway. Some caregivers in orphanages wear masks, depriving the children of the experience of seeing human faces.27 The visual stimuli of shapes, colours, contrasts and movement are essential to the correct development of VA and binocular vision. A lack of visual stimulation is associated with the pathogenesis of amblyopia.
This study emphasises the need for an initial ophthalmological assessment and the ophthalmological followup of all internationally adopted children. Paediatricians and adoptive parents must be watchful given the risk of visual abnormalities in these children, and provide the necessary resources for early diagnosis and treatment.
Conflicts of interestThe authors have no conflicts of interest to declare.
We want to thank Professor R. Jiménez for his valuable revision of the manuscript, and Dr Joan Salvador Vila del Parc from Recerca Biomèdica of Barcelona for his help in the statistical analysis of the data.
Please cite this article as: Cavero-Roig L, Díaz-Conradi Á, Negre-Loscertales A, Ferrero-Rosanas A, Salvador-Valle A, Burch-Piñol S, et al. Patología ocular en adopción internacional: importancia de la región de origen. An Pediatr (Barc). 2015;82:293–301.