Newborns with congenital chylothorax or chylothorax secondary to cardiac or thoracic surgery are at high risk of malnutrition and infection due to continuous losses of fat, albumin and lymphocytes in the chyle.1 Treatment usually consists in placement of a chest drain, restriction of long-chain triglycerides and, therefore, discontinuation of breastfeeding, parenteral nutrition and enteral nutrition with formulas with medium-chain triglycerides (MCTs) as the sole for a period ranging from 2 to 6 weeks, which usually results in permanent discontinuation of breastfeeding.
In order to optimise nutrition in these patients, the personalised nutrition unit (PNU) in our hospital, which has been operating since 2018, offers the possibility of centrifuging human milk (HM) to remove the fat while maintaining certain immune features that may have an additional beneficial effect in this population of immunosuppressed patients.
We conducted a retrospective descriptive study in newborns (NBs) with chylothorax secondary to surgery that received centrifuged maternal or donor HM supplemented with fats in order to optimise energy and nutritional intake.
The PNU is an on-site production unit within the department of neonatology that meets all the standards of the Asociación Española de Bancos de Leche (Spanish Association of Human Milk Banks),2 where all the donors are mothers of hospitalised NBs.
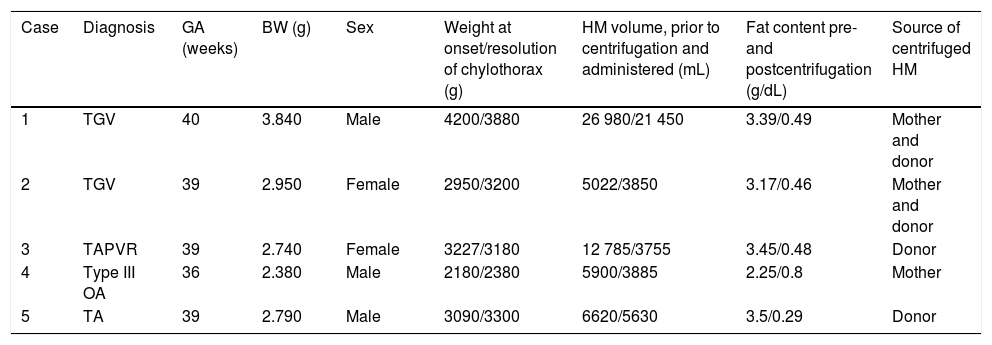
We describe epidemiological and clinical variables in 5 NBs with postsurgical chylothorax in 2018, as well as the volumes of milk contributed by donor mothers and the volumes obtained after centrifugation, along with their respective fat contents (Table 1). Table 2 summarises relevant clinical and outcome data.
Patient characteristics and volume and fat content of processed human milk.
| Case | Diagnosis | GA (weeks) | BW (g) | Sex | Weight at onset/resolution of chylothorax (g) | HM volume, prior to centrifugation and administered (mL) | Fat content pre- and postcentrifugation (g/dL) | Source of centrifuged HM |
|---|---|---|---|---|---|---|---|---|
| 1 | TGV | 40 | 3.840 | Male | 4200/3880 | 26 980/21 450 | 3.39/0.49 | Mother and donor |
| 2 | TGV | 39 | 2.950 | Female | 2950/3200 | 5022/3850 | 3.17/0.46 | Mother and donor |
| 3 | TAPVR | 39 | 2.740 | Female | 3227/3180 | 12 785/3755 | 3.45/0.48 | Donor |
| 4 | Type III OA | 36 | 2.380 | Male | 2180/2380 | 5900/3885 | 2.25/0.8 | Mother |
| 5 | TA | 39 | 2.790 | Male | 3090/3300 | 6620/5630 | 3.5/0.29 | Donor |
BW, birth weight; GA, gestational age; HM, human milk; OA, oesophageal atresia; TA, tricuspid atresia; TAPVR, total anomalous pulmonary venous return; TGV, transposition of the great vessels.
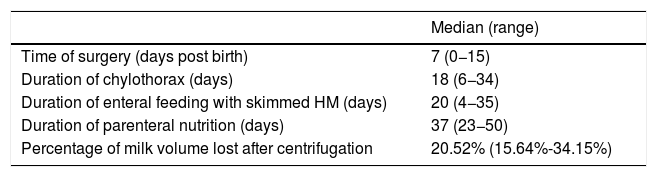
Clinical and outcome data for the sample.
| Median (range) | |
|---|---|
| Time of surgery (days post birth) | 7 (0−15) |
| Duration of chylothorax (days) | 18 (6−34) |
| Duration of enteral feeding with skimmed HM (days) | 20 (4−35) |
| Duration of parenteral nutrition (days) | 37 (23−50) |
| Percentage of milk volume lost after centrifugation | 20.52% (15.64%-34.15%) |
HM, human milk.
Chylothorax was identified as a complication of surgery between 24 h and 15 days after the procedure, requiring pleural drainage in every case and mechanical ventilation in 80% of cases. The median duration of mechanical ventilation required in the management of chylothorax was 10 days (range, 0–70). In 80% of cases, the centrifuged HM used in enteral nutrition was supplemented with MCTs to a maximum concentration of 5 mL/100 mL. Administration of HM did not preclude the need to administer formula with MCTs as the sole fat (Monogen®), which had to be prescribed to every patient due to an insufficient stock of centrifuged HM. In 3 out of 5 cases, the patient gained weight throughout the course of chylothorax.
The PNU makes it possible to administer HM from the mother or a donor to infants with chylothorax after a process of centrifugation at 3000 rpm and 2°C lasting 15 min.3 The solidified fat layer is then removed manually with a spatula and the liquid portion filtered through sterile gauze to facilitate the removal of any remaining visible fat, a stage that is carried out under sterile conditions in a laminar flow hood. The milk is subsequently pasteurised and stored frozen in bottles until it is used. Pasteurization allows the use as donor milk for other patients of the milk of mothers of infants whose chylothorax has resolved if any bottles remain in storage, something that is possible given the variable duration of chylothorax. In our study, this occurred in 2 cases (Table 1), and all the centrifuged HM was pasteurised.
The fat content of HM prior to centrifugation was lower compared to other studies in the literature, as in many cases NBs received HM from the mother in the early days of life, which has a lower fat content (transitional milk or early mature milk). The final fat content was similar to that described in other studies (< 1 g/100 mL).3,4 We did not find significant differences in the protein content of HM in the analyses performed before and after centrifugation.
The use of centrifuged HM allows adjustment of the fat content to current guidelines for nutritional management of chylothorax, which in our case series never lasted longer than 4 weeks. There was no case of recurrence of chylothorax after resumption of breastfeeding without centrifugation. Calorie supplementation achieved a reduction of weight loss relative to what has been described in the previous literature.5 This process allowed maintenance of breastfeeding in 4 of the 5 patients in the sample after resolution of the chylothorax. The PNU makes it possible to administer mature centrifuged HM from other mothers, thus meeting the requirements of patients whose mothers cannot offer their own HM. Pasteurization can be omitted if the centrifuged HM is not going to be donated and will only be used by that mother’s own infant, as has been described by other authors.5
Optimising Holder pasteurization by adjusting treatment settings to recent recommendations has proven to better preserve certain immunoactive components of milk such as IgA, lysozyme and lactoferrin.6 These and other components are essential to the protection of infants against infection, especially in those at increased risk as are infants with chylothorax. In our PNU, the pasteurization and cooling processes are automated and allow control and monitoring to verify the different phases of Holder pasteurization (Beldico PA 45® pasteurizer).
Our study has the limitations intrinsic to retrospective descriptive studies. Due to the small sample size, larger studies are needed to determine the clinical relevance of its findings.
The availability of a PNU facilitates maintenance of breastfeeding in infants with chylothorax. Due to losses in milk volume due to the centrifuging process, it is necessary to produce substantial amounts of milk and, in some cases, to resort to donated HM.
We thank the Laboratory of Molecular Immune Biology and the HIV BioBank of the Hospital Gregorio Marañón led by Dr María Ángeles Muñoz for allowing us access to the 5810R centrifuge to produce the skimmed milk. We also thank all lactating donors for their generosity and invaluable contribution, without which all of these infants would be unable to receive human milk.
Please cite this article as: Luna MS, Martín SC, de Orgaz MdCSG, Corrales ER, Blanco AJ. Leche materna descremada en recién nacidos con quilotórax: opciones con una unidad de nutrición personalizada. An Pediatr (Barc). 2020;93:194–195.