Recent epidemiological studies report paracetamol use in 65% of pregnant women.1 Although it is known that paracetamol can cross the human placenta, there is no evidence of it producing foetal complications in animal models, and it is considered a safe drug during pregnancy.2 For this reason, paracetamol is the first-line analgesic drug used in pregnant women. However, some authors have reported finding an association between paracetamol use in pregnant women and the development of attention-deficit hyperactivity disorder and autism spectrum disorder,3 asthma,4 criptorquidism5 and foetal ductus arteriosus closure.6 In reference to neonatal complications, there have been reports of newborns with heart failure and pulmonary hypertension with a known history of intrauterine exposure to paracetamol and ductus arteriosus closure. Allegaert et al. reviewed a case series in October 2018 and concluded that a causal relationship is highly probable,6 as paracetamol has been proven to be effective for therapeutic closure of patent ductus arteriosus in preterm infants.
The aim of our study was to describe the use of paracetamol by pregnant women in our area and assess their knowledge of the potential side effects of the drug on the foetus. A secondary objective was to analyse which health care professional provided this information.
We designed a prospective study with collection of data through a questionnaire administered to women admitted to the maternity ward of our hospital over a period of 3 months.
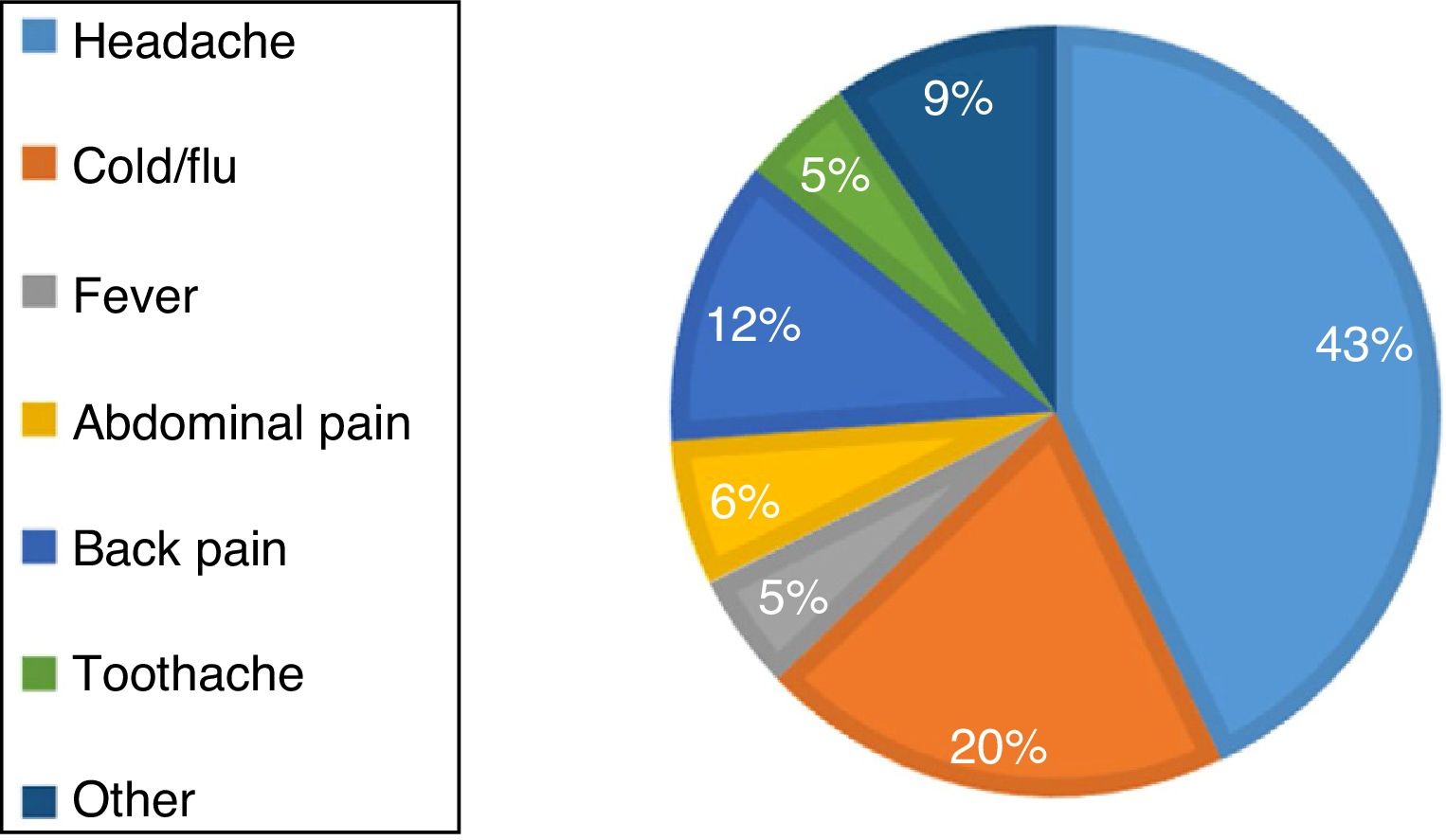
We received 900 completed questionnaires (93% of mothers in the maternity ward during the period under study). A majority of respondents had a university degree (55.5%). Of the total, 67.4% reported having used paracetamol during pregnancy, a proportion that was slightly larger compared to the previous literature. Most respondents (99%) consumed the therapeutic dose (< 4 g/day) and nearly half (45.7%) used it for a very short time interval (< 3 days). The most common reasons of paracetamol consumption are shown in Figure 1. The maximum daily dose of 4 or more grams per day was prescribed for management of headache (50% of cases), cold symptoms (33.3%) or toothache (16.7%). The distribution of paracetamol was similar in every trimester of pregnancy; 12.5% of respondents used it over 2 trimesters and 21.5% throughout the pregnancy.
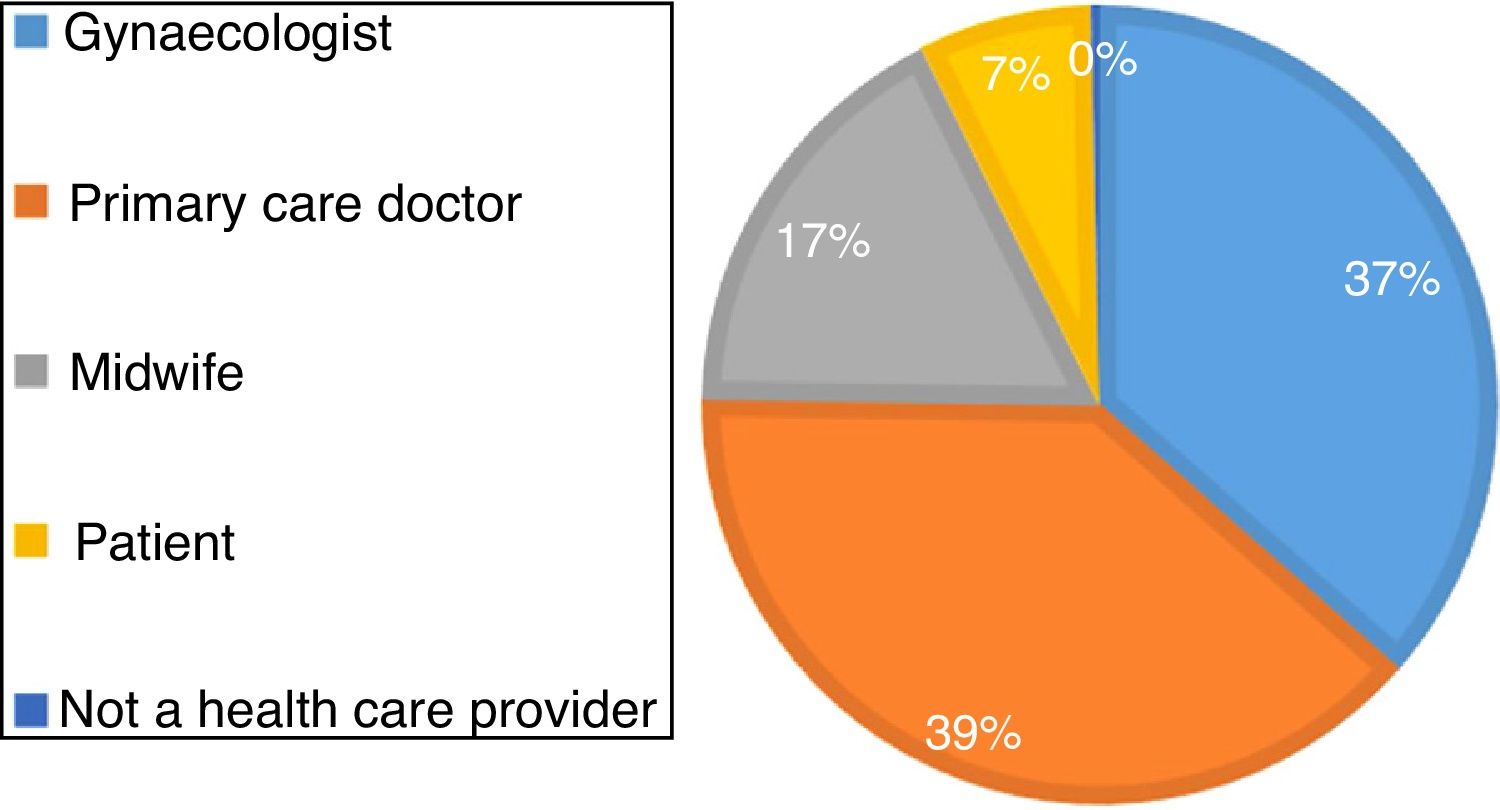
The prescription was made most frequently by the primary care doctor (39%) or the gynaecologist (37%) (Fig. 2). When it came to knowledge about the drug, 26% of pregnant women believed that paracetamol had no effects on the foetus. In addition, 51.9% of pregnant women had received information from a health care professional about the effects of paracetamol. Of the group that had received information, 74% reported being told that consumption of paracetamol carried no risks to the foetus. Our study reflects the current situation in the use of paracetamol by pregnant women and in the education given by health care providers in a metropolitan area with a population characterised by a medium-to-high educational attainment.
When it comes to the limitations of this study, given the high educational attainment of the survey respondents, most of who had a university degree, our findings may not be generalised to the general population. On the other hand, given the high response rate, our sample is representative of the population under study. Another limitation is that the items explore retrospective information, so there is a risk of recall bias. The questionnaire did not investigate how long participants consumed the maximum dose of paracetamol. Analysing neonatal outcomes was not an objective of our study. However, it would be relevant to carry out another study with an appropriate design to assess the safety of prescribing paracetamol during pregnancy, as the current evidence on the subject is scarce.
In conclusion, use of paracetamol in pregnant women in our area was greater than reported in the literature, and the information that they received on the potential adverse effects or the dosage that is considered safe was inadequate. Until the quality of the evidence improves, public health education strategies should be implemented to guarantee delivery of sufficient information and to facilitate the search for alternatives encouraging rational use of this drug in order to control consumption during pregnancy.
Please cite this article as: Castillo Barrio B, Bravo Laguna MC, de la Calle Fernández M, Pellicer Martinez A. Consumo de paracetamol durante la gestación. An Pediatr (Barc). 2020;93:196–197.
Previous presentations: This study was presented at the XXVII Congress of Neonatology and Perinatal Medicine and the VII Congress of Neonatal Nursing; October, 2019, Madrid, Spain.