Simulation-based medical education, which allows clinicians to develop skills to manage serious and infrequent situations without detriment of patient safety,1 is even more important during unexpected public health emergencies like the pandemic we are currently experiencing.2
The coronavirus disease 2019 (COVID-19) pandemic has brought on numerous adjustments that have limited the pursuit of medical education activities,3 including the development of simulation programmes. Therefore, we need to contemplate the development of other modalities of simulation, such as remote simulation, to substitute or supplement in situ simulation training to be able to continue implementing educational programmes.4–6
We present the results of a cross-sectional, observational survey-based study aimed at assessing the use of simulation for preparing clinicians to manage COVID-19 during the first and second waves of the pandemic at paediatric intensive care units in Spain, as well as the the simulation modalities used, and the continuation of simulation activities unrelated to COVID-19.
Nineteen Spanish paediatric intensive care units (PICUs) of different levels of care (Appendix A) submitted responses to the survey in December 2020. Ten of these units had simulation training programmes as part of their regular educational curriculum prior to the COVID-19 pandemic. More than half started implementing the COVID-19 trainings in March 2020, 8 were able to start the trainings before starting to manage COVID-19 patients, 2 started the trainings at the same time they started managing patients, and 9 after starting to manage patients. In 9 PICUs, the COVID-19 training programme was an initiative of the unit itself.
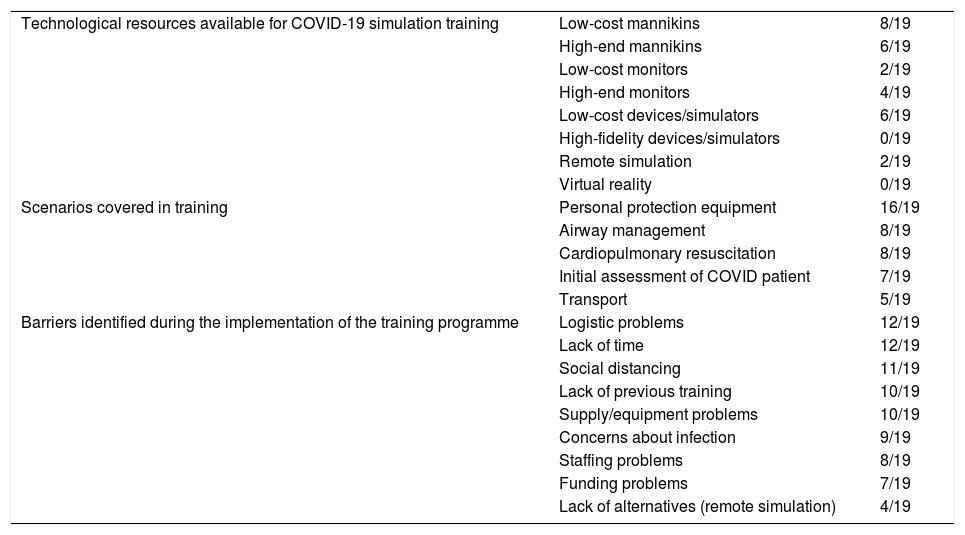
Table 1 presents the equipment and technology available to the units to deliver the training programmes, with a predominance of low-cost equipment. Only 2 units had access to the technological resources required to offer remote simulation, and none had access to virtual reality simulators.
Available technology, scenarios included in trainings and barriers identified by hospitals during the development of the COVID-19 simulation training programme expressed in number of hospitals over the total of 19 that participated.
| Technological resources available for COVID-19 simulation training | Low-cost mannikins | 8/19 |
| High-end mannikins | 6/19 | |
| Low-cost monitors | 2/19 | |
| High-end monitors | 4/19 | |
| Low-cost devices/simulators | 6/19 | |
| High-fidelity devices/simulators | 0/19 | |
| Remote simulation | 2/19 | |
| Virtual reality | 0/19 | |
| Scenarios covered in training | Personal protection equipment | 16/19 |
| Airway management | 8/19 | |
| Cardiopulmonary resuscitation | 8/19 | |
| Initial assessment of COVID patient | 7/19 | |
| Transport | 5/19 | |
| Barriers identified during the implementation of the training programme | Logistic problems | 12/19 |
| Lack of time | 12/19 | |
| Social distancing | 11/19 | |
| Lack of previous training | 10/19 | |
| Supply/equipment problems | 10/19 | |
| Concerns about infection | 9/19 | |
| Staffing problems | 8/19 | |
| Funding problems | 7/19 | |
| Lack of alternatives (remote simulation) | 4/19 |
The scenario covered most frequently in these trainings was the correct donning and doffing of personal protection equipment (PPE), followed by airway management and cardiopulmonary resuscitation (CPR) (Table 1). Most trainings were conducted in situ (in the patient care setting): 73.7% of trainings on the donning of PPE, 57.1% of trainings on airway management, 61.5% of CPR trainings and 63.6% of trainings on other scenarios. Less frequently, simulation trainings were delivered outside the unit in specific facilities or centres. A substantial proportion of units (13/19) delivered multidisciplinary trainings and 12/19 of the units included other departments in their training programme.
Table 1 presents the barriers identified by participating units in delivering the trainings, with a high percentage reporting logistic problems, a lack of time and a lack of staff. Have the units reported lack of previous training and concerns regarding infection. Social distancing measures affected training programmes in nearly 60% of units, and the lack of alternatives like remote simulation was another of the identified barriers. Units also frequently reported problems related to material resources and funding.
The main problems reported by participants regarding group dynamics were difficulty communicating due to wearing PPE in 12 of the 19 units, anxiety or concerns in the care team in 12, lack of knowledge of COVID-19 care practices in 9 and lack of knowledge of COVID-19 teamwork in 8. Compared to simulation-based training programmes offered prior to COVID-19, engagement of the team in trainings during the pandemic was the same in 9 of the units and greater in 7.
When it came to the continuation of simulation-based activities unrelated to COVID-19, 14 of the 19 units continued implementing simulation-based activities, although less frequently and with fewer participants. Only 5 of the units were able to continue the regular simulation-based training programme without significant adjustments. Only 3 units used remote simulation to offer simulation-based trainings unrelated to COVID-19.
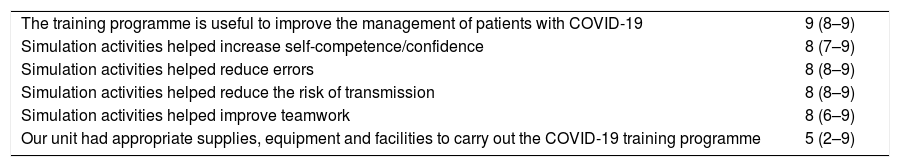
Participants considered the training programme useful to improve the management of patients with COVID-19 (Table 2).
Assessment by participants of COVID-19 simulation training programme, rated on a scale of 1 to 10 (expressed as median and interquartile range).
| The training programme is useful to improve the management of patients with COVID-19 | 9 (8–9) |
| Simulation activities helped increase self-competence/confidence | 8 (7–9) |
| Simulation activities helped reduce errors | 8 (8–9) |
| Simulation activities helped reduce the risk of transmission | 8 (8–9) |
| Simulation activities helped improve teamwork | 8 (6–9) |
| Our unit had appropriate supplies, equipment and facilities to carry out the COVID-19 training programme | 5 (2–9) |
Despite the potential limitations of the study, including the subjectivity of survey-based designs and that responses were only submitted by half of the PICUs in Spain, it reflects the use of simulation in this care setting during the COVID-19 pandemic. Simulation has been used to train in different scenarios related to COVID-19, mainly with low-cost technology and in situ trainings. Emerging modalities like remote simulation3,4 using different applications, including some inexpensive options,5–7 are still rarely used by Spanish PICUs. Despite the reported barriers, participants found the training programmes very useful.
Simulation-based medical education must be established as part of the regular training curriculum of all units delivering care to complex patients, such as PICUs. However, only half of the units had an established educational programme, and trainings on COVID-19 were mostly an initiative of the units themselves. It may be necessary to provide greater financial and material support and increase awareness of the usefulness of simulation-based medical education, as failing to do so could have a significant negative impact on the training of clinicians and patient safety.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Hospital Sant Joan de Déu, Hospital Universitario Fundación Jiménez Díaz, Complejo Hospitalario de Jaén, Hospital Clínico San Carlos, Hospital Universitario Central de Asturias, Hospital Universitario de Cruces, Hospital Universitario de Burgos, Complejo Asistencial Universitario de León, Complejo Hospitalario de Toledo, Hospital Virgen del Rocío, Hospital Universitario Gregorio Marañón, Hospital Universitario de Donostia, Hospital Universitario Puerta del Mar, Complejo Hospitalario Universitario de A Coruña, Hospital Clínico Universitario de Santiago de Compostela, Hospital Regional Universitario de Málaga, Hospital Clínico Universitario de Valladolid, Hospital Universitario Nuestra Señora de Candelaria.
Please cite this article as: Butragueño Laiseca L, Zanin A, López-Herce Cid J, Mencía Bartolomé S. Uso de la simulación durante la pandemia COVID-19 en las UCIP españolas. Nuevos retos en educación médica. An Pediatr (Barc). 2021;95:373–375.