Near-infrared spectroscopy (NIRS) is becoming a widespread method for monitoring of ill infants in neonatal intensive care units. The detection by NIRS of cerebral hypoxia in extremely preterm newborn infants and its correction with appropriate care measures decreases the time spent in hypoxia by the immature brain, although the evidence on the impact of NIRS monitoring on long-term neurodevelopmental outcomes is still not robust.1 Studies in adult patients with liver disease show that high levels of bilirubin may interfere significantly with cerebral NIRS monitoring, but this phenomenon has not been investigated in neonates.2–4 We present 4 cases of interference with NIRS monitoring in extremely low birth weight (ELBW) infants with conjugated hyperbilirubinaemia.
The ethics committee of our hospital approved the retrospective analysis as exempted it from the need to obtain informed consent. The patients were ELBW neonates born between 25+0 and 28+5 weeks of gestation with birth weights of 500 to 990 g who developed multifactorial cholestasis with progressive elevation of serum conjugated bilirubin. Concurrent to this process, we observed a reduction in the cerebral regional oxygen saturation (rSO2) measured by NIRS. Table 1 presents the clinical characteristics of the patients and Table 2 the changes over time in the levels of bilirubin and cerebral rSO2 measured by NIRS. In these 4 patients, the abnormal NIRS values could not be explained by abnormalities in haemoglobin concentration, partial pressure of CO2, oxygen saturation (SatO2), lactate levels or blood pressure. In every case, an ultrasound examination confirmed that cerebral blood flow (CBF) velocities and cardiac output were normal. In patients A and D, once they were stable and cholestasis had resolved (at 33 days and 4 months of age, respectively), NIRS monitoring was resumed and detected normal values.
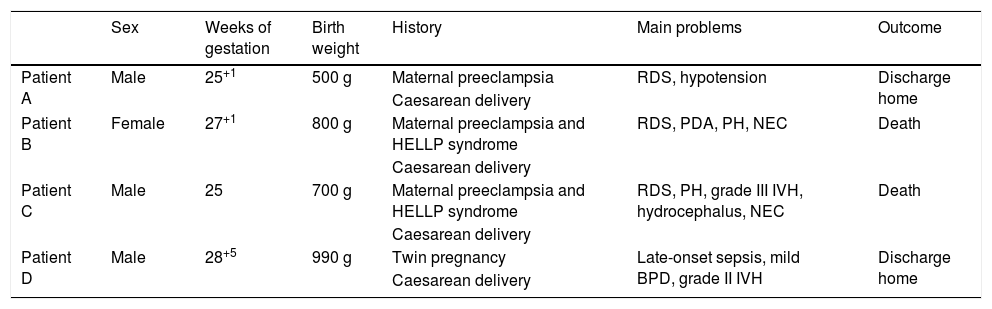
Clinical characteristics of the patients.
| Sex | Weeks of gestation | Birth weight | History | Main problems | Outcome | |
|---|---|---|---|---|---|---|
| Patient A | Male | 25+1 | 500 g | Maternal preeclampsia | RDS, hypotension | Discharge home |
| Caesarean delivery | ||||||
| Patient B | Female | 27+1 | 800 g | Maternal preeclampsia and HELLP syndrome | RDS, PDA, PH, NEC | Death |
| Caesarean delivery | ||||||
| Patient C | Male | 25 | 700 g | Maternal preeclampsia and HELLP syndrome | RDS, PH, grade III IVH, hydrocephalus, NEC | Death |
| Caesarean delivery | ||||||
| Patient D | Male | 28+5 | 990 g | Twin pregnancy | Late-onset sepsis, mild BPD, grade II IVH | Discharge home |
| Caesarean delivery |
BPD, bronchopulmonary dysplasia; HELLP, haemolysis, elevated liver enzymes and low platelet; IVH, intraventricular haemorrhage; NEC, necrotising enterocolitis; PDA, patent ductus arteriosus; PH, pulmonary hypertension; RDS, respiratory distress syndrome.
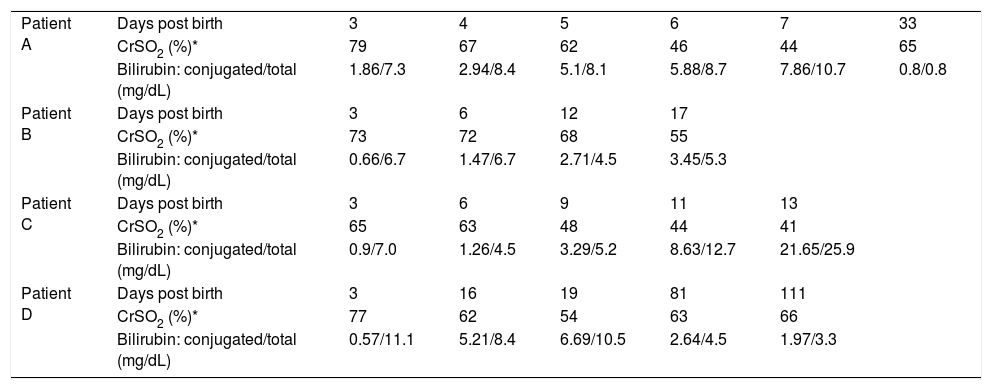
Temporal trends in bilirubin and cerebral rSO2.
| Patient A | Days post birth | 3 | 4 | 5 | 6 | 7 | 33 |
| CrSO2 (%)* | 79 | 67 | 62 | 46 | 44 | 65 | |
| Bilirubin: conjugated/total (mg/dL) | 1.86/7.3 | 2.94/8.4 | 5.1/8.1 | 5.88/8.7 | 7.86/10.7 | 0.8/0.8 | |
| Patient B | Days post birth | 3 | 6 | 12 | 17 | ||
| CrSO2 (%)* | 73 | 72 | 68 | 55 | |||
| Bilirubin: conjugated/total (mg/dL) | 0.66/6.7 | 1.47/6.7 | 2.71/4.5 | 3.45/5.3 | |||
| Patient C | Days post birth | 3 | 6 | 9 | 11 | 13 | |
| CrSO2 (%)* | 65 | 63 | 48 | 44 | 41 | ||
| Bilirubin: conjugated/total (mg/dL) | 0.9/7.0 | 1.26/4.5 | 3.29/5.2 | 8.63/12.7 | 21.65/25.9 | ||
| Patient D | Days post birth | 3 | 16 | 19 | 81 | 111 | |
| CrSO2 (%)* | 77 | 62 | 54 | 63 | 66 | ||
| Bilirubin: conjugated/total (mg/dL) | 0.57/11.1 | 5.21/8.4 | 6.69/10.5 | 2.64/4.5 | 1.97/3.3 |
CrSO2, cerebral regional oxygen saturation.
These 4 ELBW infants with multifactorial cholestatic hyperbilirubinaemia had rSO2 values indicative of risk of severe cerebral hypoxia, but after the common causes of altered cerebral NIRS monitoring values were ruled out, this finding was attributed to hyperbilirubinaemia.1 Although cerebral rSO2 decreases progressively in the first days of life in preterm infants, the values observed in our patients were below those reported in the literature and therefore were not completely explained by this pattern. In addition, in patients A and D, the rSO2 normalized as the hyperbilirubinaemia improved. To our knowledge, no evidence on this phenomenon has been published for the neonatal population, but studies in adults with liver disease have reported a negative correlation between the cerebral rSO2 and the serum bilirubin level.2,4 Furthermore, some authors found that NIRS was not at all reliable in patients with severe hyperbilirubinaemia during liver transplantation.3 The products of the degradation of the haem group are chromophores that absorb light in the near-infrared range (650-900 nm), but do not modify cerebral blood flow or oxygen uptake. Therefore, the interaction between bilirubin levels and rSO2 has been attributed to a competitive absorbtion of light by bilirubin and haemoglobin.2,4 There is solid evidence on the interference between haemoglobin and bilirubin in the measurement of bilirubin levels by transcutaneous or spectrophotometric methods in newborn infants, a problem that can be bypassed by the simultaneous measurement of several wavelengths. Interestingly, the use of NIRS in stool samples has been investigated as a means to detect biliary atresia in neonates.5 In patients with this condition, the absorbance peak at 730 nm attributed to conjugated bilirubin is absent, contrary to the samples of patients without biliary atresia. The evidence shows that the presence of meconium in the bowel, with its high concentration of conjugated bilirubin, interferes with abdominal NIRS monitoring using most of the devices currently available.6 For this reason, clinical trials are currently underway to test NIRS systems that include algorithms to compensate for the presence of meconium in the bowel. Monitors made by different manufacturers use different wavelengths, and therefore the interference of bilirubin may vary between systems, but this aspect has also not been studied to date.
It would be interesting to investigate whether unconjugated and conjugated bilirubin interfere with NIRS monitoring to the same extent, given the high incidence of indirect hyperbilirubinaemia in neonates.
In short, this case series suggests that hyperbilirubinemia may interfere with NIRS monitoring in VLBW infants. Large-scale, robust studies are required to corroborate these findings and to explore relevant questions, such as the role of indirect bilirubin in this interference and whether NIRS values are associated with the degree of hyperbilirubinaemia. Our findings warn of the limitations of NIRS in detecting changes during regional monitoring in this group of patients.
FundingThe study did not receive any form of funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Rodríguez MJ, Corredera A, Martínez-Orgado J, Arruza L. Interferencia entre NIRS cerebral y bilirrubina conjugada en neonatos de extremado bajo peso. Anales de Pediatría. 2021;95:371–373.