In children, infection by adenovirus is a frequent cause of self-limiting, mild to moderate febrile and/or respiratory illness, but in some instances it can cause severe disease followed by chronic sequelae. We present 3 cases of severe adenovirus infection that illustrate the broad clinical spectrum of this pathogen and the short- and long-term impact of the infection.
A boy aged 22 months with acute bronchitis of 2 day’s duration was transported to the emergency department in an ambulance due to hypoxaemia with an oxygen saturation (SaO2) of 87%, tachypnoea with 58 bpm, generalized retractions and bilateral expiratory wheezing. The patient experienced cardiac arrest requiring orotracheal intubation and mechanical ventilation in the intensive care unit for 8 days. Testing by polymerase chain reaction of a throat swab specimen turned out positive for adenovirus and respiratory syncytial virus. After extubation, inspiratory and expiratory rhonchi, bilateral coarse crackles and the need for oxygen therapy persisted for three weeks, prompting performance of a lung CT scan that revealed a bilateral mosaic attenuation pattern compatible with postinfectious bronchiolitis obliterans (PiBO1 (Fig. 1A). Treatment of PiBO was initiated with intravenous high-dose methylprednisolone, azithromycin, montelukast and acetylcysteine.2 As a complication, the patient developed tracheal stenosis of 60%–70% secondary to intubation, diagnosed by a chest TC scan and flexible bronchoscopy that allowed visualization of tracheal granuloma (Fig. 1B) and treated with repeated balloon dilations and nebulised budesonide, leaving residual stenosis of 20%–30% (Fig. 1C). The respiratory manifestations improved gradually, and the patient was discharged 60 days after admission without need of oxygen therapy. The outcome at 1 year is satisfactory, with no signs of respiratory distress, although the lung sounds continue to be abnormal with bilateral coarse crackles. The patient experiences acute episodes of infectious bronchitis that are managed with inhaled salbutamol and oral corticosteroids.
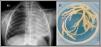
(A) Lung computed tomography scan: bilateral mosaic attenuation pattern compatible with bronchiolitis obliterans. (B) Flexible bronchoscopy: tracheal stenosis with reduction of 60% to 70% of the tracheal lumen due to granuloma. (C) Flexible bronchoscopy, 3 months after image B: residual membrane after steroid therapy and dilations.
A boy aged 3 years presented with increased work of breathing in the context of febrile acute bronchitis. The salient findings of the physical examination were increased work of breathing with generalized retractions, tachypnoea with 70 bmp, bilateral expiratory wheezing with hypoventilation in the left hemithorax and an SaO2 of 84%. The plain chest radiograph showed complete opacification of the left hemithorax with tracheal shift toward the involved lung and hyperinflation of the contralateral lung, all of which was compatible with complete atelectasis of the left lung (Fig. 2A). A few hours later, a flexible bronchoscopy examination revealed mucus plugging in the left main bronchus occluding the entire bronchial lumen. Aspiration achieved full clearance of the plugging, with removal of bronchial casts (Fig. 2B), and full re-expansion of the left lung with rapid improvement of the respiratory symptoms. Testing of a bronchoalveolar lavage sample detected adenovirus, confirming the diagnosis of plastic bronchitis secondary to adenovirus infection, an association that is rare in our region.3,4 The patient was then discharged, at which time the physical examination was normal, and has since experienced recurrent episodes of mild bronchitis.
A girl aged 2 years presented with malaise, vomiting and high fever of 4 days’ duration. The physical examination evinced poor general health, palpable hepatomegaly of 2–3 finger widths and a Glasgow score of 12–13 points. The blood glucose level as 26mg/dL with a ketone body concentration of 1.3mg/dL and metabolic acidosis with a lactate level of 11.7mmol/L. Further blood tests revealed an ammonia level of 528μmol/L, hypertransaminasaemia (gamma-glutamyl transferase 98 U/L; aspartate aminotransferase 16 658 U/L and alanine aminotransferase 7384 U/L), C-reactive protein level of 3.95mg/dL and severe coagulopathy with a prothrombin time percent activity of 9% and an international normalized ratio of 7.95. The abdominal ultrasound scan found hepatomegaly and gallbladder oedema. These findings, suggestive of acute liver failure, prompted transfer of the patient to a reference centre, where she underwent liver transplantation for management of fulminant hepatic failure. Adenovirus was detected in the bloodstream, leading to diagnosis of acute liver failure due to adenovirus infection in the context of an outbreak of severe acute hepatitis that affected 1010 children from 35 countries across the world in the first half of 2022 and associated with infection by serotype 41.5 During the post-transplantation follow-up, there has been no evidence of complications or acute transplant rejection. The patient remains in treatment with tacrolimus, which she tolerates well.
We consider that the cases presented are examples of the phenomenon known as “immunity debt”,6 which we have been experiencing since 2022 after the lifting of the restrictions imposed to fight SARS-CoV-2 and is characterised by an increase incidence and virulence of classical pathogens due to the reduction in herd immunity resulting from prolonged periods of decreased exposure, as was the case during the recent COVID-19 pandemic.