Self-prescribing or medicating ‘by proxy’ is not an autonomous, free and voluntary decision in the case of children. On the contrary, in this case it is based on the subjective interpretation of symptoms made by the mother or by a third person who is legally responsible for the minor. Analysing this situation is of great importance in order to know the determining factors, perceptions, and realities related to this problem.
MethodsOur proposal is to perform a prospective observational study for analysing maternal and familiar determinant factors related to self-prescribing and self-medicating ‘by proxy’ in paediatrics. A validated survey was developed to be applied to mothers of children aged 0–14 who are users of the Paediatric Emergency Department in a hospital.
ResultsA total of 1.714 mothers were recruited in a random period of time. This sample included 345 mothers who exclusively self-medicated their children (case group), and 1.369 mothers (control group) who did not meet this requirement. The overall percentage of medicating ‘by proxy’ was 32.8%. There is a significant association between self-medicating and educational level of the mother, the number of children, and the birth order among siblings. Neither maternal age nor social-occupational level are related to this problem. Most frequently used drugs include antipyretics and ‘anticatharrals’, usually administered as a monotherapy.
ConclusionsOur results seem to indicate that the educational level and the parental experience acquired with previous children could generate the required confidence in parents to choose the medication by themselves. Almost 85% of these drugs come from the ‘home first-aid kit’.
La autoprescripción o medicación «por poderes» en el niño no es una decisión autónoma, libre y voluntaria del paciente, sino que se fundamenta en la interpretación subjetiva que hace de los síntomas la madre o una tercera persona responsable del menor. Analizar esta situación nos parece de vital importancia, a fin de conocer condicionantes, percepciones y realidades relacionadas con esta problemática.
MétodosNos planteamos analizar mediante un estudio observacional prospectivo condicionantes maternos y familiares relacionados con la autoprescripción y medicación «por poderes» en pediatría. Desarrollamos una encuesta validada para madres de usuarios de 0–14 años de un Servicio de Urgencias pediátricas hospitalario.
ResultadosEn un periodo de tiempo aleatorio se selecciona a 1.714 madres, de las cuales 345 habían automedicado exclusivamente a sus hijos (grupo problema), las otras 1.369 (grupo control) no cumplían con el requisito anterior. La prevalencia total de medicación «por poderes» fue del 32.8%. Hay unaasociación significativa entre la automedicación y el nivel de estudios maternos, el número de hijos, el orden que ocupa entre los hermanos. Ni la edad materna, ni el nivel sociolaboral de la familia se relacionan con el problema. Los fármacos utilizados con más frecuencia incluyen antitérmicos y «anticatarrales», habitualmente como monoterapia.
ConclusionesNuestros resultados parecen indicar que el nivel educativo, y la experiencia adquirida por las madres con hijos previos, les genera la confianza suficiente para elegir los fármacos, que casi en el 85% de los casos proceden del «botiquín doméstico».
From certain perspectives, self-medication could be considered a positive self-care measure, as it can expedite the care for mild illnesses.1–4 However, when done irresponsibly, that is, when it turns into self-prescription,5,6 there can be potential adverse effects whose consequences may be hard to predict. The World Medical Association7 established a simple distinction between self-medication (use of medicines that do not require a physician's prescription) and self-prescription (self-determined use of medicines that require a physician's prescription due to their indications or risks); however, the boundaries between the two concepts may not be well understood by the general population.8
In children, there are unique factors at play in both self-prescription and self-medication that carry a higher risk compared to their practice in adults. On one hand, we do not know the actual effects on children of many drugs used in adults that have not been authorised for paediatric use.9,10 At present, there are several conditions limiting the use of medicines in children: not recommended, authorised with restrictions, not specified, use for unauthorised indications, or off-label use.11–15 On the other hand, and perhaps this may be the most particular aspect, it could be said that in children, both self-prescription and self-medication are carried out “by proxy,” that is, the decision is made by a third party, usually the mother, in the absence of any type of professional prescription. In children, this is not a self-directed, free and voluntary decision on the part of the patient based on the patient's knowledge or perceived symptoms, as it is in adults,16 but is based on the subjective interpretation of the symptoms by the mother or a third party in charge of the minor. Thus, we think that exploring this phenomenon is of vital importance in order to learn the factors and perceptions associated with this issue, which may not correspond to reality.
Materials and methodsWe conducted a prospective observational study on the population of paediatric patients in the catchment area of the Hospital Universitario San Cecilio de Granada that sought care in the outpatient emergency department. We recruited patients seeking care in dates selected at random after informing the parents or legal guardians about the study and obtaining their consent for participation. We provided the parents with a questionnaire that was designed, validated, corrected and approved by the competent Ethics Committee (Table 1).
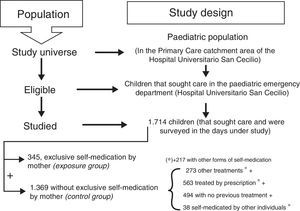
We recruited patients on days selected at random with a seasonal chronogram during the 2010–2011period. For the purposes of analysis, we classified patients into two groups: the exposure group, consisting of the children that had been exclusively self-medicated by the mother prior to visiting the emergency department, and the control group, consisting of children that did not fulfil this criterion. Fig. 1 represents the study design.
We entered the data on an electronic database, validated and analysed them with the Epi Info software version 3.4.3 for Windows. We guaranteed the confidentiality of the data in writing. We conducted a descriptive analysis of quantitative variables by calculating proportions and comparing them with the chi square test. We analysed qualitative variables by calculating odds ratios (ORs) with a confidence interval (CI) of 95%.
ResultsWe recruited 1.714 children, of who 345 (20.1%) were exclusively self-medicated by the mother. Of the 1.369 remaining children, 494 had received no medication, 273 were taking medication prescribed for a different illness, 564 were receiving prescribed medication for the current illness, and 38 were self-medicated by someone other than the mother. Of these 1.369 patients, 217 had also been self-medicated. Out of all the patients under study, 70.3% were receiving some sort of medication at the time of the visit: the overall percentage of self-medicated patients was 32.8% (345+217 of the 1714 patients). Table 2 shows the association between self-medication and different social and familial factors in our study.
Association between the frequency of self-medication and various factors.
| Factor | OR (95% CI) |
|---|---|
| Number of children (reference group: 1 child) | |
| 2 children | 2.47 (1.82–3.37) |
| 3 or more children | 3.14 (2.21–4.44) |
| Sibling order (reference group: first child) | |
| Second child | 1.83 (1.38–2.44) |
| Third or more | 2.32 (1.69–3.20) |
| Patient age (years) (reference group: 3–6 years) | |
| 0–2 | 0.90 (0.66–1.23)a |
| 7–10 | 1.47 (1.10–1.97) |
| 11–14 | 2.12 (1.28–3.49) |
| >14 | 3.51 (1.51–8.16) |
| Duration of symptoms prior to emergency department visit (hours) (reference group: <6h) | |
| 6–12 | 4.60 (3.20–6.62) |
| 12–24 | 6.32 (4.31–9.27) |
| 24–48 | 12.16 (7.83–18.86) |
| >48 | 25.77 (14.30–46.33) |
| Maternal educational attainmentb(reference group: primary/ESO) | |
| Intermediate | 1.41 (1.05–1.91) |
| Higher | 1.62 (1.22–2.14) |
| Maternal age (years) (reference group: <20 years) | |
| 21–30 | 1.36 (0.49–4.08)a |
| 31–40 | 1.39 (0.50–4.18)a |
| >40 | 2.01 (0.66–6.49)a |
| Family socioeconomic statusb(reference group: low) | |
| Middle | 1.18 (0.8–1.56)a |
| High | 1.23 (0.92–1.65)a |
CI, confidence interval; ESO, Spanish compulsory secondary education; OR, odds ratio.
The individual that decided on the use of medication was most frequently the mother (90.1%) with a significant difference (P<.01) compared to all other situations: grandmother or hired caregiver (4.2%), father (2.6%), patient/itself (1.8%) or pharmacist (1.3%).
We did not find a significant association between maternal age and the frequency of self-medication of children, taking mothers aged less than 20 years as reference: mothers aged 21–30 years (OR, 1.36; 95% CI, 0.49–4.08), mothers aged 31–40 years (OR, 1.39; 95% CI, 0.50–4.18), mothers aged 40 years (OR, 2.01; 95% CI, 0.66–6.49).
Maternal educational attainment (We designed a three-level scale for the study that summarised the scale used in the National Health Survey [Encuesta Nacional de Salud, ENS])28 was categorised as basic (primary-compulsory secondary education [ESO]), with 54.7% of mothers; intermediate, with 20.9% of mothers, and higher, with 24.4% of mothers. We found statistically significant differences between groups (P<.05 to P<.01) that were also significantly associated with the frequency of self-medication, which increased with higher educational attainment. For the intermediate educational attainment group, the OR was 1.41 (95% CI, 1.05–1.91) and for the higher educational attainment group, it was 1.62 (95% CI, 1.22–2.14).
We did not find a significant association between the socioeconomic level of the family (assessed with a method similar to the one used for educational attainment) and the frequency of self-medication: low (OR, 1 [reference]), middle (OR, 1.18; 95% CI, 0.89–1.56) and high (OR, 1.23; 95% CI, 0.92–1.65).
As for the number of children in the family, there was a predominance of families with one or two children (38.1 and 41.3%), with statistically significant differences (P<.01) between each of these and families with three or more children (20.6%). The frequency of self-medication was significantly associated with the number of children: it was more frequent in families with more children, with an OR of 3.14 for families with more than three children (95% CI, 2.21–4.44).
The frequency of self-medication was also significantly associated with the sibling order of the patient: it was greater the higher the sibling order. This criterion was distributed in the sample with a predominance of first-born children (56.2%) with a significant difference compared to the other groups (P<.01). Self-medication in second-born children corresponded to an OR of 1.83 (95% CI, 1.38–2.44), and for third and subsequent children, to an OR of 2.32 (95% CI, 1.69–3.20).
The frequency of self-medication was directly correlated to the age of patients, although this association was only significant starting at age 6 years. In our study, 1.8% of patients self-medicated without parental involvement; most of them were adolescents, mainly females, and nearly always due to treat menstruation symptoms.
The analysis of the duration of symptoms prior to seeking care found that it was of less than 6h in 45.3%, 6–12h in 25.6%, and that the frequencies declined for other durations. We found statistically significant differences (P<.01) between all duration groups, and also a significant association between duration of symptoms and self-medication frequency. Self-medication was more frequent with increasing duration of symptoms prior to seeking care: the OR for a duration of 6–12h was 4.60 (95% CI, 3.20–6.62), and for durations of more than 24h, it was 12.16 (95% CI, 7.83–18.86).
The type of medication used was consistent with the reason for seeking care. Antipyretic drugs (56.8%), cough medicine and mucolytic agents (40.3%) predominated over all other types (P<.01), which included oral rehydration solutions (6.1%), bronchodilators (5.5%), topical agents (4.6%) and others (22.8%). Eighteen percent of patients were taking antibiotics. Of all self-medicated patients, 62.6% were taking a single drug, 27.8% two drugs, and 9.6% three or more drugs.
As for the source of the medicines used, the majority were left over from the treatment of previous illnesses (84.9%), with medicines obtained specifically to treat the current episode amounting to only 11.9% and medicines of a different source to 3.2%. The choice of medication was based on a previous prescription for another child (49%), a previous prescription for the same child (44%) and a recommendation from outside the healthcare field (7%).
DiscussionThe issue of self-medication is an infrequent subject matter in the paediatric medical literature, while it is addressed more commonly in the adult and family medicine literature.17–19 Many studies have been designed to assess the use of medication,11–15,20–25 but few have provided evidence on aspects as specific as the association between the mother's and the family's role and self-medication.
The percentage of patients that were receiving medication (70.3%) and of patients that were self-medicated (32.8%) in our study were consistent with those published by other authors.20 There is wide variability owing to cultural influences and factors related to health care and social welfare. A rate of self-medication of 34% has been reported in Spain,20 which rose to 63% when narrowed down to the use of antipyretics in particular.23 The percentage reported in Italy is 28%,26 and in rural areas in Mexico, 58%.24
In our sample, the individual that decided on self-medication was the mother in 90% of the patients, similar to the 85.1% reported by other authors.24 Consultation with a pharmacist is rare, with a reported frequency in Spain of approximately 1%,20 which was consistent with our findings. Higher frequencies have also been described, although they have been questioned by the very authors that reported them.27
The association found between the number of children and the frequency of self-medication could be attributed to the experience acquired by the mother with previous children: as they grow in years, they feel “qualified” to treat symptoms already observed in previous children. This hypothesis seemed even more plausible when we found that the frequency of self-medication increased with the patient's sibling order.
Our data show that maternal educational attainment is associated with the frequency of self-medication, which was greater in mothers with intermediate and higher education compared to mothers with basic education. When we analysed data obtained from the ENS, we found that adult women use emergency services less frequently when they have a higher education (OR, 0.89; 95% CI, 0.81–0.97).28
Some authors20,28 have reported that children aged less than 4 or 5 years are the most medicated patients; this does not necessarily contradict our results, which show that medication “by proxy” is less frequent in children aged less than 2 years, a finding that could be explained by the greater vulnerability perceived by mothers in younger children, which would motivate mothers to medicate them by prescription as opposed to self-medication.
We did not find data in the literature regarding the association between duration of symptoms and the frequency of self-medication. The analysis of our data suggests that medication “by proxy” may delay seeking medical care, which could result in the need for emergency services in cases in which the problem is not resolved with self-medication.
The higher frequency of visits within 6h from the onset of symptoms found in our data (45.3%) was corroborated by the figure we obtained by analysing the data from the ENS28 for patients aged 0–14 years: patients sought care most frequently within 6h starting at age 5 years.
We also did not find any references in the literature on the frequency of the use of combined drugs in medication “by proxy.” A study of 336 children that visited the emergency department already medicated with one, two or three or more drugs found that fewer patients had received two or more drugs compared to only one.20 These results are similar to those of our study when considering self-medicated patients alone.
The “home medicine cabinet”, understood as the collection of medications kept at home, most of which are left over from previous treatments,29 is a tradition in our health culture, and although its prevalence is variable,40,19,29 we found it to be the main source of the medicines being used. The source of these medicines is frequently a prescription made for a past treatment, and less frequently its isolated purchase, as most can be obtained over the counter.
Antibiotics deserve special attention, as they are prescription medicines of which at least one container is found in 37% of Spanish households. In 85% of these households, the antibiotics had been prescribed by a physician, even though only 30% had a member that was being treated with antibiotics at the time they were surveyed.29,30 In our study, antibiotics accounted for 18% of self-prescribed medicines. Previous studies have found that 24% of mothers self-prescribe antibiotics for their children and that 21% save leftover antibiotics for future use,31,32 which may result in the use of antibiotics that are expired or at ineffective doses.
Using the data provided by the ENS,28 we analysed which pharmaceuticals had been consumed in the past two weeks by patients aged 0–14 years, and found that 11% had taken antibiotics, of which 98% had been obtained by prescription. It is very likely that courses of treatment in which the actual dosage and duration were lower than those prescribed also contributed to medicine stockpiles.
There is evidence of an association between maternal self-medication and more frequent self-medication of children.33 Our findings seem to confirm that the education mothers gain in the identification of symptoms through their experience with previous children allows them to acquire certain “competences” to indicate the administration of a medicine that they usually consider most appropriate on account of past prescriptions made by physicians for illnesses mothers consider to be similar. This hypothesis also fits with the source of the medicines used for self-medication, as 84.9% are left overs from previous treatments.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Valenzuela Ortiz M, Sánchez Ruiz-Cabello FJ, Uberos J, Checa Ros AF, Valenzuela Ortiz C, Augustín Morales MC, et al. Automedicación, autoprescripción y medicación «por poderes» en pediatría. An Pediatr (Barc). 2017;86:264–269.