Malnutrition on admission is closely related to a longer hospital stay and a higher morbidity. The prevalence of hospital malnutrition has been reported as almost as high as 50%, with 6% being the lowest. DHOSPE study investigates nutrition status in Spanish hospitals and its outcome during the hospital stay.
Patients and methodsA longitudinal, multicentre, descriptive, cross-sectional study, with a short follow-up period was conducted in 32 hospitals during 2011. A total of 991 patients were included, with ages from 0 to 17 years. Each patient was measured at admission (weight, length, weight for length -W/L-, length for age -L/A-), and at 7 and 14 days. The STAMP nutritional screening tool was completed on admission. Anthropometric measurements were reported as z-score, and nutrition status classified according to W/L and L/A for acute and chronic malnutrition, respectively.
ResultsThe prevalence of malnutrition was 7.1% for moderate, and 0.7% for severe acute malnutrition. For chronic malnutrition, 2.7% was moderate, and 1.4% severe. There were significant differences according to the underlying condition but not according to age. Results of STAMP show that around 75% of patients had a moderate to high risk of malnutrition. Nutritional status changed during admission for weight, as well as W/L and L/A. A worse nutritional status at admission and a higher STAMP score were positively correlated with the need for nutrition support.
ConclusionsThe prevalence of undernutrition was slightly lower (<8%) than previously reported, probably in relation to the variety of hospitals in the survey. Nevertheless, nutritional risk when evaluated with STAMP showed a high risk of malnutrition.
La desnutrición al ingreso se relaciona con hospitalizaciones más prolongadas y mayor morbilidad. La prevalencia varía entre un 6 y un 50%. El estudio DHOSPE se pregunta sobre la situación nutricional al ingreso y cómo se modifica durante el mismo.
Pacientes y métodosEstudio observacional, descriptivo, transversal, con un breve seguimiento longitudinal, multicéntrico, realizado en 32 hospitales en 2011. Se incluyó a 991 pacientes. En todos se realizó una valoración nutricional al ingreso, a los 7 y 14 días. Se utilizó la herramienta de cribado nutricional STAMP en el momento del ingreso. Las medidas antropométricas se evaluaron como puntuaciones Z y el estado nutricional con los índices de Waterlow de peso para la desnutrición aguda y de talla para la crónica.
ResultadosLa prevalencia de desnutrición fue del 7,1% para la aguda moderada y del 0,7% para la grave. Para la crónica: 2,7% moderada y 1,4% grave. No se encontraron diferencias significativas en función de la edad pero sí en función de la enfermedad. Algo más del 75% de los pacientes presentaban riesgo intermedio o elevado de desnutrirse durante el ingreso, valorado con STAMP. La peor situación nutricional al ingreso y una puntuación más elevada en el riesgo nutricional se correlacionaron positivamente con la necesidad de soporte nutricional.
ConclusionesLa prevalencia de desnutrición fue sensiblemente inferior (< 8%) a lo publicado, probablemente en relación con la distinta complejidad de los hospitales. El riesgo nutricional valorado con la herramienta STAMP fue elevado (el 75% presentaba riesgo moderado o intenso de desnutrición).
The European Society for Clinical Nutrition and Metabolism (ESPEN) defines malnutrition as “a state of nutrition in which a deficiency or excess of energy, protein, and other nutrients causes measurable adverse effects on tissue/body form and function, and clinical outcome.”1 Although this definition also refers to malnutrition due to excess intake (overweight and obesity), in the context of hospitalised patients, malnutrition due to insufficient intake, known as undernutrition, is more relevant. More recently, there have been advances on the classification of malnutrition as illness-related or not, which has implications for both the approach to its management and the response to the interventions used to prevent or treat it.2
The prevalence of acute and chronic undernutrition in hospitalised children depends to a great extent on the criteria used to define them and the growth references used in their assessment.3 The prevalence reported in studies published in different European countries or the United States ranges between 6% and a little less than 50%.4 On the other hand, it is well known that nutritional status worsens during the hospital stay in a variable percentage of patients.
The Undernutrition in Children's Hospitals in Spain study (Desnutrición en Hospitales Pediátricos en España [DHOSPE]) is a multicentric study conducted simultaneously in 32 hospitals and designed to answer two questions: which is the nutritional status of children at admission, and how does it change during their hospital stay? To these questions, we added the Screening Tool for the Assessment of Malnutrition in Pediatrics (STAMP). More detailed information on the design of the study and the prevalence of undernutrition and the risk of undernutrition at admission can be found in a previously published article,5 while in this one we will focus on the changes in nutritional status throughout the hospital stay and its correlation with the need for nutritional support.
Patients, materials and methodsWe conducted a multicentric, observational, descriptive, cross-sectional cohort study with a brief longitudinal followup, performed under conditions of everyday clinical practise (with no targeted intervention based on the results of the assessment at the time of admission). The study was conducted in 32 hospitals between June and September of 2011 (Appendix A details the participating hospitals). We included patients aged less than 17 years with a length of stay of more than 48h and whose parents or legal guardians signed their informed consent for participation in the study. We excluded patients admitted to the neonatal or intensive care units, or patients with medical conditions that would complicate the interpretation of the anthropometric data based on the judgment of the researcher, such as perinatal static encephalopathy, chromosome disorder, etc.
We grouped patients into the following age categories: infants (n=235, 23.7%), young children (1–3 years, n=212; 21.4%); age 3–8 years (n=286; 28.9%) and age more than 8 years (n=258; 26%); 54.3% were male.
The patients included in the study underwent a nutritional assessment in the first 72h of admission and later on at seven (V2) and at 14 days if they remained hospitalised or otherwise at discharge (V3). We collected the results of laboratory parameters (complete blood count, blood chemistry panel) when applicable. Furthermore, we administered the STAMP questionnaire during the initial evaluation to assess for nutritional risk. The STAMP tool consists of five simple steps: steps 1 through 3 rate elements associated with dietary intake and anthropometric measurements; step 4 combines the three scores and establishes a risk category (from 0 to >4), and step 5 proposes a treatment plan6 (available at http://stampscreeningtool.org/stamp.html, accessed March 27, 2015). We only applied the first four steps.
We also documented the type of nutritional support that patients received during their stay (without specific indications, use of enteral tube feeding and use of parenteral nutrition) and assessed its correlation with nutritional status at admission and the evaluation of nutritional risk (STAMP).
The study protocol was approved by the Clinical Research Ethics Committees of all participating hospitals. We obtained the informed consent of the parents or legal guardians as well as the consent of patients aged more than 12 years.
Statistical methodsWe assumed a prevalence of undernutrition in the sample of 25% based on the evidence from previous studies.3,4 We estimated that 801 participants were required for an error in the estimation of the prevalence of ±3% and a 95% confidence interval. Considering that we could had losses of up to 15%, we established that we needed a final sample of 1000 children. Using the STAMP questionnaire, we classified diseases into three categories: low or zero probability, high probability, or certain or near-certain probability of malnutrition.
We assessed anthropometric measurements (weight, height, body mass index) in z-scores, and using the Fundación Orbegozo growth charts of 1988 as reference.7 We determined the nutritional status of patients using the percentage of weight-for-height (Waterlow-weight) as a measure of acute undernutrition (>100%, overweight-obesity; 90–100%, normal weight; 80–90%, mild undernutrition; 70–80%, moderate undernutrition; <70%, severe undernutrition) and the percentage of height-for age (Waterlow-height) as a measure of chronic undernutrition (>95%, normal; 90–95% mild undernutrition; 85–90%, moderate undernutrition; <85%, severe undernutrition).
We performed the statistical analysis with Statistical Analysis Software (SAS) version 9.3. We compared the means or medians of independent groups by means of parametric ANOVA for normally distributed variables and nonparametric ANOVA for variables that did not follow a normal distribution. We used the chi square test or the Cochran-Mantel-Haenszel test to compare proportions in independent groups. For repeated measures, we used ANOVA to compare central tendency and Friedman's test to compare proportions.
ResultsThe data on the prevalence of malnutrition have been published in a previous article5: in short, out of the 991 patients in the final analysis we found moderate acute malnutrition in 7.1% and acute severe malnutrition in 0.7%, while 37.9% of the children admitted to hospital were overweight or obese. We found chronic moderate malnutrition in 2.7% and chronic severe malnutrition in 1.4%. We found no significant differences between age groups, although there were differences between patients with different diseases. Thus, the weight z-score was significantly lower in the group of patients with diseases categorized as “with certain probability of malnutrition” in all age groups except the group aged more than 8 years. We did not find an association between serum albumin levels and nutritional status at admission.
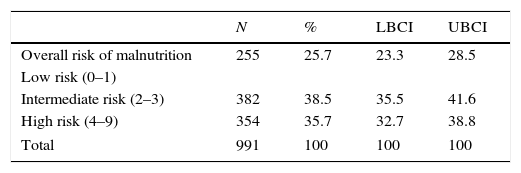
Table 1 shows the results of the STAMP questionnaire at admission. The percentage of patients with intermediate or high risk of having undernutrition during the hospital stay was 76.6% for the group aged less than 1 year, 75.4% for the group aged 1–3 years; 70.3% for the group aged 3–8 years 75.6% for the group aged more than 8 years, with no significant differences between groups. We observed higher nutritional risk scores in patients that had moderate acute malnutrition at admission.
Risk of malnutrition at admission based on the STAMP tool.
| N | % | LBCI | UBCI | |
|---|---|---|---|---|
| Overall risk of malnutrition | 255 | 25.7 | 23.3 | 28.5 |
| Low risk (0–1) | ||||
| Intermediate risk (2–3) | 382 | 38.5 | 35.5 | 41.6 |
| High risk (4–9) | 354 | 35.7 | 32.7 | 38.8 |
| Total | 991 | 100 | 100 | 100 |
Mean and 95% confidence interval.
LBCI, lower bound of confidence interval; UBCI, upper bound of confidence interval.
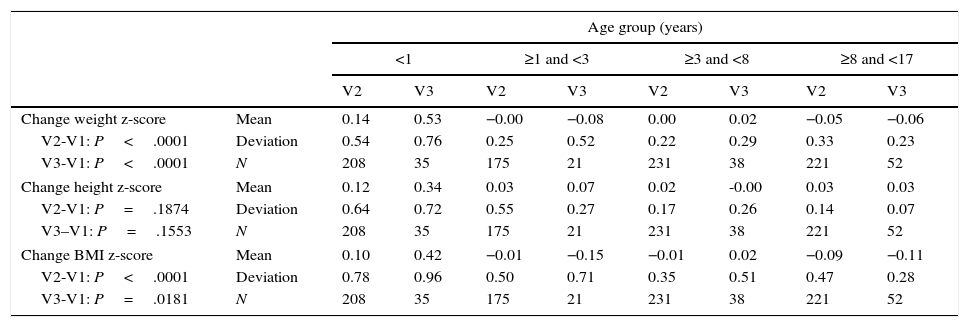
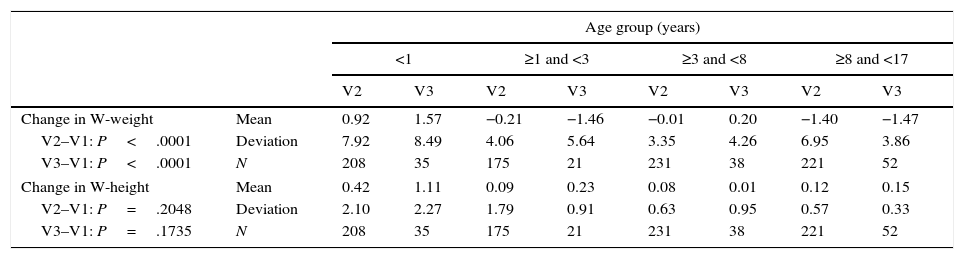
An additional nutritional assessment was performed one week after admission in 835 patients, and a third one at two weeks from admission or at discharge in 146 patients. We found significant differences in the changes in weight z-score from baseline both in V2 and V3, but not in height (Table 2), as well as in the Waterloo weight-for-height (Table 3), although with an uneven trend across age groups. Thus, it improved in infants and the 3-to-8 years age group, but it worsened in children aged 1–3 years and hardly changed in the group of children aged more than 8 years. Although weight-for-height did not change during the hospital stay in 73–87% of patients, nutritional status improved in approximately 17.3% (in infants) and 2.7% (children aged more than 8 years), while nutritional status worsened in 10% of patients in all age groups.
Assessment of the change in z-score in the measurements at one week (V2) and 2 weeks (V3), by age group.
| Age group (years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| <1 | ≥1 and <3 | ≥3 and <8 | ≥8 and <17 | ||||||
| V2 | V3 | V2 | V3 | V2 | V3 | V2 | V3 | ||
| Change weight z-score | Mean | 0.14 | 0.53 | −0.00 | −0.08 | 0.00 | 0.02 | −0.05 | −0.06 |
| V2-V1: P<.0001 | Deviation | 0.54 | 0.76 | 0.25 | 0.52 | 0.22 | 0.29 | 0.33 | 0.23 |
| V3-V1: P<.0001 | N | 208 | 35 | 175 | 21 | 231 | 38 | 221 | 52 |
| Change height z-score | Mean | 0.12 | 0.34 | 0.03 | 0.07 | 0.02 | -0.00 | 0.03 | 0.03 |
| V2-V1: P=.1874 | Deviation | 0.64 | 0.72 | 0.55 | 0.27 | 0.17 | 0.26 | 0.14 | 0.07 |
| V3–V1: P=.1553 | N | 208 | 35 | 175 | 21 | 231 | 38 | 221 | 52 |
| Change BMI z-score | Mean | 0.10 | 0.42 | −0.01 | −0.15 | −0.01 | 0.02 | −0.09 | −0.11 |
| V2-V1: P<.0001 | Deviation | 0.78 | 0.96 | 0.50 | 0.71 | 0.35 | 0.51 | 0.47 | 0.28 |
| V3-V1: P=.0181 | N | 208 | 35 | 175 | 21 | 231 | 38 | 221 | 52 |
P-value obtained in nonparametric ANOVA, as variables did not have a normal distribution.
Assessment of weight-for-height (W-weight) and height-for-age (W-height) at one week (V2) and two weeks (V3) compared to baseline, by age group.
| Age group (years) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| <1 | ≥1 and <3 | ≥3 and <8 | ≥8 and <17 | ||||||
| V2 | V3 | V2 | V3 | V2 | V3 | V2 | V3 | ||
| Change in W-weight | Mean | 0.92 | 1.57 | −0.21 | −1.46 | −0.01 | 0.20 | −1.40 | −1.47 |
| V2–V1: P<.0001 | Deviation | 7.92 | 8.49 | 4.06 | 5.64 | 3.35 | 4.26 | 6.95 | 3.86 |
| V3–V1: P<.0001 | N | 208 | 35 | 175 | 21 | 231 | 38 | 221 | 52 |
| Change in W-height | Mean | 0.42 | 1.11 | 0.09 | 0.23 | 0.08 | 0.01 | 0.12 | 0.15 |
| V2–V1: P=.2048 | Deviation | 2.10 | 2.27 | 1.79 | 0.91 | 0.63 | 0.95 | 0.57 | 0.33 |
| V3–V1: P=.1735 | N | 208 | 35 | 175 | 21 | 231 | 38 | 221 | 52 |
P-value obtained in nonparametric ANOVA, as variables did not have a normal distribution.
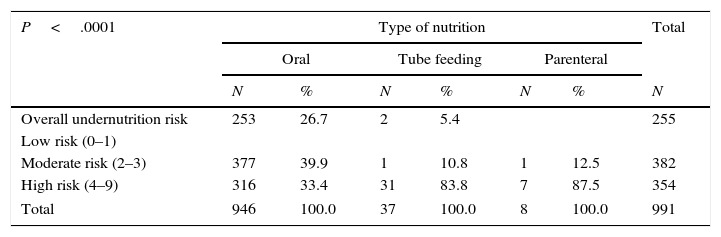
Nutritional status at admission was significantly correlated with the need for artificial nutrition (P=.03 for acute undernutrition and P<.0001 for chronic undernutrition) and with nutritional risk (Table 4).
Type of nutritional intervention based on the undernutrition risk score.
| P<.0001 | Type of nutrition | Total | |||||
|---|---|---|---|---|---|---|---|
| Oral | Tube feeding | Parenteral | |||||
| N | % | N | % | N | % | N | |
| Overall undernutrition risk | 253 | 26.7 | 2 | 5.4 | 255 | ||
| Low risk (0–1) | |||||||
| Moderate risk (2–3) | 377 | 39.9 | 1 | 10.8 | 1 | 12.5 | 382 |
| High risk (4–9) | 316 | 33.4 | 31 | 83.8 | 7 | 87.5 | 354 |
| Total | 946 | 100.0 | 37 | 100.0 | 8 | 100.0 | 991 |
P-value obtained using the Cochran-Mantel-Haenszel test (based on ranges), as the variable did not follow a normal distribution.
The prevalence of acute or chronic malnutrition in hospitalised pediatric patients varies widely based on the criteria applied for its definition and the growth charts that serve as the reference standard.3 This partly explains why the prevalence reported in published studies ranges between 6% and 40%. A national survey recently conducted in the Netherlands found that 19% of hospitalised children in this country had acute or chronic malnutrition.8 There is also the problem that a variable percentage of children become malnourished during their hospital stay, so that it would be convenient to identify not only the patients with undernutrition at the time of admission, but also those at risk of undernutrition during their hospital stay.4
The purpose of the DHOSPE study, promoted by the Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica, was to answer the questions already mentioned. A study conducted in a tertiary care hospital in Spain found a prevalence of undernutrition of 17%.9 However, the prevalence of acute undernutrition found by the DHOSPE study was of approximately 8%, and it was moderate in most patients. The most likely reason for this is that the latter included hospitals of every possible level of care, providing a more realistic representation of undernutrition at admission, with a lower prevalence compared to those reported in the classical references on the subject10,11 and closer to those reported by more recent studies by Pawelleck et al. (2008, prevalence of 6.4%),12 Huysentruyt et al. (2013, 9.8% of patients with acute undernutrition)13 or the multicentric European study (2015, 7.0%),14 and has the added strength of being a nationwide survey. These figures are considerably lower than those reported in the adult population,15,16 especially in the elderly.17 Unlike what has been reported in other series, we did not find a higher prevalence of undernutrition either in infants or in children with diseases with the potential to impact nutritional status.
The aforementioned European multicentric study16 found that the more severe the undernutrition at admission, the longer the hospital stay, an association that was not analyzed in the DHOSPE study. While 23% of the patients in the European study lost weight during their hospital stay, the percentage in our study was substantially lower (10%), although we were unable to quantify the weight loss. On the other hand, few children experienced improvements in nutritional status during their stay.
While the prevalence of undernutrition at admission may be low (<10%), there is the added concern that a similar percentage develops undernutrition during their hospital stay, so it could be beneficial to have screening tools for the risk of undernutrition that would allow the performance of preventive interventions in at-risk children. As we have already mentioned, undernutrition is not only associated with longer lengths of stay, but also with increased morbidity (nosocomial infections, complications of wound healing, etc.). In recent years, considerable efforts have been made toward developing nutritional screening tools for the pediatric population. At least five such tools have been published in the past decade,5,18–21 most frequently validated by their own authors,22 and rarely by other parties.23,24 Furthermore, there is no evidence on the impact in terms of costs and benefits of the potential implementation of these tools in clinical practice. Most of the tools are highly sensitive in detecting nutritional risk, but they have low specificity, as we were able to corroborate in using the STAMP tool at admission (based on which approximately three fourths of admitted children were at moderate to high risk of undernutrition). Its correlation with nutritional status at the time of admission was also weak. However, in the DHOSPE study we found a greater probability of requiring artificial nutritional support during the hospital stay in patients with unfavorable STAMP scores, which suggests that it may be useful in the practice of pediatrics nutritional support teams,25 although larger studies are required to corroborate this.
Some of the limitations of the study include its performance during a specific season of the year (summer) that may not be representative of the entire year, and that the criteria applied to define undernutrition (weight-for-height and height-for-age) may erroneously categorize some children as malnourished that are not. Although some interesting approaches to the definition of malnutrition have been proposed, such as the one by Mehta mentioned above or the ASPEN indicators,26 the task has yet to be completed, as is also the case for the adult population.27
However, the identification of malnutrition and the risk of undernutrition in hospitalised children, along with ensuring the visibility of the problem (for instance, by coding it among the diagnoses included in the discharge summary)28 are key elements to improve the approach and resolution of the problem.
FundingThis study was conducted with the support of the Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica with a grant from the Abbott Fund (area of nutrition).
Conflict of interestsThe authors have no conflicts of interest to declare.
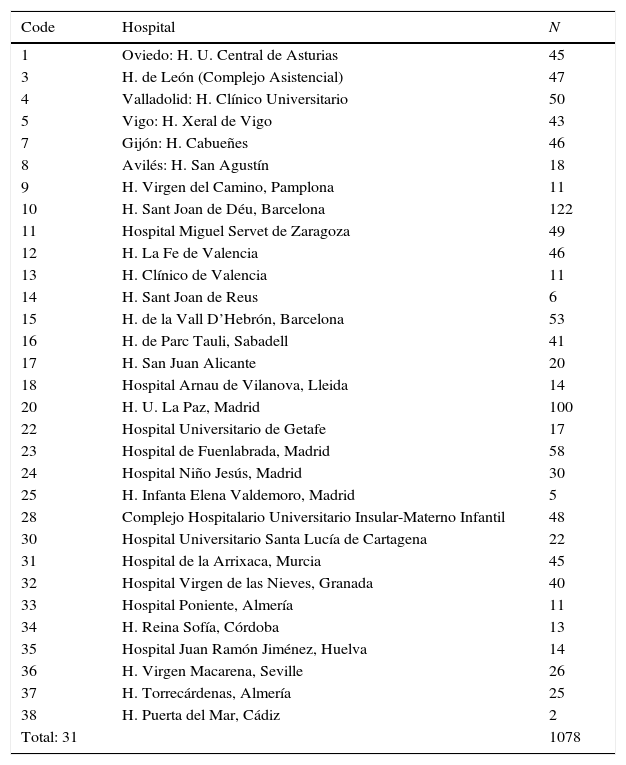
Number of patients included in the study by participating hospital.
| Code | Hospital | N |
|---|---|---|
| 1 | Oviedo: H. U. Central de Asturias | 45 |
| 3 | H. de León (Complejo Asistencial) | 47 |
| 4 | Valladolid: H. Clínico Universitario | 50 |
| 5 | Vigo: H. Xeral de Vigo | 43 |
| 7 | Gijón: H. Cabueñes | 46 |
| 8 | Avilés: H. San Agustín | 18 |
| 9 | H. Virgen del Camino, Pamplona | 11 |
| 10 | H. Sant Joan de Déu, Barcelona | 122 |
| 11 | Hospital Miguel Servet de Zaragoza | 49 |
| 12 | H. La Fe de Valencia | 46 |
| 13 | H. Clínico de Valencia | 11 |
| 14 | H. Sant Joan de Reus | 6 |
| 15 | H. de la Vall D’Hebrón, Barcelona | 53 |
| 16 | H. de Parc Tauli, Sabadell | 41 |
| 17 | H. San Juan Alicante | 20 |
| 18 | Hospital Arnau de Vilanova, Lleida | 14 |
| 20 | H. U. La Paz, Madrid | 100 |
| 22 | Hospital Universitario de Getafe | 17 |
| 23 | Hospital de Fuenlabrada, Madrid | 58 |
| 24 | Hospital Niño Jesús, Madrid | 30 |
| 25 | H. Infanta Elena Valdemoro, Madrid | 5 |
| 28 | Complejo Hospitalario Universitario Insular-Materno Infantil | 48 |
| 30 | Hospital Universitario Santa Lucía de Cartagena | 22 |
| 31 | Hospital de la Arrixaca, Murcia | 45 |
| 32 | Hospital Virgen de las Nieves, Granada | 40 |
| 33 | Hospital Poniente, Almería | 11 |
| 34 | H. Reina Sofía, Córdoba | 13 |
| 35 | Hospital Juan Ramón Jiménez, Huelva | 14 |
| 36 | H. Virgen Macarena, Seville | 26 |
| 37 | H. Torrecárdenas, Almería | 25 |
| 38 | H. Puerta del Mar, Cádiz | 2 |
| Total: 31 | 1078 |
H, hospital; H.U., University Hospital (Hospital Universitario).
Please cite this article as: Moreno Villares JM, Varea Calderónb V, Bousoño Garcíac C, On behalf of the Sociedad Española de Gastroenterología, Hepatología y Nutrición Pediátrica (SEGHNP). Malnutrición en el niño ingresado en un hospital. Resultados de una encuesta nacional. An Pediatr (Barc). 2017;86:270–276.