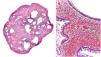
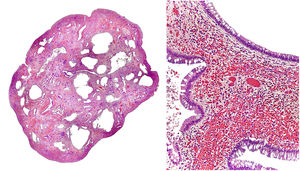
Intestinal juvenile polyps are benign lesions that constitute a frequent cause of rectal bleeding in childhood.1 We present the case of a 2-years-old girl with no history of interest who presented in the Pediatric Emergency Department on two occasions due to a prolapse of mucosal tissue through the rectum that resolved spontaneously (Fig. 1, left), leading to the diagnosis of recurrent rectal prolapse. At the same time, the patient was diagnosed of intestinal parasitic infection by Giardia lamblia and Dientamoeba fragilis and started targeted antiparasitic treatment. Weeks later, the patient spontaneously expelled a mucosal mass with an ulcerated base through the anus (Fig. 1, right) followed by an episode of self-limited rectal bleeding. The histological examination determined that the mass was a juvenile polyp without dysplasia (Fig. 2). The patient had a favourable outcome. Rectal juvenile polyps are frequent in childhood. Most of them are located in the left colon, although they may develop anywhere in the bowel. Although the most usual presentation is painless rectal bleeding (which may be severe),2 the prolapse of rectal polyps through the anus has been described previously in the paediatric population.3 Therefore, polyps must be contemplated in the differential diagnosis of rectal mucosal prolapse in paediatric patients.
Histological examination of the lesion (Haematoxylin & Eosin stain, microphotographs). Left (2×): transverse section of the polyp. Glandular dilatation accompanied by cystic spaces in the lamina propria. Right (10×): Glands lined by simple cuboidal epithelium with caliciform cells. Vascular congestion, lymphoplasmacytic infiltration and marked eosinophilia.
Before the submission of this article, we obtained the verbal and written informed consent from the legal guardians of the patient whose clinical photographs are included in this publication. We accessed the medical records of the patient according to current hospital regulations.
Conflicts of interestThe authors have no conflicts of interest to declare.