Skin infections are a common cause for dermatological consultations in the paediatric setting. A review is presented of the clinical manifestations, diagnosis and treatment of the main bacterial skin infections, as well as the diagnosis and treatment of super-infected puncture and bite wounds. The most prevalent bacteria in skin infections are Staphylococcus aureus and Streptococcus pyogenes. Treatment is usually empirical, since microbiological studies are only recommended under certain circumstances or lack of improvement with common therapies. Superficial skin infections can be treated with local antiseptics or antibiotics (mupirocin or fusidic acid). Systemic treatment is usually reserved for patients with extensive or severe disease or with other risk factors. Systemic treatment depends on the suspected infecting bacteria, with penicillin, amoxicillin, amoxicillin–clavulanic acid and first- or second-generation cephalosporin being the most frequently used drugs. Due to the low incidence of community-acquired methicillin-resistant infection by S. aureus in Spain, the use of clindamycin or co-trimoxazole is only recommended after severe disease, relapses or a clear epidemiological background.
Las infecciones cutáneas constituyen un motivo de consulta frecuente en dermatología pediátrica. Se revisan las manifestaciones clínicas, el diagnóstico y el tratamiento de los principales cuadros infecciosos bacterianos de la piel, así como de la sobreinfección de las heridas punzantes y por mordedura. Las bacterias más prevalentes en las infecciones cutáneas son Staphylococcus aureus (S. aureus) y Streptococcus pyogenes. El tratamiento es generalmente empírico y solo ante determinadas circunstancias o mala evolución clínica se recomienda el estudio microbiológico. Las infecciones cutáneas superficiales pueden tratarse con antisépticos y antibióticos tópicos (mupirocina o ácido fusídico). El tratamiento sistémico se reserva para formas extensas, graves o con otros factores de riesgo del huésped. En estos casos, el antibiótico de elección dependerá, entre otros factores, de los patógenos sospechados; los más utilizados son penicilina, amoxicilina, amoxicilina-ácido clavulánico y cefalosporinas de primera o segunda generación. Considerando la baja incidencia de S. aureus resistente a la meticilina de adquisición comunitaria en nuestro país, no se recomienda modificar el tratamiento empírico salvo en circunstancias de especial gravedad, recurrencia o antecedente epidemiológico, en cuyo caso el tratamiento recomendado es clindamicina o trimetoprima-sulfametoxazol.
The skin is the first barrier of the organism against external agents and skin infections, the most frequent reason for paediatric dermatology consultations. The main risk factors are deterioration of the integrity of the skin, poor hygiene, overcrowding, humidity and immunodeficiency.
The most prevalent bacteria are Staphylococcus aureus (S. aureus) and Streptococcus pyogenes (S. pyogenes). Both can cause skin infections by direct inoculation, haematogenous dissemination and through the production of toxins,1 as in Staphylococcal scalded skin syndrome by S. aureus and staphylococcus or streptococcus toxic shock syndrome.
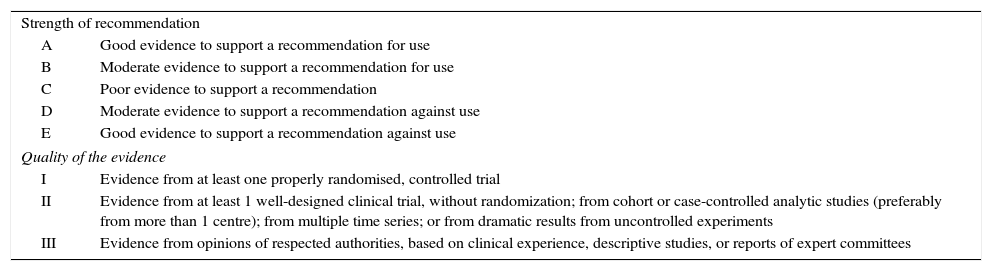
Based on the system of consensus documents, we will add the strength of the recommendation to our proposed measures, following the classification of the Infectious Diseases Society of America (Table 1).2
Strength of recommendation and quality of evidence.
| Strength of recommendation | |
| A | Good evidence to support a recommendation for use |
| B | Moderate evidence to support a recommendation for use |
| C | Poor evidence to support a recommendation |
| D | Moderate evidence to support a recommendation against use |
| E | Good evidence to support a recommendation against use |
| Quality of the evidence | |
| I | Evidence from at least one properly randomised, controlled trial |
| II | Evidence from at least 1 well-designed clinical trial, without randomization; from cohort or case-controlled analytic studies (preferably from more than 1 centre); from multiple time series; or from dramatic results from uncontrolled experiments |
| III | Evidence from opinions of respected authorities, based on clinical experience, descriptive studies, or reports of expert committees |
Taken from Khan et al.2
In general, the antibiotic treatment of skin infections is empirical.3 Blood or aspirate cultures, biopsies and swabs are only recommended under certain circumstances (chemotherapy, neutropoenia, serious immunodeficiency, immersion wounds, animal bites, infection of the general condition, suspicion of complications, extensive infection, suspicion of ecthyma gangrenosum, necrotising fasciitis, admitted patients) or in the event of poor response to treatment. Treatment should be based on clinical analysis, possible microorganism involved, site, extension and depth of the infection, and personal history.
Asymptomatic skin infections involving the superficial layers of the skin are usually treated with antiseptics or topical antibiotics; those with the best coverage against common pathogens are mupirocin ointment and fusidic acid cream or ointment. In infections by methicillin-sensitive S. aureus with poor response to mupirocin, retapamulin ointment is a valid alternative in patients aged over 9 months.4
Systemic antibiotic therapy is reserved for certain clinical forms (cellulitis), extensive forms, rapid progression or dissemination, serious cases or patients in generally poor condition (necrotising fasciitis), neonates, cellulitis-adenitis in patients under 3 months of age and in immunodepressed patients. Sometimes, incision and surgical drainage are essential.
If there is suspicion of S. aureus, the antibiotic of choice is cloxacilin, although its pharmacological characteristics (administration every 6h, low bioavailability and bad taste) make amoxicillin–clavulanic acid and first-generation cephalosporin (cefadroxil or cefalexin) a reasonable alternative. In the event of contraindication for β-lactams, the drugs of choice are clindamycin (only available in 150 and 300mg capsules in Spain) and trimethoprim-sulfamethoxazole.
If there is suspicion of S. pyogenes, the antibiotic of choice is penicillin or amoxicillin. In patients who are allergic to β-lactams, 16-atom macrolides can be used (josamycin or midecamicina), clindamycin or, in the event of non-anaphylactic reaction, first-generation cephalosporin.
In infections where both bacteria may be implicated, treatment with amoxicillin–clavulanic acid or a first-generation cephalosporin is indicated.
At the time of drafting this document, neither cefadroxil nor cefalexin, the only first-generation cephalosporin with oral presentation, are sold in Spain in suspension form, and only 500mg capsules are available. Under these circumstances, second-generation cephalosporin (cefuroxime, cefaclor), despite being slightly less active against gram-positive cocci than first-generation cephalosporin, is a valid alternative.
Main infectious conditionsImpetigoThe onset of impetigo may occur at any age and is transmitted by autoinoculation, direct contact, or contaminated objects. It produces non-scarring epidermal lesions, well delimited, usually in exposed areas. It may be bullous or non-bullous. In the non-bullous form, caused by S. pyogenes, S. aureus (alone or in co-infection) and, occasionally, by group C and G streptococci, the lesions evolve from macula to papules, vesicles and pustules, which finally form a thick meliceric crust. In the bullous form, caused by S. aureus exfoliative toxins, the lesions evolve to vesicles and then to blisters with yellow more or less turbid and even purulent fluid, and finally form a fine crust. The main complication is local dissemination (cellulitis, lymphadenitis) or even systemic complications (pneumonia, osteoarthritis, sepsis).
In non-complicated mild cases, topical disinfectants can be used, mupirocin or fusidic acid every 8h, or retapamulin every 12h, for 5–7 days. If the lesions are extensive or with systemic symptoms, oral antibiotic therapy with amoxicillin–clavulanic acid, a first- or second-generation cephalosporin, or cloxacilin is recommended.5
Perianal bacterial dermatitisPerianal bacterial dermatitis consists of an erythema around the anus caused by S. pyogenes or less frequently by S. aureus, alone or associated with S. pyogenes.6 Incidence peaks at 3–5 years of age, predominantly in males (70%), although prevalence is the same in both sexes if vulvovaginitis is included,8 which together with balanoposthitis constitute what is known as perineal disease.
It manifests as a non-elevated erythema, measuring 2–3cm, around the anus, with well-delimited edges, sometimes accompanied by pruritus, painful bowel movement, constipation, overflow incontinence, haematochezia and fissures.9 Boys may present with balanoposthitis and girls with vulvovaginitis with secretion and dysuria.10 There are usually no general symptoms, unlike cellulitis. In the acute phase (<6 weeks progression) the lesion is red, bright, humid and painful, and may present a whitish pseudo-membrane. Without treatment, lesions become chronic, with painful fissures, mucous secretion or psoriasis-like plates with yellowish periphery crust. When the cause is staphylococcus, there may be pustules and the erythema extends towards the adjacent skin.6
Patients or members of the household may have presented acute pharyngoamigdalitis or a skin infection7 in the previous 3 months or simultaneously with perianal dermatitis, or be pharyngeal or perianal carriers of S. pyogenes.7,8 Recurrence after treatment with penicillin or amoxicillin is frequent (up to 37%),11 especially if there are non-diagnosed cases in relatives.
It is believed that transmission is by contact, whether through autoinoculation (infection or pharyngeal or skin carrier) or interfamilial contagion, especially if bath water is shared10 or if a relative has presented acute pharingoamigdalitis or perianal dermatitis.7
Diagnosis is based on clinical analysis and confirmation is bacteriological. Samples from the perianal area must be gathered from all patients (A-II) and pharyngeal samples if there are symptoms (B-III), for a rapid antigen detection test for S. pyogenes (100% positive predictive value)7 or a culture. If the result of the test is negative, it is recommended to prepare a culture due to the possibility of false negatives or S. aureus as a cause of the condition (A-II). Potential cases in persons cohabiting with the patient should be investigated and a rapid diagnostic test or a culture for symptomatic patients (B-III) carried out, since this is a frequent cause of recurrences within the family.
Although good results have been reported with topical antibiotic therapy in monotherapy (B-II), the use of systemic antibiotics is recommended in all cases (A-II). If no rapid diagnostic test available or if it is positive, oral treatment with penicillin or amoxicillin for 10 days is recommended (B-II), which may be prolonged to 14–21 days based on clinical progress (C-III).10 If there is no response after one cycle of amoxicillin, or if the diagnostic test was negative, and while waiting for the result of the culture, amoxicillin–clavulanic acid may be used (C-III).
When choosing the initial antibiotic therapy, a familial history of streptococci or staphylococcus infection must be taken into consideration (C-II).
For recurrent infection cefuroxime is recommended11 for 7–10 days (C-II). The association of oral and topic treatment seems to decrease recurrences (A-II).6
Infections of hair follicles: folliculitis, furuncle and carbuncleThe aetiological agent of hair follicle infection is S. aureus, followed by gram-negative bacilli. Predisposing factors include obesity, diabetes, hyperhidrosis, immunosuppression and atopical dermatitis.
Clinically, patients present with lesions on hair-bearing sites on the face, neck, armpits or glutei, ranging from a papule-vesicle with a erythematosus base (folliculitis, which affects the superficial hair follicle), to tender erythematosus nodules (furuncle, extending to the deep dermis), to warm, tender, erythematous plaques (carbuncle, affecting the surrounding subcutaneous cellular tissue).
The diagnosis is clinical and a microbiological study is only recommended for lesions that are atypical or respond poorly to treatment.12
Treatment is initially topical with mupirocin or fusidic acid, and in recurrent or extensive forms not responding to topical treatment, a combination of amoxicillin–clavulanic acid, clindamycin, cefadroxil, cefalexin or cefuroxime. For furuncles and carbuncles, it is recommended to apply local heat and assess the possibility of making an incision and surgical drainage.
Acute bacterial lymphangitisThis is defined as the inflammation of the lymphatic vessels of the subcutaneous tissue. The organisms most frequently involved are S. pyogenes, S. aureus and Pasteurella multocida (P. multocida) (the latter after an animal bite). There is usually systemic involvement, even before the distal oedema and linear cord to regional nodes are evident.
Empirical treatment in mild to moderate forms is amoxicillin–clavulanic acid or a first- or second-generation cephalosporin.
ErysipelasThis is a superficial infection affecting the superior dermis, the subcutaneous cellular tissue and sometimes the lymphatic system, in most cases caused by S. pyogenes or streptococci of groups B, C or G.1,13–18
The triggering factors include abrasions, ulcers, intertriginous fungal infections of the feet, venous or lymphatic obstruction and chronic oedema. In neonates, the infection may originate in the umbilical cord and extend to the abdominal wall.
Onset is acute, characterised by an erythematosus plate with well-defined and slightly elevated edges. It is more frequent in lower limbs and face, and may be associated with regional lymphadenitis. There are usually general symptoms (fever, chills, discomfort), sometimes before cutaneous signs. Systemic complications are also possible (sepsis, streptococcal toxic-shock syndrome, endocarditis, etc.), although they are rare in otherwise healthy patients. When the infection is resolved it produces scaling and hyperpigmentation.
The diagnosis is clinical (A-II); haemocultures and cultures of skin biopsies or aspirates have a low yield.
Treatment consists of administration of oral penicillin or amoxicillin (A-III).1 Patients with lesions of more than 5cm or generally poor condition, infants and immunodepressed patients may require hospitalisation and parenteral treatment (A-II). The care of wounds and their predisposing factors are also important aspects of the treatment (A-II).
CellulitisThis is an acute infection affecting the dermis and subcutaneous cellular tissue. Predisposing factors include trauma, wounds and pre-existing infections. It appears as a warm, tender, poorly defined erythematous plaque, which sometimes causes phlyctena, petechial or local necrosis and may be accompanied by lymphadenitis and systemic symptoms.17
The main cause is S. aureus and S. pyogenes. Other less frequent microorganisms are Streptococcus agalactiae and gram-negative bacilli in neonates and enterobacteria in immunosuppressed patients.
Its location may provide an aetiological orientation: in the periauricular region and the sole of the foot with puncture wounds P. aeruginosa is more frequent, while in bites, P. multocida is common.
The diagnosis is clinical, but a microbiological study is recommended in the cases discussed in the section on general treatment. An ultrasound scan may be useful to differentiate cellulitis from non-fluctuant abscesses.
A systemic antibiotic treatment with good coverage against S. aureus and S. pyogenes must always be recommended. In mild cases and under strict surveillance, oral treatment with amoxicillin–clavulanic acid, cloxacilin, cefadroxil, cefalexin, cefuroxime or clindamycin may be considered.
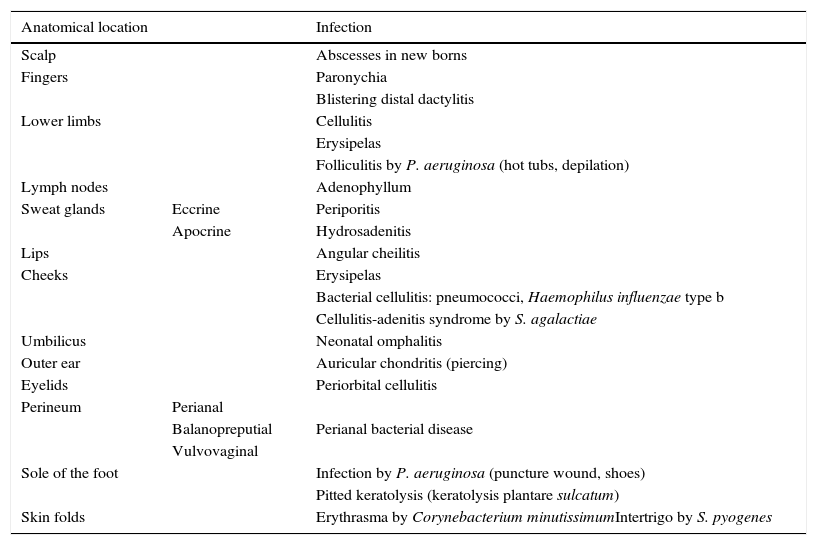
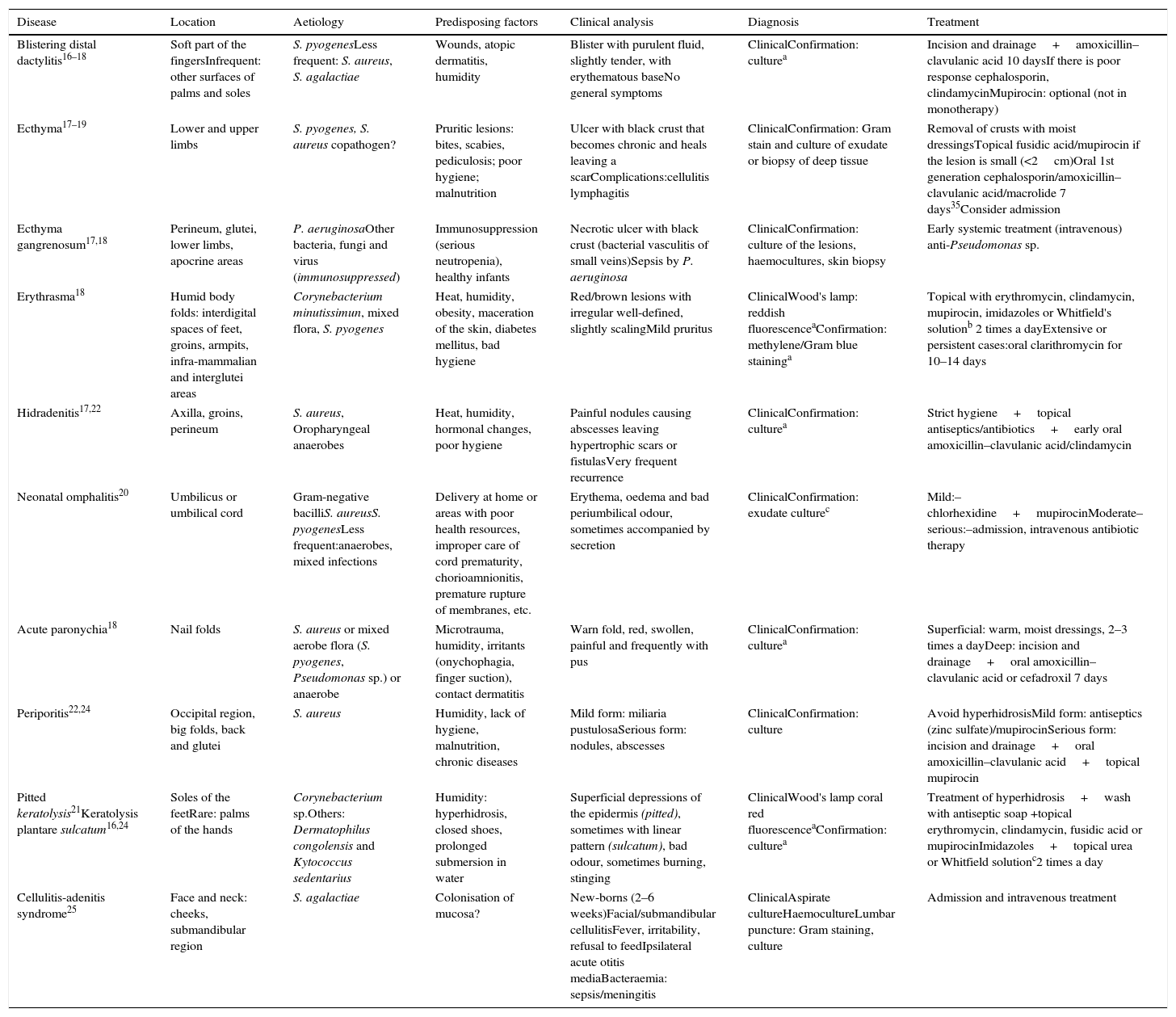
Tables 2 and 3 summarise of other infectious conditions of clinical relevance, and Table 4 details the recommended dosage of the most widely used anti-infective drugs.
Clinical forms of most frequent bacterial skin infections according to their location of preference.
| Anatomical location | Infection | |
|---|---|---|
| Scalp | Abscesses in new borns | |
| Fingers | Paronychia | |
| Blistering distal dactylitis | ||
| Lower limbs | Cellulitis | |
| Erysipelas | ||
| Folliculitis by P. aeruginosa (hot tubs, depilation) | ||
| Lymph nodes | Adenophyllum | |
| Sweat glands | Eccrine | Periporitis |
| Apocrine | Hydrosadenitis | |
| Lips | Angular cheilitis | |
| Cheeks | Erysipelas | |
| Bacterial cellulitis: pneumococci, Haemophilus influenzae type b | ||
| Cellulitis-adenitis syndrome by S. agalactiae | ||
| Umbilicus | Neonatal omphalitis | |
| Outer ear | Auricular chondritis (piercing) | |
| Eyelids | Periorbital cellulitis | |
| Perineum | Perianal | |
| Balanopreputial | Perianal bacterial disease | |
| Vulvovaginal | ||
| Sole of the foot | Infection by P. aeruginosa (puncture wound, shoes) | |
| Pitted keratolysis (keratolysis plantare sulcatum) | ||
| Skin folds | Erythrasma by Corynebacterium minutissimumIntertrigo by S. pyogenes |
Taken from Moraga-Llop and Tobeña Rue18
Other clinical forms of bacterial skin infections.
| Disease | Location | Aetiology | Predisposing factors | Clinical analysis | Diagnosis | Treatment |
|---|---|---|---|---|---|---|
| Blistering distal dactylitis16–18 | Soft part of the fingersInfrequent: other surfaces of palms and soles | S. pyogenesLess frequent: S. aureus, S. agalactiae | Wounds, atopic dermatitis, humidity | Blister with purulent fluid, slightly tender, with erythematous baseNo general symptoms | ClinicalConfirmation: culturea | Incision and drainage+amoxicillin–clavulanic acid 10 daysIf there is poor response cephalosporin, clindamycinMupirocin: optional (not in monotherapy) |
| Ecthyma17–19 | Lower and upper limbs | S. pyogenes, S. aureus copathogen? | Pruritic lesions: bites, scabies, pediculosis; poor hygiene; malnutrition | Ulcer with black crust that becomes chronic and heals leaving a scarComplications:cellulitis lymphagitis | ClinicalConfirmation: Gram stain and culture of exudate or biopsy of deep tissue | Removal of crusts with moist dressingsTopical fusidic acid/mupirocin if the lesion is small (<2cm)Oral 1st generation cephalosporin/amoxicillin–clavulanic acid/macrolide 7 days35Consider admission |
| Ecthyma gangrenosum17,18 | Perineum, glutei, lower limbs, apocrine areas | P. aeruginosaOther bacteria, fungi and virus (immunosuppressed) | Immunosuppression (serious neutropenia), healthy infants | Necrotic ulcer with black crust (bacterial vasculitis of small veins)Sepsis by P. aeruginosa | ClinicalConfirmation: culture of the lesions, haemocultures, skin biopsy | Early systemic treatment (intravenous) anti-Pseudomonas sp. |
| Erythrasma18 | Humid body folds: interdigital spaces of feet, groins, armpits, infra-mammalian and interglutei areas | Corynebacterium minutissimun, mixed flora, S. pyogenes | Heat, humidity, obesity, maceration of the skin, diabetes mellitus, bad hygiene | Red/brown lesions with irregular well-defined, slightly scalingMild pruritus | ClinicalWood's lamp: reddish fluorescenceaConfirmation: methylene/Gram blue staininga | Topical with erythromycin, clindamycin, mupirocin, imidazoles or Whitfield's solutionb 2 times a dayExtensive or persistent cases:oral clarithromycin for 10–14 days |
| Hidradenitis17,22 | Axilla, groins, perineum | S. aureus, Oropharyngeal anaerobes | Heat, humidity, hormonal changes, poor hygiene | Painful nodules causing abscesses leaving hypertrophic scars or fistulasVery frequent recurrence | ClinicalConfirmation: culturea | Strict hygiene+topical antiseptics/antibiotics+early oral amoxicillin–clavulanic acid/clindamycin |
| Neonatal omphalitis20 | Umbilicus or umbilical cord | Gram-negative bacilliS. aureusS. pyogenesLess frequent:anaerobes, mixed infections | Delivery at home or areas with poor health resources, improper care of cord prematurity, chorioamnionitis, premature rupture of membranes, etc. | Erythema, oedema and bad periumbilical odour, sometimes accompanied by secretion | ClinicalConfirmation: exudate culturec | Mild:–chlorhexidine+mupirocinModerate–serious:–admission, intravenous antibiotic therapy |
| Acute paronychia18 | Nail folds | S. aureus or mixed aerobe flora (S. pyogenes, Pseudomonas sp.) or anaerobe | Microtrauma, humidity, irritants (onychophagia, finger suction), contact dermatitis | Warn fold, red, swollen, painful and frequently with pus | ClinicalConfirmation: culturea | Superficial: warm, moist dressings, 2–3 times a dayDeep: incision and drainage+oral amoxicillin–clavulanic acid or cefadroxil 7 days |
| Periporitis22,24 | Occipital region, big folds, back and glutei | S. aureus | Humidity, lack of hygiene, malnutrition, chronic diseases | Mild form: miliaria pustulosaSerious form: nodules, abscesses | ClinicalConfirmation: culture | Avoid hyperhidrosisMild form: antiseptics (zinc sulfate)/mupirocinSerious form: incision and drainage+oral amoxicillin–clavulanic acid+topical mupirocin |
| Pitted keratolysis21Keratolysis plantare sulcatum16,24 | Soles of the feetRare: palms of the hands | Corynebacterium sp.Others: Dermatophilus congolensis and Kytococcus sedentarius | Humidity: hyperhidrosis, closed shoes, prolonged submersion in water | Superficial depressions of the epidermis (pitted), sometimes with linear pattern (sulcatum), bad odour, sometimes burning, stinging | ClinicalWood's lamp coral red fluorescenceaConfirmation: culturea | Treatment of hyperhidrosis+wash with antiseptic soap +topical erythromycin, clindamycin, fusidic acid or mupirocinImidazoles+topical urea or Whitfield solutionc2 times a day |
| Cellulitis-adenitis syndrome25 | Face and neck: cheeks, submandibular region | S. agalactiae | Colonisation of mucosa? | New-borns (2–6 weeks)Facial/submandibular cellulitisFever, irritability, refusal to feedIpsilateral acute otitis mediaBacteraemia: sepsis/meningitis | ClinicalAspirate cultureHaemocultureLumbar puncture: Gram staining, culture | Admission and intravenous treatment |
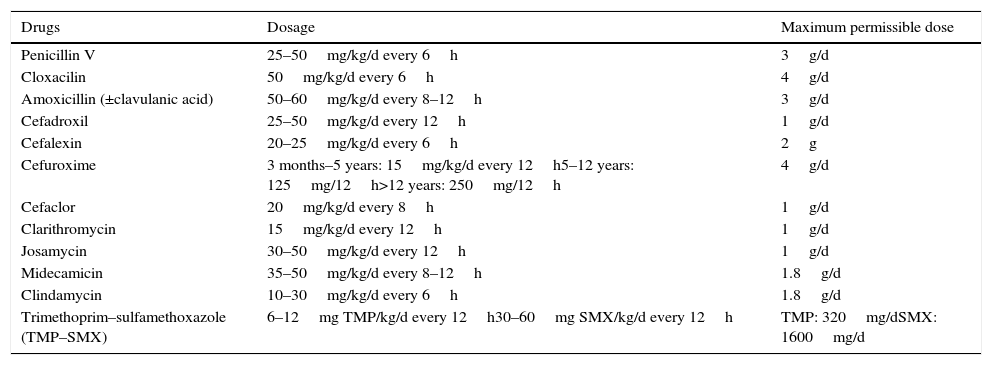
Posology of most used oral antibiotics in bacterial skin infections.a
| Drugs | Dosage | Maximum permissible dose |
|---|---|---|
| Penicillin V | 25–50mg/kg/d every 6h | 3g/d |
| Cloxacilin | 50mg/kg/d every 6h | 4g/d |
| Amoxicillin (±clavulanic acid) | 50–60mg/kg/d every 8–12h | 3g/d |
| Cefadroxil | 25–50mg/kg/d every 12h | 1g/d |
| Cefalexin | 20–25mg/kg/d every 6h | 2g |
| Cefuroxime | 3 months–5 years: 15mg/kg/d every 12h5–12 years: 125mg/12h>12 years: 250mg/12h | 4g/d |
| Cefaclor | 20mg/kg/d every 8h | 1g/d |
| Clarithromycin | 15mg/kg/d every 12h | 1g/d |
| Josamycin | 30–50mg/kg/d every 12h | 1g/d |
| Midecamicin | 35–50mg/kg/d every 8–12h | 1.8g/d |
| Clindamycin | 10–30mg/kg/d every 6h | 1.8g/d |
| Trimethoprim–sulfamethoxazole (TMP–SMX) | 6–12mg TMP/kg/d every 12h30–60mg SMX/kg/d every 12h | TMP: 320mg/dSMX: 1600mg/d |
Most superinfections of the wounds produce clinical manifestations in the first 12h, generally erythema, pain or some other type of secretion through the wound. In human bites, fever above 38°C, abscess and lymphagitis are established criteria of superinfection, as well as the presence of at least 4 of the following: erythema extending more than 3cm from the edge of the wound, pain on palpation, inflammation, purulent drainage or leukocyte count of over 12,000cells/ml.
In superinfections of puncture wounds in the foot, clinical symptoms usually begin during the first 5–7 days if the causative agent is Staphylococcus, and after 7 days if it is produced by Pseudomonas. It is important to note the infection of bones and deep tissues.23,24
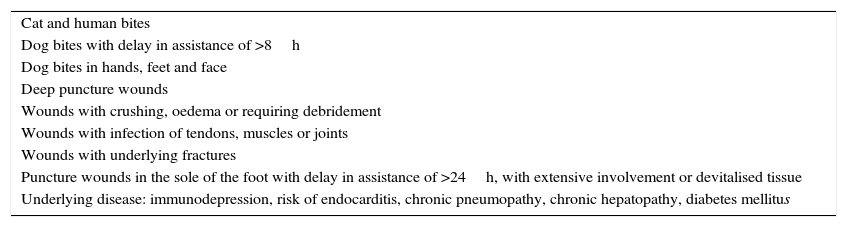
In addition to local cleaning and debridement, prophylactic antibiotic treatment is recommended only in the cases listed in Table 5 (A-I) and according to the guidelines in Table 6.
Indications of antibiotic prophylaxis in bites and puncture wounds.25
| Cat and human bites |
| Dog bites with delay in assistance of >8h |
| Dog bites in hands, feet and face |
| Deep puncture wounds |
| Wounds with crushing, oedema or requiring debridement |
| Wounds with infection of tendons, muscles or joints |
| Wounds with underlying fractures |
| Puncture wounds in the sole of the foot with delay in assistance of >24h, with extensive involvement or devitalised tissue |
| Underlying disease: immunodepression, risk of endocarditis, chronic pneumopathy, chronic hepatopathy, diabetes mellitus |
Taken from Bangert et al.25.
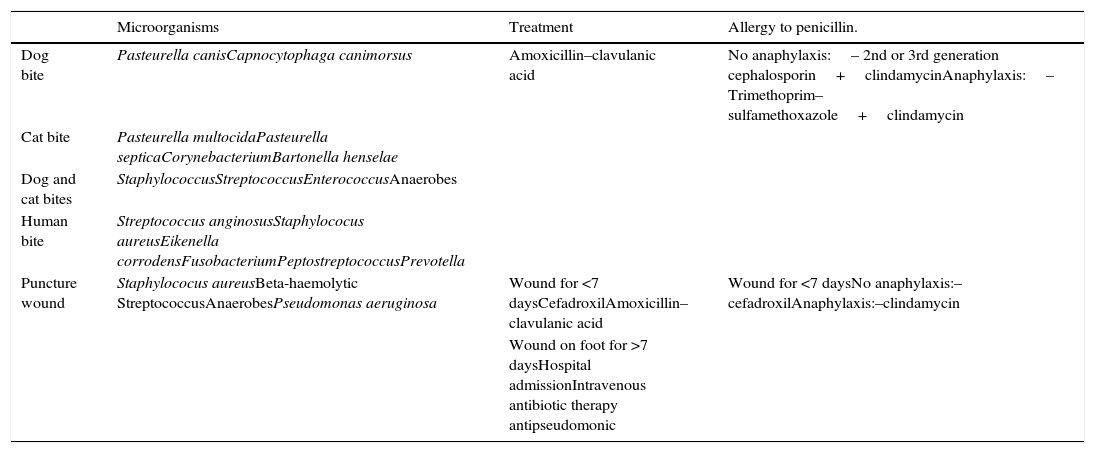
Infections secondary to bites and puncture wounds.23
| Microorganisms | Treatment | Allergy to penicillin. | |
|---|---|---|---|
| Dog bite | Pasteurella canisCapnocytophaga canimorsus | Amoxicillin–clavulanic acid | No anaphylaxis:– 2nd or 3rd generation cephalosporin+clindamycinAnaphylaxis:– Trimethoprim–sulfamethoxazole+clindamycin |
| Cat bite | Pasteurella multocidaPasteurella septicaCorynebacteriumBartonella henselae | ||
| Dog and cat bites | StaphylococcusStreptococcusEnterococcusAnaerobes | ||
| Human bite | Streptococcus anginosusStaphylococus aureusEikenella corrodensFusobacteriumPeptostreptococcusPrevotella | ||
| Puncture wound | Staphylococus aureusBeta-haemolytic StreptococcusAnaerobesPseudomonas aeruginosa | Wound for <7 daysCefadroxilAmoxicillin–clavulanic acid | Wound for <7 daysNo anaphylaxis:–cefadroxilAnaphylaxis:–clindamycin |
| Wound on foot for >7 daysHospital admissionIntravenous antibiotic therapy antipseudomonic |
Taken from Álvez González.23
Standard prophylaxis should always be considered in the case of rabies, tetanus and other diseases transmitted through wounds.
Community-acquired methicillin- resistant S. aureusEpidemiologyIn the United States, where up to 80% of staphylococci isolated in ambulatory patients are resistant to methicillin, Community-acquired methicillin- resistant S. aureus (CA-MRSA) represents a public health problem.25 In Spain, some studies in paediatric populations report a frequency of resistance to methicillin in S. aureus of 9–14.8%,26–29 but there are no studies at the national level. The frequency in neonates was investigated in the Community of Madrid30 from 2007 to 2009, and a prevalence of 3.3% was reported.
The role of methicillin resistance as an indicator of seriousness is starting to be questioned, and more relevance is being given to other virus factors, such as Panton–Valentine leukocidin (PVL),32 although most strains of PVL are also resistant to methicillin.31,33 Nosocomial MRSA is associated with certain multidrug-resistant genotypes, but this is not the case in CA-MRSA, which only rarely presents resistance to macrolides and lincosamides.27,31,33
Clinical symptoms and diagnosisAlthough they may cause pneumonia, sepsis and osteoarthritis, most CA-MRSA infections are limited to the skin and soft tissues.
There are no clinical criteria to differentiate skin infections produced by methicillin-sensitive S. aureus from those caused by MRSA,34 although in the latter, therapeutic failure and formation of abscesses and necrosis with black superficial crust similar to a spider bite are more frequent.3 Given the implications for treatment, any non-fluctuant lesions suggestive of abscesses detected during physical examination should be studied under ultrasound examination (C-III). If possible, it is recommended to take samples for culture, determination of LPV and genetic profiling.
TreatmentThe current low incidence of AC-MRSA in the paediatric population does not justify amending empirical antibiotic therapy guidelines. However, under certain circumstances changes must be considered, such as extensive cellulitis, abscesses or necrosis, the presence of recurrent abscesses in children or in other members of their household, poor response to conventional treatment, patients living in highly endemic areas (Asia, America or Eastern Europe) or living with known carriers (C-III).
In minor, non-suppurating infections (impetigo, mild superinfection of wounds, etc.), topical treatment with mupirocin is usually sufficient35 (A-III). In skin abscesses, incision and early surgical drainage are essential. This has been shown to be effective with otherwise healthy patients with non-complicated infections to achieve full healing with no adjuvant antibiotic therapy35–38 (A-II). Systemic antibiotic treatment is recommended in other localised infections, as adjuvant if drainage has been incomplete, if there is intense local infection (abscesses of more than 5cm) and in patients under 2 years of age or with other risk factors (immunosuppression, moderate-serious atopical dermatitis, etc.) (A-III).
The drug of first choice is oral clindamycin, which also inhibits the production of LPV35 (A-II). Trimethoprim–sulfamethoxazole is an effective alternative in areas where there is high resistance to clindamycin (A-II), in the event of intolerance, or when capsules are not suitable for the patient. Linezolid must be avoided in mild-moderate infections, because it is expensive, has potential adverse effects and leads to development of resistances. The presence of LPV does not require changes in the therapeutic approach although it is associated with a greater need for incision and surgical drainage.3,31
If empirical treatment is initiated with any of these drugs, changing to a betalactamic is recommended as soon as its sensitivity can be proved.
Study and treatment of carriersIt is estimated that 19.3% of the Spanish population is colonised by S. aureus, of which only 1.3% are MRSA.39 The most frequent areas of colonisation are the nostrils, but axilla inguinal and intestinal carriers have also been described.40 Considering the low incidence of MRSA in paediatrics, the systematic study of persons living with the patient is not recommended, and should be limited to outbreaks in limited communities (families, institutions, etc.) and recurrent infections3 (C-III). In these cases, decolonisation in the child and carriers living in their household should consist of nasal mupirocin every 12h and washing the body and hair with 4% chlorhexidine soap for 5–10 days (C-III). In the event of therapeutic failure with mupirocin, topical fusidic acid every 12h along with oral trimethoprim–sulfamethoxazole for 7 days should be used3,35 (C-III).
PreventionThe main transmission pathway seems to be intimate skin-to-skin contact.40 General prevention measures consist in minimising the risk of skin trauma (use of protection during sports activities, etc.) (C-III), keeping wounds clean and covered (A-III), frequent hand washing and body hygiene (A-III), avoiding sharing towels and clothes (A-III) and proper disposal of contaminated objects35,40 (C-III).
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Conejo-Fernández AJ, Martínez-Chamorro MJ, Couceiro JA, Moraga-Llop FA, Baquero-Artigao F, Alvez F, et al. Documento de consenso SEIP–AEPAP–SEPEAP sobre la etiología, el diagnóstico y el tratamiento de las infecciones cutáneas bacterianas de manejo ambulatorio. An Pediatr (Barc). 2016;84:121.