Children with asthma were considered a risk group on the advent of the SARS-CoV-2 pandemic1; after the initial alarm, several studies in different countries evinced a decreased incidence of exacerbations during the pandemic.2–4 Data on this subject have not been published in Spain.
The Working Group on Respiratory Disease of the Sociedad Española de Urgencias Pediátricas (Spanish Society of Paediatric Emergency Medicine) proposed performing a retrospective multicentre study. It consisted in analysing the monthly visits to paediatric emergency departments (PEDs) due to asthma exacerbations, defined as diagnostic code J45.909 or J45.22 of International Classification of Diseases 10th Revision (ICD-10), the proportions of cases resulting in admission to the ward and to the paediatric intensive care unit (PICU) in the first 2 years of the pandemic, and the association of exacerbations to the cumulative incidence of infection by SARS-CoV-2 at 14 days and the different quarantine periods.
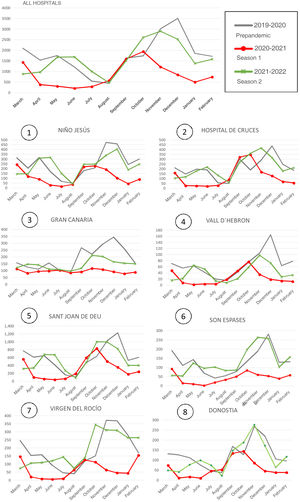
Eight hospitals agreed to participate in the study. The analysis included a total of 1 096 624 visits to participating PEDs, with 50 337 care episodes for exacerbations, 6631 admissions to the ward and 498 admissions to the PICU. Visits to the PED due to asthma exacerbations decreased by more than half in the first year of the pandemic (47.72% of the number of prepandemic visits) and grew back to a similar frequency in the second year (91.82% of the number of prepandemic visits). Although the total volume of PED visits for any reason also decreased, the decrease in the volume of visits due to exacerbations was greater. The percentage of PED visits due to exacerbations decreased from 4.73% before the pandemic to 4.09% in the first year of the pandemic (4.85% in year 2). The monthly pattern of asthma exacerbations and their association with different waves of the pandemic were very similar across participating hospitals (Fig. 1).
Visits due to asthma exacerbation in each of the 3 seasons and in each hospital. Chart reflecting the number of visits due to asthma exacerbation managed in the given month. The first chart presents the total visits due to asthma exacerbations to all participating hospitals. Subsections 1 through 8 present the data broken down by hospital.
The mean annual proportion of exacerbations leading to admission did not increase significantly: 12.23% (standard deviation [DS], 8.39%) before the pandemic; 14.00% (SD, 10.56%) in the first year of the pandemic and 13.73% (SD, 15.73%) in the second year. There was also no increase in the proportion of PICU admission: 1.00% (SD, 0.51%) before the pandemic; 0.95% (SD, 0.21%) in the first year and 1.07% (SD, 0.64%) in the second year. The risk of hospital admission and of PICU admission due to asthma exacerbation did not increase with the SARS-CoV-2 pandemic either (OR 0.88 [CI, 0.79–1.24] and OR 0.97 [CI, 0.86–1.33], respectively).
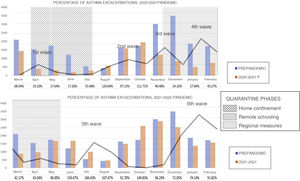
When we assessed the association between exacerbations (Fig. 2) and successive pandemic waves, we found a decrease in their incidence in the first (March 2020), third (November 2020) and fourth (January 2021) waves. During the second wave, which took place during the step-down of precautions in September 2020, there was a peak in asthma exacerbations similar to the one observed before the pandemic in every hospital except those located in islands (Fig. 1). The fifth and sixth waves, which took place after most restrictions had been lifted (August 2021; January 2022), were preceded by an increase in exacerbations in children and a decrease that coincided with the peak of SARS-CoV-2 cases. The decrease in exacerbations during the first wave has been described extensively,2–5 but the peak in exacerbations that coincided with the second wave observed in most hospitals in our case series, with the exception of those in islands, does not seem to have occurred in other countries.4,5
Percentage of visits due to asthma exacerbations relative to the same month of the year before the pandemic. The bars show the number of asthma exacerbations managed each season. The table reflects the percentage of the number of emergency visits in the pandemic seasons compared to the prepandemic period. The grey line represents the trend in SARS-CoV-2 cases each month. The shadings correspond to the different phases of the quarantine and isolation measures.
The only meta-analysis in the literature6 mentions as possible causes of the decrease in exacerbations during the pandemic the reduced exposure to respiratory viruses, the decrease in air pollution due to movement restrictions and the decreased exposure to allergens due to the use of masks. Some of these measures were analysed. Strict home confinement and restrictions to movement had a protective effect (OR, 0.27 [CI, 0.23−0.79] and OR, 0.65 [CI, 0.42−0.83]). The risk did not increase with the return to the classrooms (OR, 0.97; CI, 0.54–1.27) or with lifting the requirement to wear masks out of doors (OR 1.09; CI, 0.76–1.44). Differences between autonomous communities within Spain in the rest of applied measures precluded an analysis of their overall impact.
This is the first study on the impact of SARS-CoV-2 on visits to PEDs due to asthma exacerbations, and it was conducted in a large sample of patients managed in 8 hospitals in 6 autonomous communities. The main limitations are its retrospective design, which does not allow the establishment of causal relationships, the lack of a demographic analysis and the fact that not every region in Spain was represented, which limits the extrapolation of the findings and the conclusions on the association of the factors.
In conclusion, SARS-CoV-2 does not seem to have increased the frequency of exacerbations in children with asthma or related hospital or PICU admissions. The isolation measures introduced to control SARS-CoV-2 may have decreased exacerbations in children. One year later, the figures were once again similar to those before the pandemic. Some of the measures implemented during the pandemic could be contemplated for prevention of asthma exacerbations in children, although further research is required to determine the specific benefits of each of the measures while taking into account their psychosocial impact.
Annex 1. Working Group on Respiratory Disease of the Sociedad Española de Urgencias Pediátricas (SEUP (SEUP)Alonso Montejo, María del Mar. Hospital Universitario Virgen del Rocío*, Seville. Bustamante Hernández, Sandra. Hospital Universitari Mútua Terrassa, Terrassa, Barcelona. Claret Teruel, Gemma. Hospital Sant Joan de Déu*, Barcelona. González Díaz, Carlos. Hospital Universitario Basurto, Bilbao. Khodayar Pardo, Parisá. Hospital Clínico Universitario de Valencia, Valencia. Lera Carvallo, Esther. Hospital Universitario Vall d´Hebron*, Barcelona. Martínez Álvarez, Ana. Hospital Clínico Universitario Virgen de la Arrixaca, Murcia. Ovelar Zubiaga, Nerea. Hospital Universitario Donostia*,San Sebastian. Paniagua Calzón, Natalia. Hospital Universitario Cruces*, Bizkaia. Pavlovic Nesic, Svetlana. Hospital Universitario Materno Infantil de Las Palmas*, Las Palmas de Gran Canarias. Pérez Aragón, Ana. Hospital Universitario Virgen de las Nieves, Granada. Pérez García, Cristina. Hospital Universitario Santa Lucía de Cartagena*, Murcia. Pérez Suárez, Esther. Hospital Infantil Universitario Niño Jesús*, Madrid. Pons Morales, Sara Hospital Universitario Doctor Peset, Valencia. Soriano Arola, Marta. Hospital Universitari Son Espases*, Majorca.
*Hospitals that contributed data to the study.
We thank Dr María del Mar Alonso Montejo, Dr Marta Soriano Arola, Dr Amaia Cámara Otegui and Dr Cristina Pérez García for their invaluable collaboration in the study.
Previous meeting: partial results of this study were presented as a brief communication at the XXVI Meeting of the Sociedad Española de Urgencias de Pediatría; August 16, 2022; Pamplona, Spain.
All members of the Respiratory Task Force Spanish Society of Pediatric Emergencies (SEUP) presents in Annex 1.