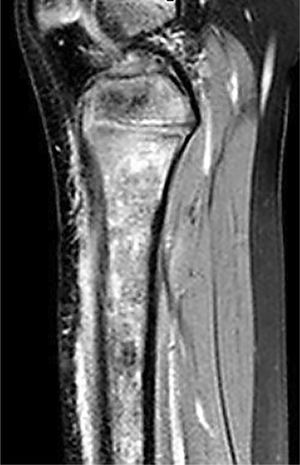
We present the case of a girl aged 6 years presenting with increasingly severe tibial pain and lameness of 10 days’ duration in the absence of fever or recent trauma. Both the patient and her mother had a previous diagnosis of hemoglobin (Hb) C trait, while her father had received a diagnosis of sickle cell trait. The patient reported having experienced several episodes of bone pain in different locations of her upper and lower extremities in the last year. The physical examination revealed pain in the right proximal tibial metaphysis on palpation, with no other relevant findings. Blood tests showed elevation of C-reactive protein (7.9mg/dL), lactate dehydrogenase (420mg/dL) and bilirubin (1.4mg/dL), while the results of the complete blood count, coagulation tests and other biochemical tests were all normal. The findings of plain radiography were unremarkable, so bone scintigraphy was performed on the suspicion of chronic nonbacterial osteomyelitis based on the previous history of recurrent episodes of musculoskeletal pain. Since scintigraphy only revealed abnormal uptake at the tibial metaphysis, the decision was made to perform an MRI scan, which revealed an extensive acute bone infarct (Figs. 1 and 2). This led to repetition of hemoglobin electrophoresis, which detected percentages of 46% of hemoglobin S and 44.5% of hemoglobin C, confirming the diagnosis of hemoglobin SC disease.
Hemoglobin SC disease, a compound heterozygous condition that manifests as the addition of sickle cell trait and HbC trait,1 neither of which has significant manifestations in isolation, results in serious disease because HbC increases the intracellular concentration of hemoglobin through loss of water, amplifying the effect of the 50% of HbS contained by increasing its tendency to polymerize.2 Hemoglobin SC disease should not be considered a mild form of sickle cell disease, but a separate disease characterized by increased blood viscosity and a higher risk of thrombotic events.