A female adolescent aged 14 years with a history of controlled coeliac disease and adequate growth (weight, 63.6 kg [89th percentile]; height, 166 cm [81st percentile]); presented with severe epigastric pain. The salient findings of the diagnostic tests performed in the referring facility were elevation of lipase (2170 IU/L), amylase (778 IU/L), aspartate aminotransferase (AST, 122 IU/L), alanine aminotransferase (ALT, 245 IU/L), gamma-glutamyl transferase (GGT, 203 IU/L), in absence of elevation of total bilirubin (0.33 mg/dL) and tissue transglutaminase IgA (tTg-IgA, 0.9 Uarb/mL; normal range, <4), as well as morphological and echogenic abnormality of the pancreas.
An assessment was scheduled for 2 weeks after, at which time the patient was asymptomatic and laboratory tests had normalised (liver function, amylase, lipase, serologic tests, IgG4, autoimmunity markers). The findings of the ultrasound scan and magnetic resonance cholangiopancreatography (MRCP) were normal. During the follow-up, the patient had steatorrhoea (elastase <15 μg/g), and required pancreatic enzyme replacement therapy for exocrine pancreatic insufficiency (EPI).
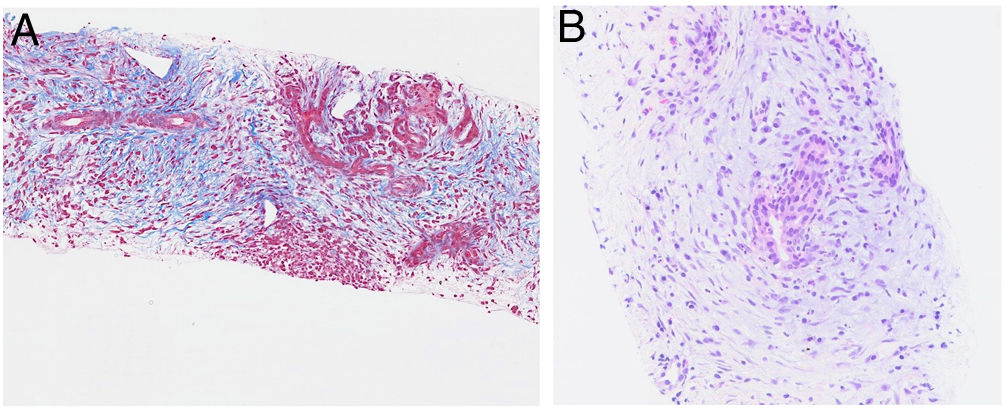
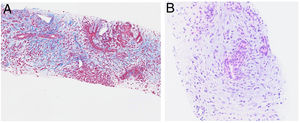
Despite the normal imaging findings, given the personal history and the progression to EPI, an echoendoscopic examination was performed, revealing hypoechogenicity and enlargement of the pancreas. The biopsy findings were compatible with autoimmune pancreatitis (AIP) type 2 (Fig. 1).
The patient received oral prednisone at a dose of 40 mg/day for 2 weeks, and treatment was tapered off over 10 weeks. The follow-up MRCP at 13 months revealed pancreatic atrophy.
The clinical presentation of AIP in children differs from the presentation in adults, as elevation of IgG4 is usually absent and the histological features are those of AIP type 2.1,2
According to the existing literature, 16% of these patients develop EPI and 61% have pancreatic atrophy within 11 months.3