Random audits are a safety tool to help in the prevention of adverse events, but they have not been widely used in hospitals. The aim of the study was to determine, through random safety audits, whether the information and material required for resuscitation were available for each patient in a neonatal intensive care unit and determine if factors related to the patient, time or location affect the implementation of the recommendations.
Material and methodsProspective observational study conducted in a level III-C neonatal intensive care unit during the year 2012. The evaluation of written information on the endotracheal tube, mask and ambu bag prepared of each patient and laryngoscopes of the emergency trolley were included within a broader audit of technological resources and study procedures. The technological resources and procedures were randomly selected twice a week for audit. Appropriate overall use was defined when all evaluated variables were correctly programmed in the same procedure.
ResultsA total of 296 audits were performed. The kappa coefficient of inter-observer agreement was 0.93. The rate of appropriate overall use of written information and material required for resuscitation was 62.50% (185/296). Mask and ambu bag prepared for each patient was the variable with better compliance (97.3%, P=.001). Significant differences were found with improved usage during weekends vs. working-day (73.97 vs. 58.74%, P=.01), and the rest of the year vs. 3rd quarter (66.06 vs. 52%, P=.02).
ConclusionsOnly in 62.5% of cases was the information and the material necessary to attend to a critical situation urgently easily available. Opportunities for improvement were identified through the audits.
Las auditorías en tiempo real son una herramienta de seguridad que apenas se ha aplicado anteriormente en el ámbito hospitalario. El objetivo del estudio fue determinar mediante auditorías si la información y el material necesario para la reanimación estaban disponibles para cada paciente de cuidados intensivos y si factores relacionados con el paciente, el momento o su ubicación en la unidad influyen en el cumplimiento de las recomendaciones.
Material y métodosEstudio observacional prospectivo realizado durante el año 2012 en una unidad neonatal nivel III-C. Dentro de un estudio más amplio de auditorías de recursos tecnológicos y procedimientos se incluyó la evaluación de la información escrita sobre el tubo endotraqueal, mascarilla y ambú de cada paciente y los laringoscopios del carro de parada. Dos veces por semana al azar se seleccionaba qué procedimiento o recurso se iba a evaluar. Se definió la variable uso global adecuado cuando todos los ítems evaluados eran correctos en el mismo procedimiento.
ResultadosSe realizaron 17 auditorías que incluyeron 296 valoraciones. El coeficiente kappa interobservador fue 0,93. La frecuencia de uso global adecuado de la información y el material de reanimación fue de 62,50% (185/296). La mascarilla y ambú preparado en cada paciente fue la variable mejor cumplimentada (97,3%; p=0,001). El uso global adecuado fue mejor en días festivos que en laborables (73,97 vs. 58,74%; p=0,01) y el resto del año frente al verano (66,06 vs. 52%; p=0,02).
ConclusionesSolo en el 62,5% de los casos toda la información y el material necesario para atender una situación crítica de forma urgente estaba fácilmente disponible. Gracias a las auditorías se identificaron oportunidades de mejora.
Adverse health care events are a significant problem worldwide, as they are associated with a high morbidity in the short and long term.1–4 In the case of neonatal intensive care units (NICUs), several studies have demonstrated that adverse events are a substantial problem, and all possible efforts are being made to minimise their occurrence.5–8 Furthermore, critical unplanned events often happen in the NICU that favour the occurrence of adverse events. Therefore, it is essential that we identify the essential equipment needed to address these situations, such as every component needed to intubate and ventilate patients during resuscitation, and ensure that equipment is always accessible and functions correctly.
There are various safety tools at our disposal, including real-time safety audits (RTSAs), which are widely used in high-risk industries on account of their considerable ability to identify errors and risk situations and facilitate their prevention.9,10 However, this approach has barely been applied to hospital settings.
For these reasons, we decided to use RTSAs to assess the adherence in our NICU to recommendations regarding the ventilation equipment that needs to be ready at each patient's station, the intubation equipment in each crash trolley and the documentation necessary to manage a critical situation. The aim of our study was to determine by means of audits whether the documentation and equipment needed for resuscitation was ready for each intensive care patient, and whether factors related to patient characteristics, the time of admission or the location in the unit had an impact on the degree of adherence to recommendations.
Materials and methodsWe conducted a prospective observational study between January 1 and December 31, 2012 in the framework of a broader study whose purpose is to determine whether safety mechanisms in devices and protocols for the performance of the most frequent procedures were used correctly by conducting RTSA rounds. In this article, we will only describe the variables related to the documentation and equipment for ventilation in resuscitation during critical situations. Previous articles published by our group11,12 described other variables assessed in the broader project, such as those related to monitoring and invasive and noninvasive mechanical ventilation systems and infusion pumps.
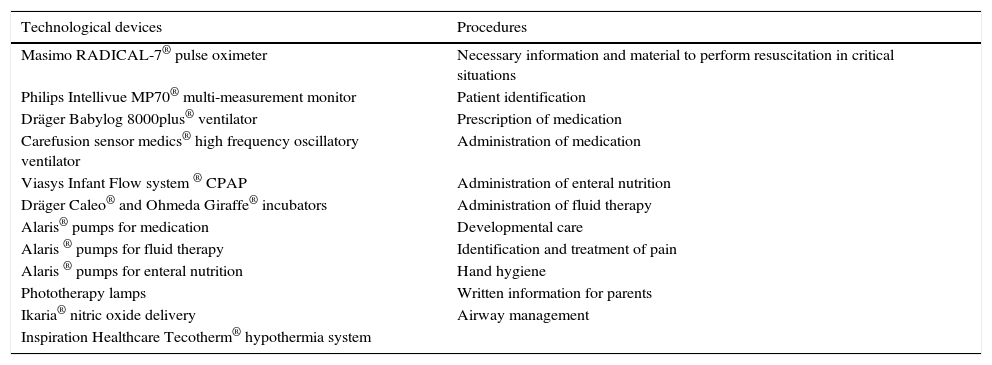
We started by consulting with physicians and nurses using a modified Delphi method to determine which were the devices and procedures for which recommendations were neglected most often in order to ensure the inclusion of the most relevant devices and procedures in the study. We included a total of 23 devices/procedures (Table 1). To carry out the audits, we created different cards detailing the variables that had to be evaluated for a given device or procedure.
Technological devices and procedures included in the study.
| Technological devices | Procedures |
|---|---|
| Masimo RADICAL-7® pulse oximeter | Necessary information and material to perform resuscitation in critical situations |
| Philips Intellivue MP70® multi-measurement monitor | Patient identification |
| Dräger Babylog 8000plus® ventilator | Prescription of medication |
| Carefusion sensor medics® high frequency oscillatory ventilator | Administration of medication |
| Viasys Infant Flow system ® CPAP | Administration of enteral nutrition |
| Dräger Caleo® and Ohmeda Giraffe® incubators | Administration of fluid therapy |
| Alaris® pumps for medication | Developmental care |
| Alaris ® pumps for fluid therapy | Identification and treatment of pain |
| Alaris ® pumps for enteral nutrition | Hand hygiene |
| Phototherapy lamps | Written information for parents |
| Ikaria® nitric oxide delivery | Airway management |
| Inspiration Healthcare Tecotherm® hypothermia system |
For every week in the period under study, we randomly selected 2 days (weekdays or weekend days) and one shift (morning or evening). We also selected two cards at random to conduct the audit on selected day. One researcher (EBS or MCPG, both of who are clinical neonatologists employed in the unit) determined the devices or procedures that needed to be audited and were in use in any of the patients each day, and audited the variables under study for the selected devices or procedures.
When it came to the documentation and equipment needed for ventilation in critical situations, the audited variables concerned the documentation written in the chart of each patient (size and length of endotracheal tube recorded in patient chart [yes/no], size and length of nasogastric tube recorded in patient chart [yes/no]), the ventilation supplies available at each patient's station (bag-valve mask and mask of appropriate size ready in each station [yes/no]) and the laryngoscopes in the crash trolley of each intensive care room (0 and 00 handles and blades in the crash trolley [yes/no], and correct functioning of laryngoscopes (yes/no]). We also defined a variable called overall appropriate use that was only considered positive when all items evaluated for a specific procedure were in order, that is, if correct information concerning endotracheal and nasogastric tubes had been entered in the patient's chart, the bag-valve mask and the appropriate mask were available in the incubator, and the laryngoscopes in the room where the newborn was located functioned correctly and there was a sufficient supply of 0 and 00 size blades. “Overall use” was only considered appropriate if all of the above was correctly done for a given patient. Furthermore, we analysed the degree of agreement between the 2 researchers by conducting simultaneous auditing rounds.
With the exception of the department chief and the nurse supervisors, the staff of the NICU were unaware of the purpose of the auditing, but when serious errors that may have posed a danger to patients were detected, the staff in charge of the patient were immediately notified.
Our unit is a III-C level NICU with 500 admissions a year. The NICU is divided into 3 intensive care rooms of different characteristics: a large room with 10 intensive care beds (NIC-A) and 2 small rooms with 4 and 5 intensive care beds (NIC-B and NIC-C) and 2 additional rooms with 24 intermediate care beds. The patient/nurse ratio in the NICU is 2:1.
Other variablesWe collected data on patient, time of admission and NICU characteristics to assess whether they had an impact on adherence to the protocols for the procedures: birth weight, gestational age (GA), sex, workweek or weekend/holiday, morning or evening shift, NICU occupancy at time of audit and location of patient in the unit.
Ethical considerationsThe object of the study was the auditing of equipment and procedures in the neonatal department. We consulted with the Clinical Research Ethics Committee and verified that current Spanish law does not require a review by an Ethics Committee for this type of study. We obtained the informed consent of the department head and supervisors.
Statistical analysisWe have expressed continuous variables as mean±standard deviation (SD) and categorical variables as absolute and relative frequencies. We used the chi square test or Fisher's exact test with contingency tables to compare proportions and determine the statistical significance of their differences. We compared the distribution of ordinal and continuous values by means of Student's t test or the Wilcoxon–Mann–Whitney test, as applicable. We performed logistic regression to assess the strength of the association between appropriate use and several variables including GA, birth weight, sex, location in NICU, weekday or weekend/holiday, morning or evening shift, month and unit occupancy. We present the results in the form of 95% confidence intervals.
ResultsDuring the period under study, we performed 17 audits that included 296 evaluations of the documentation and equipment required for resuscitation in critical situations that we have already described. The kappa coefficient corresponding to the agreement of the 2 researchers that carried out the audits was 0.93.
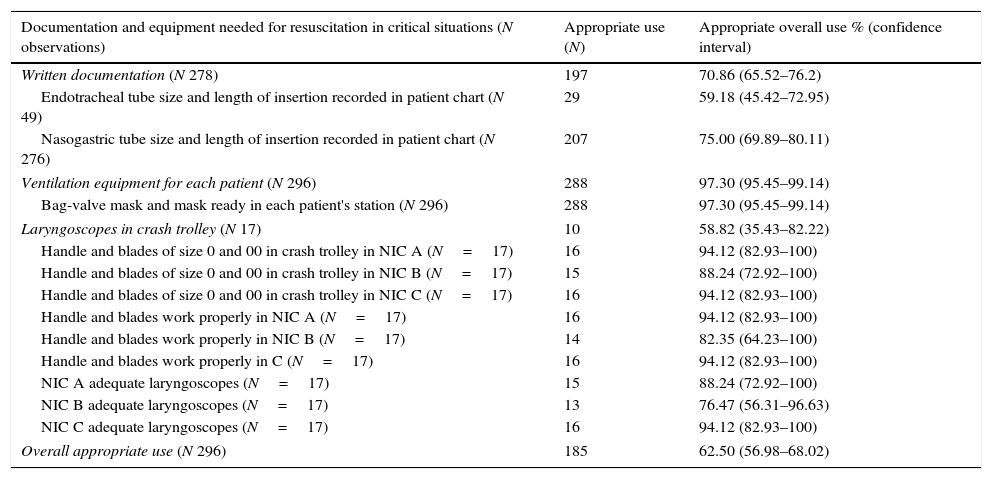
The frequency of the overall appropriate use of the necessary information and equipment for ventilation in resuscitation in critical situations was 62.50% (185/296). Table 2 presents the frequencies of appropriate adherence to recommendations for the different variables under study. The variable for which we found the highest degree of adherence was the ventilation equipment at the patient's station (97.3%; P=.001).
Frequency of adherence to recommended documentation and equipment for resuscitation in critical situations.
| Documentation and equipment needed for resuscitation in critical situations (N observations) | Appropriate use (N) | Appropriate overall use % (confidence interval) |
|---|---|---|
| Written documentation (N 278) | 197 | 70.86 (65.52–76.2) |
| Endotracheal tube size and length of insertion recorded in patient chart (N 49) | 29 | 59.18 (45.42–72.95) |
| Nasogastric tube size and length of insertion recorded in patient chart (N 276) | 207 | 75.00 (69.89–80.11) |
| Ventilation equipment for each patient (N 296) | 288 | 97.30 (95.45–99.14) |
| Bag-valve mask and mask ready in each patient's station (N 296) | 288 | 97.30 (95.45–99.14) |
| Laryngoscopes in crash trolley (N 17) | 10 | 58.82 (35.43–82.22) |
| Handle and blades of size 0 and 00 in crash trolley in NIC A (N=17) | 16 | 94.12 (82.93–100) |
| Handle and blades of size 0 and 00 in crash trolley in NIC B (N=17) | 15 | 88.24 (72.92–100) |
| Handle and blades of size 0 and 00 in crash trolley in NIC C (N=17) | 16 | 94.12 (82.93–100) |
| Handle and blades work properly in NIC A (N=17) | 16 | 94.12 (82.93–100) |
| Handle and blades work properly in NIC B (N=17) | 14 | 82.35 (64.23–100) |
| Handle and blades work properly in C (N=17) | 16 | 94.12 (82.93–100) |
| NIC A adequate laryngoscopes (N=17) | 15 | 88.24 (72.92–100) |
| NIC B adequate laryngoscopes (N=17) | 13 | 76.47 (56.31–96.63) |
| NIC C adequate laryngoscopes (N=17) | 16 | 94.12 (82.93–100) |
| Overall appropriate use (N 296) | 185 | 62.50 (56.98–68.02) |
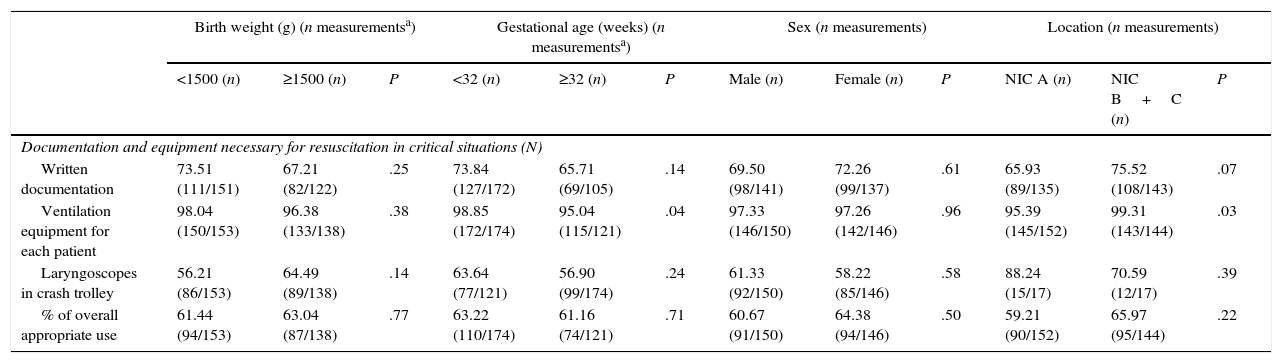
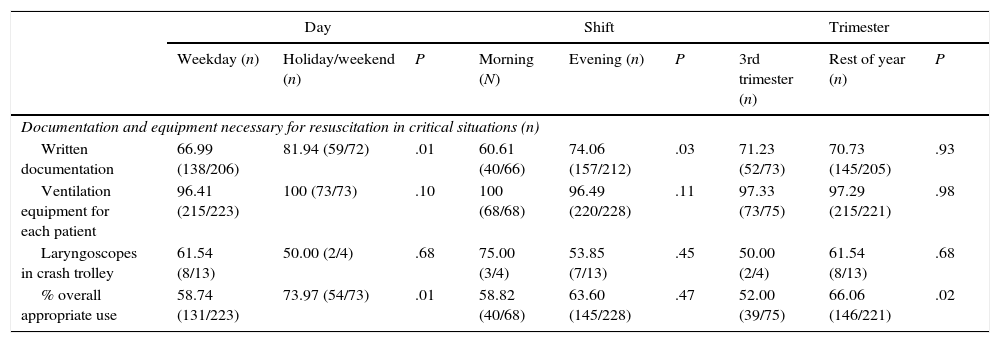
Table 3 presents the results on the overall appropriate use of documentation and materials needed for ventilation during resuscitation in critical situations in relation to patient characteristics and location in the unit, and Table 4 describes the results on overall appropriate use in relation to time characteristics. Overall appropriate use was greater in weekends or holidays compared to weekdays (73.97% vs. 58.74%; P=.01), and lesser in the summer compared to the rest of the year (52% vs. 66.06%; P=.02). Adherence to recommendations on ventilation supplies at individual patient stations was better in newborns of less than 32 weeks’ GA and in patients located in the NIC-B or C (98.85% for GA <32 weeks compared to 95.04% for GA ≥32 weeks [P=.04]; 95.39% in NIC-B/C vs. 99.31% in NIC-A [P=.03]). Documentation in patients’ charts was better on weekends/holidays and in the evening shift (81.94% on weekends/holidays vs. 66.99% on weekdays [P=.01]; 74.06% in the evening shift vs. 60.61% in the morning shift [P=.03]).
Frequency of adherence to recommended documentation and equipment for resuscitation by patient characteristics and unit location.
| Birth weight (g) (n measurementsa) | Gestational age (weeks) (n measurementsa) | Sex (n measurements) | Location (n measurements) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| <1500 (n) | ≥1500 (n) | P | <32 (n) | ≥32 (n) | P | Male (n) | Female (n) | P | NIC A (n) | NIC B+C (n) | P | |
| Documentation and equipment necessary for resuscitation in critical situations (N) | ||||||||||||
| Written documentation | 73.51 (111/151) | 67.21 (82/122) | .25 | 73.84 (127/172) | 65.71 (69/105) | .14 | 69.50 (98/141) | 72.26 (99/137) | .61 | 65.93 (89/135) | 75.52 (108/143) | .07 |
| Ventilation equipment for each patient | 98.04 (150/153) | 96.38 (133/138) | .38 | 98.85 (172/174) | 95.04 (115/121) | .04 | 97.33 (146/150) | 97.26 (142/146) | .96 | 95.39 (145/152) | 99.31 (143/144) | .03 |
| Laryngoscopes in crash trolley | 56.21 (86/153) | 64.49 (89/138) | .14 | 63.64 (77/121) | 56.90 (99/174) | .24 | 61.33 (92/150) | 58.22 (85/146) | .58 | 88.24 (15/17) | 70.59 (12/17) | .39 |
| % of overall appropriate use | 61.44 (94/153) | 63.04 (87/138) | .77 | 63.22 (110/174) | 61.16 (74/121) | .71 | 60.67 (91/150) | 64.38 (94/146) | .50 | 59.21 (90/152) | 65.97 (95/144) | .22 |
Frequency of adherence to recommended documentation and equipment for resuscitation by temporal characteristics.
| Day | Shift | Trimester | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Weekday (n) | Holiday/weekend (n) | P | Morning (N) | Evening (n) | P | 3rd trimester (n) | Rest of year (n) | P | |
| Documentation and equipment necessary for resuscitation in critical situations (n) | |||||||||
| Written documentation | 66.99 (138/206) | 81.94 (59/72) | .01 | 60.61 (40/66) | 74.06 (157/212) | .03 | 71.23 (52/73) | 70.73 (145/205) | .93 |
| Ventilation equipment for each patient | 96.41 (215/223) | 100 (73/73) | .10 | 100 (68/68) | 96.49 (220/228) | .11 | 97.33 (73/75) | 97.29 (215/221) | .98 |
| Laryngoscopes in crash trolley | 61.54 (8/13) | 50.00 (2/4) | .68 | 75.00 (3/4) | 53.85 (7/13) | .45 | 50.00 (2/4) | 61.54 (8/13) | .68 |
| % overall appropriate use | 58.74 (131/223) | 73.97 (54/73) | .01 | 58.82 (40/68) | 63.60 (145/228) | .47 | 52.00 (39/75) | 66.06 (146/221) | .02 |
The occupation rate in the unit when overall use was appropriate was 95.02% (79–105%) compared to 93.10% when overall use was inappropriate (79–105%) (P=.03).
DiscussionOur prospective observational study showed a percentage lower than expected of adherence to recommendations on the information recorded in patient charts, the material ready for ventilation for each patient and the preparation of laryngoscopic equipment in crash trolleys. More specifically, had there been a critical situation, the documentation and full equipment needed for resuscitation would only have been readily available for 62% of the patients. This is a very important aspect in patient safety, since the perceptions of health professionals may significantly diverge from reality, as was the case in our study. We do not know of any other study that specifically assessed the same items as we did here.
The availability of a bag-valve mask and mask of appropriate size by each patient was the variable for which we found the highest degree of adherence. We found no significant differences in any of the other variables under study.
The RTSAs detected flaws in the resuscitation equipment in nearly 40% of instances. As we already noted, we could not compare this result with others in the literature. We only found one study that reported that 31% out of 693 surveyed paediatric anaesthesiologists had experienced problems with the difficult airway trolley.13 Since these data originated from a survey, a comparison would be challenging, as they may be affected by recall bias. The success of advanced life support measures partly depends on the availability of a resuscitation trolley with the necessary equipment and medication. Missing or defective equipment can significantly compromise resuscitation efforts.14 Current recommendations call for the staff in the unit to check the contents of the crash trolley, restock supplies as needed for all devices and check the expiration date of drugs, and for designating a staff member to be responsible for checking and maintaining the crash trolley.14,15
Contrary to what we expected, we found that admission during weekends, holidays or evening shifts and high unit occupancy did not foster non-adherence to recommendations on the safety variables under study. Attenello et al. found that weekend admission was associated with a higher probability of adverse events, increased length of stay and increased costs.16 In contrast, in our study we found a higher degree of adherence to recommendations during weekends and holidays (weekends/holidays, 73.97% vs. weekdays, 58.74%; P=.01). Our research group had already found a higher degree of adherence in the use of safety mechanisms in monitoring and invasive mechanical ventilation equipment in a previous study.11 Perhaps this is because the workflow is different on weekends and holidays, with fewer interruptions, allowing the staff to focus better on their work. It is also possible that the professionals that cover weekend shifts are not the same as those scheduled during the week. In our department, weekend shifts are not covered by a fixed staff, and the same professionals that work weekdays are scheduled for these shifts; nevertheless, if data on staff characteristics had been available, it would have been interesting to compare them.
When it came to the readiness of ventilation equipment in individual patient stations, we observed that adherence was better for preterm newborns with GAs of less than 32 weeks and patients located in the NIC-B or NIC-C rooms. These rooms are the smallest and are where patients born at less than 30 weeks’ gestation are usually hospitalised. They are quieter, darker and calmer, and have a less stressful environment, which promotes clinical stability and neurodevelopment in preterm newborns, who are the most vulnerable patients.17–19 Perhaps their smaller size makes it easier to control equipment and keep everything in order.
We also wanted to compare the months of July, August and September with the rest of the year, as we consider the summer a period with an increased risk of adverse events because less experienced staff is scheduled to cover for vacations. We found that adherence to recommendations during these months was lower compared to the rest of the year (52% in the summer compared to 66.06% in the rest of the year; P=.02), which was similar to the results of a study conducted by Utrera Torres et al. that found a higher incidence of accidental extubation in the summer period.20
When it came to occupancy, while the results were statistically significant and suggested that the greater the occupancy the greater the adherence (95.02 vs. 93.10%; P=.03), they may not be clinically relevant because occupancy in our unit is always very high (≥90%).
In our study, RTSAs were effective in detecting weaknesses in the system that would have gone unnoticed otherwise. Ursprung et al. were the first to demonstrate the usefulness of RTSAs in a NICU, as they found that auditing contributed to the prevention of future errors by detecting flaws in the system.5,9 Another study that implemented safety rounds with hospital managers in adult and paediatric intensive care units had similar results, as these audits succeeded in improving aspects of great importance to patient safety.21 Our team has also demonstrated that the use of RTSAs to assess safety in the use of infusion pumps achieved significant improvements in their use.12 Based on the findings of this study, and in agreement with the nursing staff, we have established that 1 random audit will be carried out every week by either of 2 of the authors of the study (EBS, CPG) to assess adherence to recommendations, especially in relation to the crash trolley. We have developed a checklist for the purpose that includes all the elements that need to be evaluated. The resulting information is to be collected and analysed once every trimester.
One of the limitations of the study was that due to the time constraints of researchers, we were unable to include night shifts in the audits. Auditing weekends and night shifts is advisable because differing issues might arise during these compared with day shifts or weekdays, since there may be changes in staff and workflow organisation.9 In our department, night shifts are not fixed and are covered by the same staff that works morning and evening shifts. Another limitation was the small sample size in the analysis of the presence and functioning of laryngoscopes in crash trolleys, because while trolleys were inspected in every audit, there is only one trolley in each intensive care room.
The adherence to recommendations regarding the documentation and equipment needed for ventilation in resuscitation of critical patients was lower than expected. Real-time safety audits helped detect risk situations that will allow us to develop strategies to improve adherence to protocols as regards patient safety.
FundingWe received a small amount of money from Massimo and Carefusion used exclusively to fund the database for collecting the study data. The funding sources did not participate in any capacity in the design or performance of the study.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Bergon-Sendin E, Perez-Grande MC, Lora-Pablos D, Melgar-Bonis A, Ureta-Velasco N, Moral-Pumarega MT, et al. Auditorías de seguridad en tiempo real en una unidad neonatal. An Pediatr (Barc). 2017;87:148–154.
Previous presentations: This study was presented in part at the I Jornada de Investigación en Medicina Perinatal organised by the SENeo; October 23, 2012; Madrid, Spain; the XXIV Congreso de Neonatología y Medicina Perinatal organised by the SENeo; October 4, 2013; Barcelona, Spain; the 5th Congress of the European Academy of Paediatric Societies; October 20, 2014; Barcelona, Spain; the II Jornadas de Investigación en Medicina Perinatal organised by the SENeo; September 30, 2014; Madrid, Spain; and the XXV Congreso de Neonatología and V Congreso de Enfermería Neonatal; May 20–22, 2015; Seville, Spain.