Heart rate (HR) assessment is essential during neonatal resuscitation, and it is usually done by auscultation or pulse oximetry (PO). The aim of the present study was to determine whether HR assessment with ECG is as fast and reliable as PO during preterm resuscitation.
Material and methodsThirty-nine preterm (<32 weeks of gestational age and/or <1500g of birth weight) newborn resuscitations were video-recorded. Simultaneous determinations of HR using ECG and PO were registered every 5s for the first 10min after birth. Time needed to place both devices and to obtain reliable readings, as well as total time of signal loss was registered. The proportion of reliable HR readings available at the beginning of different resuscitation manoeuvres was also determined.
ResultsTime needed to connect the ECG was shorter compared with the PO (26.64±3.01 vs. 17.10±1.28s, for PO and ECG, respectively, P<.05). Similarly, time to obtain reliable readings was shorter for the ECG (87.28±12.11 vs. 26.38±3.41s, for PO and ECG, respectively, P<.05). Availability of reliable HR readings at initiation of different resuscitation manoeuvres was lower with the PO (PO vs. ECG for positive pressure ventilation: 10.52 vs. 57.89% P<.05; intubation: 33.33 vs. 91.66%, P<.05). PO displayed lower HR values during the first 6min after birth (P<.05, between 150 and 300s).
ConclusionsReliable HR is obtained later with the PO than with the ECG during preterm resuscitation. PO underestimates HR in the first minutes of resuscitation.
La medición de frecuencia cardíaca (FC) es esencial durante la reanimación neonatal y se realiza habitualmente mediante auscultación o pulsioximetría (PO). El objetivo de este estudio es analizar si durante la reanimación del recién nacido prematuro la medición de la FC mediante ECG es tan precoz y fiable como la PO.
Material y métodosSe realizó video-grabación de la reanimación de 39 recién nacidos prematuros (<32 semanas o <1.500 g), registrando medidas de FC simultáneamente mediante ECG y PO cada 5 s desde el nacimiento hasta los 10 min de vida. Se determinó el tiempo necesario para colocación, obtención de lectura fiable y pérdida de señal de ambos dispositivos, así como la proporción de medida fiable de FC al inicio de cada maniobra de reanimación.
ResultadosEl tiempo de colocación fue menor en ECG que en PO (17,10 ± 1,28 s vs. 26,64 ± 3,01 s; p < 0,05). Igualmente, el tiempo desde el fin de la colocación hasta la obtención de una lectura fiable fue menor para ECG que para PO (26,38 ± 3,41 s vs. 87,28 ± 12,11 s; p < 0,05). La proporción de medidas fiables de la FC al inicio de la reanimación fue menor en PO (PO vs. ECG para ventilación con presión positiva: 10,52 vs. 57,89%; p < 0,05; intubación: 33,33 vs. 91,66%; p < 0,05). La PO subestimó la FC con medidas inferiores a las del ECG durante los primeros 6 min de vida (p < 0,05 entre los 150 y 300 s).
ConclusionesEn la reanimación del prematuro la obtención de la FC fiable es más tardía con la PO que con ECG; además, la PO subestima la FC en los primeros momentos de la reanimación.
International guidelines on neonatal resuscitation indicate that of all the parameters that guide both initiation of resuscitation as well as its continuation, an increase in heart rate (HR) is the quickest and most reliable indicator of resuscitation efficacy.1,2 Furthermore, progression to different steps during resuscitation fundamentally depends on the evolution of this parameter. Therefore, HR measurement is an essential element of neonatal resuscitation. Until recently, HR was measured exclusively by clinical assessment, either auscultation of precordial pulse or palpation of the base of the umbilical cord.1 However, clinical assessment underestimates HR compared to measurement by electrocardiography (ECG).3 Thus, the most up-to-date recommendations for neonatal resuscitation (International Liaison Committee on Resuscitation) establish that a preductal pulse oximeter (PO) should be placed on newborns when the need of resuscitation is anticipated.1 However, the time needed to obtain a reliable HR reading with a PO may range between 68 and 92s,3,4 so that even if the PO were placed at birth, a reliable HR would not be obtained until this time interval had elapsed. Considering that based on international resuscitation guidelines severely depressed newborns could be intubated, ventilated with positive pressure and undergoing chest compressions by 90s of life, the above suggests that in many instances these interventions are performed when reliable HR measurements are not yet available.
Thus, a method is needed to measure HR that can provide early and reliable data to guide correct implementation of neonatal resuscitation recommendations. Electrocardiography is currently the gold standard for measuring HR.3 The mean starting time of reliable data collection described in the literature for ECG ranges approximately between 30 and 80s.5–8 There is evidence that ECG provides HR data faster than pulse oximetry.6–8 While the literature describes an overall strong correlation between ECG and PO measurements,9 recent data suggest that this correlation is weak in the first minutes after birth, with significantly lower PO-derived HR values in the first 7min of life, and the most pronounced differences occurring in the first 2min.8 Most of the published studies on this subject included few very low birth weight newborns that required advanced resuscitation.3 Few data are available on the correlation between PO and ECG during resuscitation of very low birth weight newborns at birth, who are precisely the patients in whom methodical and appropriate resuscitation has the greatest impact on subsequent morbidity and mortality.8,9
The aim of our study was to analyse whether HR monitoring by ECG contributes faster and more reliable data than pulse oximetry during resuscitation in neonates born at less than 32 weeks’ gestation or weighing less than 1500g.
Materials and methodsWe conducted a retrospective study between May 2012 and November 2014 in the delivery room. The study included newborns less than 32 weeks’ gestational age or with birth weights of less than 1500g. We calculated a sample size of 70 patients, but discontinued recruitment after 39 patients once we had obtained statistically significant results. We excluded patients with chromosomal anomalies, short life expectancies, or in whom it was decided not to attempt complete resuscitation at birth. Failure to obtain the informed consent of the parents or guardians was an additional exclusion criterion. The study adhered to the principles of the Declaration of Helsinki and was approved by the Ethics Committee of our hospital.
For the purposes of data collection, we made video recordings of the resuscitations with two cameras (HD Webcam C270 with high definition recording capabilities of up to 1280×720 pixels and an integrated microphone with noise-reduction software). One of the cameras was attached to a metal extension pole placed over the resuscitation cot. This camera recorded resuscitation measures, times of PO sensor and ECG electrode placement, and the PO screen. The second camera recorded the ECG monitor (Nellcor Oximax N5600, Tyco Healthcare Group, Pleasanton, CA, United States), which was hidden from the resuscitation team. The HR sound output was disabled to prevent it from interfering with the usual resuscitation practices. Three ECG electrodes were used (Ambu Blue sensor BRS-50-K/EU/3), which were arranged on the resuscitation platform and connected to the monitor prior to delivery. We used latest-generation oximeters (Masimo Radical 7, Masimo, Irvine, CA, United States) configured for maximum sensitivity and a mean reading time of 2s. Right after birth, the PO sensor (LNCS Neo-L, Masimo, Irvine, CA, United States) was placed on the right hand or wrist of the newborn and then connected to the device in order to obtain faster readings.4 Once the PO had been placed, the chest of the patient was wiped dry and the three ECG electrodes placed. The PO and the ECG electrodes were placed sequentially by the neonatal nurse. Therefore, the times of placement for each device were measured from the moment the nurse picked up the electrodes or the PO sensor to the moment placement was completed.
We defined a reliable HR measurement in the ECG monitor as a HR value displayed along with clearly visible QRS complexes. In the case of PO, the HR value was considered reliable when the device displayed HR and SpO2 values with an oscillatory plethysmographic waveform and tall IQ signal bars.
Resuscitation teams consisted of a minimum of three staff. Resuscitation measures were performed adhering to international guidelines and guided by the HR measured by clinical assessment or PO.
Data collection started from the moment the newborn was placed on the resuscitation cot and ended at 10min of life or at the end of the stabilisation-resuscitation period once the newborn was transfered to the neonatal intensive care unit (NICU).
The recorded resuscitations were subsequently analysed by three researchers, and every recording was reviewed by all three. The researchers entered the HR measurements obtained by each device at 5-s intervals in a spreadsheet. For every 30-s interval, the mean HR obtained by PO and ECG for that time point was calculated 5s before, and 5s after, for their subsequent analysis. The researchers also collected the times spent on placement of the PO and ECG electrodes, the delay until reliable HR readings were obtained from the beginning and from completion of ECG and PO placement, and the total time of signal loss for both devices. They documented the resuscitation measures that had been implemented, and the ECG- and PO-derived HR measurements at the time they were initiated.
The statistical analysis was performed with the SPSS package (version 21.0.0.0. IBM Corp. Armonk, New York, United States). Descriptive data were expressed as mean and standard error or absolute frequencies and percentages. The means were compared with Student's t test or the Wilcoxon sign-rank test, and analysed 2×2 contingency tables by means of Fisher's exact test.
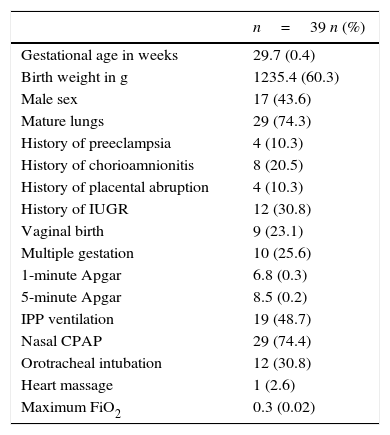
ResultsForty-five resuscitations were video recorded between May 2012 and November 2014. Six were excluded from the analysis due to problems in the recording process, so the final analysis included 39 recordings. Table 1 presents the characteristics of the sample under study.
Characteristics of the population under study and measures used during resuscitation in the delivery room.
| n=39 n (%) | |
|---|---|
| Gestational age in weeks | 29.7 (0.4) |
| Birth weight in g | 1235.4 (60.3) |
| Male sex | 17 (43.6) |
| Mature lungs | 29 (74.3) |
| History of preeclampsia | 4 (10.3) |
| History of chorioamnionitis | 8 (20.5) |
| History of placental abruption | 4 (10.3) |
| History of IUGR | 12 (30.8) |
| Vaginal birth | 9 (23.1) |
| Multiple gestation | 10 (25.6) |
| 1-minute Apgar | 6.8 (0.3) |
| 5-minute Apgar | 8.5 (0.2) |
| IPP ventilation | 19 (48.7) |
| Nasal CPAP | 29 (74.4) |
| Orotracheal intubation | 12 (30.8) |
| Heart massage | 1 (2.6) |
| Maximum FiO2 | 0.3 (0.02) |
Data are expressed as mean (standard error), n (%).
IUGR, intrauterine growth restriction; CPAP, continuous positive airway pressure; FiO2, fraction of inspired oxygen; IPP, intermittent positive pressure.
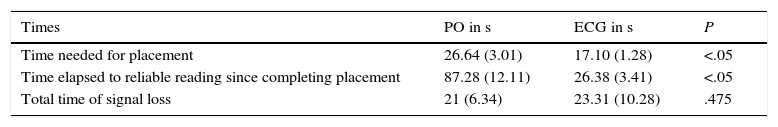
The time spent in placement of ECG electrodes was nearly 30% shorter than the time spent on placing the PO (Table 2). Furthermore, the delay in obtaining reliable HR measurements from the end of placement was nearly 70% shorter when ECG was used compared to PO (Table 2). The difference in the total time of signal loss was not statistically significant (Table 2).
Placement, reliable reading and signal loss times.
| Times | PO in s | ECG in s | P |
|---|---|---|---|
| Time needed for placement | 26.64 (3.01) | 17.10 (1.28) | <.05 |
| Time elapsed to reliable reading since completing placement | 87.28 (12.11) | 26.38 (3.41) | <.05 |
| Total time of signal loss | 21 (6.34) | 23.31 (10.28) | .475 |
Data are expressed as mean (standard error).
ECG, electrocardiogram; PO, pulse oximeter; s, seconds.
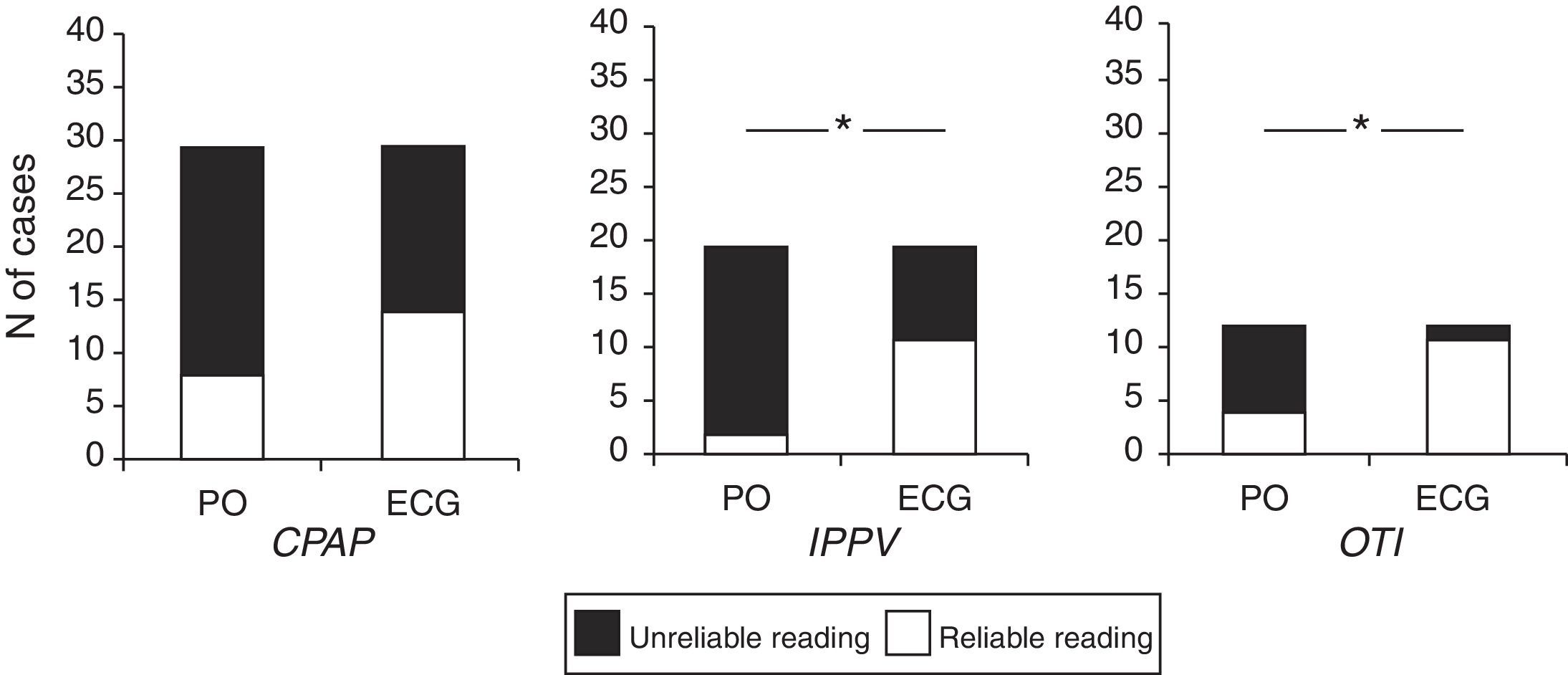
We analysed the period of initial stabilisation, defined by international guidelines as the 30s following birth.1 Heart rate values were not available by either PO or ECG in any patient for this period. The resuscitation period follows stabilisation, and the measures implemented in this period are summarised in Table 1: continuous positive airway pressure (CPAP) was initiated at a mean 109±14.53s after birth, intermittent positive pressure ventilation (IPPV) at 89.37±15.32s, and orotracheal intubation at 161±27.67s. Fig. 1 presents the frequency with which a reliable HR measurement was available at the time each measure was initiated by measurement method. In every case, PO offered a lower percentage of reliable measurements, and this difference was statistically significant for IPPV and orotracheal intubation, and nearly significant for CPAP (P=.08).
Proportion of reliable HR readings by type of device at the time different resuscitation measures were initiated in 39 preterm newborns. CPAP, continuous positive airway pressure; ECG, electrocardiography monitor; HR, heart rate; OTI, orotracheal intubation; PO: pulse oximetry; IPPV, intermittent positive pressure ventilation. *P<.05, Fisher's exact test.
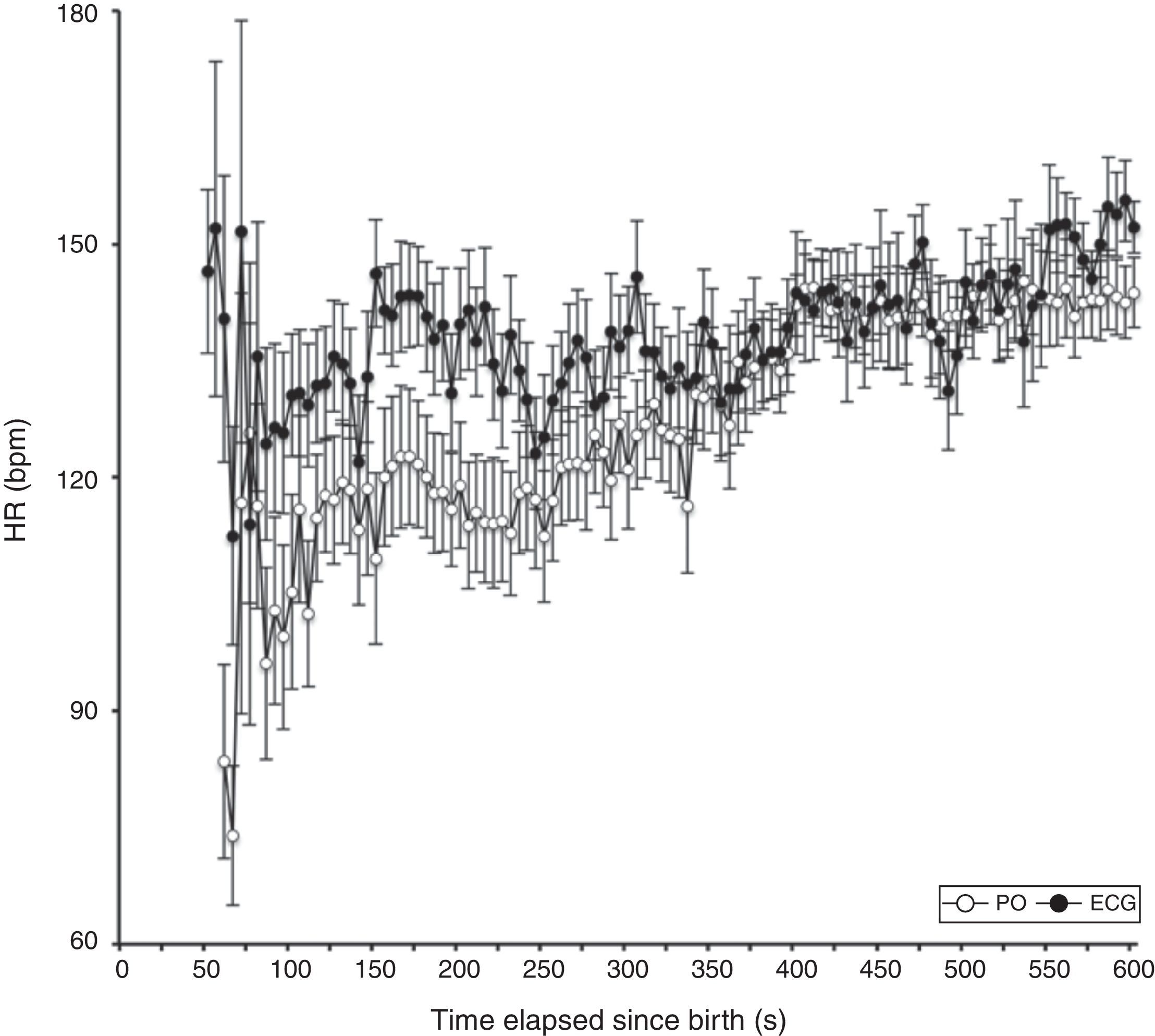
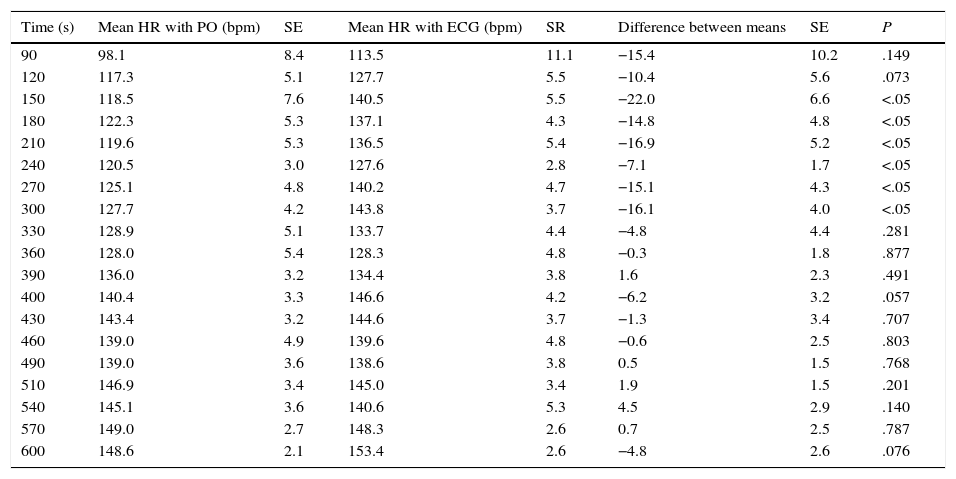
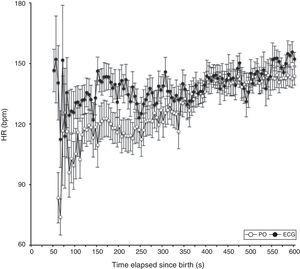
We compared the HR readings obtained by PO and ECG at 5-s intervals. We obtained 1461 valid pairs of data after removing pairs of measurements in which there was signal loss in either device. The mean HR measured by PO was lower than the mean HR measured by ECG in the first 5min of life, and the differences in measurement were statistically significant (P<.05) in the period ranging from 150 to 300s. Past this time, the HR measurements obtained by both methods were similar (Table 3 and Fig. 2).
Comparison of heart rate readings by electrocardiogram and pulse oximeter in the first 10min of life at 30-s intervals.
| Time (s) | Mean HR with PO (bpm) | SE | Mean HR with ECG (bpm) | SR | Difference between means | SE | P |
|---|---|---|---|---|---|---|---|
| 90 | 98.1 | 8.4 | 113.5 | 11.1 | −15.4 | 10.2 | .149 |
| 120 | 117.3 | 5.1 | 127.7 | 5.5 | −10.4 | 5.6 | .073 |
| 150 | 118.5 | 7.6 | 140.5 | 5.5 | −22.0 | 6.6 | <.05 |
| 180 | 122.3 | 5.3 | 137.1 | 4.3 | −14.8 | 4.8 | <.05 |
| 210 | 119.6 | 5.3 | 136.5 | 5.4 | −16.9 | 5.2 | <.05 |
| 240 | 120.5 | 3.0 | 127.6 | 2.8 | −7.1 | 1.7 | <.05 |
| 270 | 125.1 | 4.8 | 140.2 | 4.7 | −15.1 | 4.3 | <.05 |
| 300 | 127.7 | 4.2 | 143.8 | 3.7 | −16.1 | 4.0 | <.05 |
| 330 | 128.9 | 5.1 | 133.7 | 4.4 | −4.8 | 4.4 | .281 |
| 360 | 128.0 | 5.4 | 128.3 | 4.8 | −0.3 | 1.8 | .877 |
| 390 | 136.0 | 3.2 | 134.4 | 3.8 | 1.6 | 2.3 | .491 |
| 400 | 140.4 | 3.3 | 146.6 | 4.2 | −6.2 | 3.2 | .057 |
| 430 | 143.4 | 3.2 | 144.6 | 3.7 | −1.3 | 3.4 | .707 |
| 460 | 139.0 | 4.9 | 139.6 | 4.8 | −0.6 | 2.5 | .803 |
| 490 | 139.0 | 3.6 | 138.6 | 3.8 | 0.5 | 1.5 | .768 |
| 510 | 146.9 | 3.4 | 145.0 | 3.4 | 1.9 | 1.5 | .201 |
| 540 | 145.1 | 3.6 | 140.6 | 5.3 | 4.5 | 2.9 | .140 |
| 570 | 149.0 | 2.7 | 148.3 | 2.6 | 0.7 | 2.5 | .787 |
| 600 | 148.6 | 2.1 | 153.4 | 2.6 | −4.8 | 2.6 | .076 |
ECG, electrocardiogram; SE, standard error; bpm, beats per minute; PO, pulse oximeter.
The results of our study indicate that PO offers reliable and accurate HR measurements significantly later than ECG during reanimation of very preterm or very low birth weight infants. Our findings are consistent with previous data on the shorter delay in obtaining ECG measurements compared to PO during resuscitation of newborns of different gestational ages.6–8 This is a relevant finding, as HR is the most relevant vital parameter in neonatal resuscitation, guiding the initiation and steps taken during resuscitation.1,2 In this sense, we found it striking that in our study, in nearly nine out of ten neonates that received IPPV and nearly three out of four neonates that were intubated or received CPAP, these measures were initiated without a reliable PO-derived HR measurement, proportions that are significantly higher compared to measurements obtained by ECG. This suggests that when it is time to initiate measures as decisive or invasive as intubation or IPPV, if PO is the only method available, such measures will be undertaken based solely on the clinical assessment of the HR, with the limitations already described in the literature.3 We ought to note that as far as we know, our study is the first in which the ECG monitor was hidden from the resuscitation team, so that all therapeutic decisions were based on clinical assessment and PO measurements without the influence of ECG.
The placement of electrodes for ECG was nearly 10s quicker than placement of the PO sensor. Katheria et al.7 also observed this difference, although it was not found in the subset of newborns with weights above 1500g; however, in their study, the time of device placement was calculated from the moment the newborn was placed in the resuscitation platform to the moment the sensors were placed and connected to the devices, and the connection of both devices was made simultaneously in only one patient. In our study, the time of device placement was measured from the moment placement started to the moment it ended for each device. We could argue that placement of the sensor on the hand or wrist of the newborn, with additional time required to then connect the sensor to the PO, is more labour-intensive than adhering 3 electrodes to the chest of the patient. Furthermore, consistent with the results of previous studies,7 we did not observe skin lesions caused by ECG electrodes in any of our patients. The delay in obtaining a reliable HR reading by PO compared to ECG was of nearly 1min. This increased delay is not due to difficulties or poor technique in sensor placement, as the mean time required to obtain reliable PO-derived values in our study was similar to the one described by the manufacturer or those reported in other studies.4,8–10 On the contrary, it is evidence that there is an intrinsic difficulty in the detection of pulse waves by POs in the first minutes of the transition to extrauterine life. Consistent with this, our results showed that PO underestimated HR at the beginning of resuscitation, so that an accurate measurement—that is, one equal to the one obtained by ECG—was not obtained until 5min from birth, with disparities being most pronounced in the first 4min of life. Since this was calculated from the time reliable values could be obtained with both devices, the delay in obtaining a reliable HR value by PO from the moment of birth would be nearly 2min longer (the time required to obtain a reliable measurement with the PO). A previous study conducted on a group of more mature newborns8 found a 450s delay in obtaining an accurate HR measurement by PO, although the largest differences were observed between 60 and 120s after birth. These results suggest that the exclusive use of PO would not only fail to provide a reliable HR reading most of the times that resuscitation measures need to be initiated, but also that during a significant part of the resuscitation period, PO measurements would not be accurate, which could lead to initiation of measures that are not indicated.
We should also discuss the results corresponding to the stabilisation period, that is, the first 30s of life. In our study, reliable HR readings could not be obtained by either method in any of the patients during this period. We must note, however, that following the study protocol, EGG electrodes were not placed on patients until the PO sensor was already in place. Thus, electrode placement did not start until a mean of 26.5s from birth. If we add the 17s needed to complete the adhesion and connection of the electrodes, the total time elapsed amounted exactly to the approximately 43s required to obtain a reliable HR reading by means of ECG. This detail suggests that had the ECG electrodes been placed first, a reliable HR reading would have been available at 18s of life, or, in other words, a reliable and accurate HR would have been available when the stabilisation period ended and resuscitation started.
Another interesting finding was that there was no difference in total time of signal loss by either method. This finding may be biased, however, as due to the study design the resuscitation team was blinded to the ECG signal, but not to the PO signal. Thus, signal losses by incorrect placement or displacement of electrodes often went unnoticed. We could speculate that if the staff had been aware that the signal was absent, the placement of the electrodes would have been corrected earlier and the total time of signal loss would have been reduced. This possibility, and the one presented in the preceding paragraph, should be clarified in a future study designed for that purpose.
There are limitations to this study. First of all, it included few patients, and while we only included neonates born before 32 weeks’ gestational age weighing less than 1500g, the mean gestational age and mean birth weight were relatively high, with a small proportion of extremely immature patients. Another possible limitation is that the quality of the PO signal was assessed by sight, which may have led to the inclusion of incorrect readings or the exclusion of correct readings. However, we also ought to consider that in real practice signal quality is assessed visually when therapeutic decisions based on PO readings are made in the delivery room. Furthermore, studies that assessed the signal quality of PO quantitatively (SIQ>0.30) had results similar to ours.8
Pulse oximetry is a very useful tool that has vastly transformed the care of ill neonates in general, and the approach to resuscitation in particular, especially as it regard the adjustment of the amount of administered oxygen to the requirements of the newborn.11–14 The results of our study, however, suggest that the exclusive use of PO in the delivery room, at least in the first 5min of life, may not suffice to ensure that adjustments adhere to international recommendations, as during this period they rely more heavily on HR than on oxygen saturation. In this sense, measurement of the HR by ECG in the delivery room seems simple, quick, reliable and safe for the patient. Further research is required to support the recommendation of introducing ECG monitoring in the delivery room as an essential tool supplemented by PO for the optimal management of patients.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Iglesias B, Rodríguez MJ, Aleo E, Criado E, Herranz G, Moro M, et al. Pulsioximetría frente al monitor de electrocardiograma para la determinación de la frecuencia cardíaca durante la reanimación del recién nacido pretérmino. An Pediatr (Barc). 2016;84:271–277.
This study was presented at the II Jornadas de Investigación en Medicina Perinatal; September 30, 2014; Madrid, Spain.
This study was also presented at the Pediatric Academic Societies Annual Meeting; April 2015; San Diego, California, United States.