The aim of the study was twofold: a) to determine the prevalence of symptoms of depression and anxiety and sleep disturbances in young patients with vertically-transmitted HIV infection compared to uninfected peers, and b) to identify sociodemographic, psychosocial and medication-related variables and other clinical risk and protective factors related to psychological symptoms.
MethodsWe conducted a cross-sectional study in two groups with independent measures (36 youth with vertically transmitted HIV infection and 39 HIV-negative peers). We used 3 standardised assessment tools and a sociodemographic/psychosocial questionnaire (STAI, BDI, PSQI and adapted sociodemographic test). We performed univariate and multivariable analyses.
ResultsThe univariate analysis did not find significant differences between groups either in psychosocial factors or in the clinical scores. The multivariable analysis found that the presence of psychological symptoms was strongly associated with sociodemographic factors and past events.
ConclusionsPsychosocial factors and the social environment seemed to correlate more strongly to psychological symptoms than HIV status and to explain better the current psychological state of individuals.
Los objetivos principales del estudio fueron dos: a) identificar la prevalencia de síntomas depresivos y de ansiedad y trastornos del sueño en pacientes jóvenes con infección por VIH de transmisión vertical en comparación con un grupo de pares no infectados, y b) identificar factores sociodemográficos, psicosociales y relacionados con la medicación y otros factores de riesgo y protectores relacionados con los síntomas psicológicos.
MétodosEstudio transversal en dos grupos con medidas independientes: 36 sujetos con VIH (transmisión vertical) y 39 sin VIH (no infectados). Se emplearon 3 instrumentos de evaluación estandarizados y un cuestionario sociodemográfico/psicosocial (STAI, BDI, PSQI y test sociodemográfico adaptado). Se realizó análisis univariante y multivariante.
ResultadosEl análisis univariante no reveló diferencias significativas entre los dos grupos en las variables psicosociales o las escalas clínicas. El análisis multivariante encontró que los síntomas psicológicos se asociaban con fuerza a factores sociodemográficos y experiencias del pasado.
ConclusionesEl entorno y las variables psicosociales parecen estar asociados más estrechamente con los síntomas psicológicos que el estado de VIH, y podrían explicar mejor el estado psicológico actual del individuo.
Based on data from the Ministry of Health, there were 571 new cases of HIV in Spain between 2017 and 2018.1 Five of them corresponded to cases of vertical transmission (4 in 2016−17 and 1 in 2017−18). In addition, 10 of these new cases, independently of the mode of transmission, occurred in individuals aged less than 25 years in the 2017−18 period.
Suboptimal adherence to medication regimens and the ensuing progression of disease constitute a multifactorial process that needs to be studied from the vantage points of different fields,2,3 and mental health disorders are among the most important factors to consider.4–7 Furthermore, when it comes to field of mental health, it is well known that adolescence is a critical period characterised by experimentation, risk-taking and self-discovery.8 Decisions concerning relationships, engagement in sexual activity or experimentation with drugs and alcohol are more complex for adolescents with HIV, who need to consider disclosure of their HIV status, the potential for HIV transmission, adverse reactions and adherence to combination antiretroviral therapy (cART) regimens.9,10 The mental health of adolescents with HIV may be affected by the infection, adolescence in general and psychosocial problems generated by the interaction of the disease, adolescence, and the immediate social environment.10
There is currently some consensus among psychologists and clinical researchers that depression, anxiety and adjustment disorder are diagnosed more frequently in infected and exposed subjects, but the current evidence is still contradictory. For instance, Le Prevost et al. found no differences between patients with perinatal HIV infection and HIV-exposed but uninfected individuals in the prevalence of mental disorders, which was similar to normative data.11 However, other studies have found an increased risk and a higher prevalence in HIV-infected individuals compared to individuals not exposed to HIV.6,12,13
Similarly, there has been evidence of a higher prevalence of sleep disorders in HIV-infected individuals for decades14 and of their association with mental disorders.15 Recent studies found significant differences in sleep latency, sleep duration and global sleep quality between HIV+ young adults and healthy controls.16 However, these studies could not attribute these disorders to a single cause, and it is likely that these disturbances result from a complex interaction of psychosocial factors, sleep habits and mental disorders.
The development of mental disorders in HIV patients is associated with multiple factors,17 but some psychosocial variables,17–19 such as the environment where the child develops, seem to explain findings indicative of a higher prevalence in infected and exposed individuals.20,21 Furthermore, in the case of perinatally acquired HIV infection, patients may also deal with the loss of immediate family members, which could carry an increased risk of depression in their lifetimes.22,23 There is also evidence that children orphaned due to AIDS are more likely to exhibit suicidal ideation, depression, problems with their peer relationships, post-traumatic stress disorder and conduct disorders compared to children orphaned due to other causes and non-orphaned children.24 Finally, although based on small sample sizes, some studies suggest that attention-deficit hyperactivity disorder, anxiety and depression are all highly prevalent in HIV-infected children.25–27
Consequently, mental health must become an urgent priority in the fight against HIV and, as a primary objective, we screened for the presence of psychological symptoms with highly accurate tools and analysed associated risk factors in Spanish patients with vertically transmitted HIV infection, comparing the results to the reference population. Thus, the aim of our study was twofold: a) to determine the prevalence of symptoms of depression, anxiety and disturbed sleep in vertically infected HIV patients included in the Paediatric Cohort of the Spanish AIDS Research Network (CoRISpe) and non-infected peers of the same age and sociodemographic background; and b) to assess the influence of sociodemographic, psychosocial and medication-related factors and other risk and protective factors related to psychological symptoms.
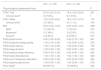
MethodsStudy design and sampleWe conducted a cross-sectional study in two groups and collected independent measures between January 2016 and January 2017. We recruited 75 participants that resided in Spain managed in Spanish public hospitals and included in the CoRISpe cohort or the cohort of paediatric patients with HIV transferred to adult care (FARO project). Thirty-six were HIV-positive (HIV+) vertically infected subjects managed in outpatient paediatric and adult infectious disease units. We selected patients without current comorbidities, cognitive impairment or psychiatric diagnoses. Most patients had virological and immunological markers of controlled infection at the time of the evaluation and had been receiving cART for a median of 15.7 years. Fifteen patients (41.7%) met the criteria for clinical category C in the classification of the Centers for Disease Control and Prevention (CDC), while 29 (80.6%) had an undetectable viral load at the time of data collection (see Table 1).
Clinical features of participants with perinatal HIV infection.
| Immunovirological variables | |
|---|---|
| CDC clinical category (n, %) | |
| A | 13 (36.1%) |
| B | 8 (22.2%) |
| C | 15 (41.7%) |
| CD4 count (cells/mm3), median (IQR) | 706.5 (469.5−900.7) |
| CD4 percentage, median (IQR) | 35.2% (31%–41.7%) |
| CD4 count nadir (cells/mm3), median (IQR) | 206 (52.5−313.7) |
| CD4 percentage nadir, median (IQR) | 13.1% (6.25%–21.6%) |
| CD4/CD8 | 0.96 (0.66−1.3) |
| AIDS | 15 (41.7%) |
| Encephalopathy | 5 (13.9%) |
| HCV | 0 |
| Antiretroviral therapy | |
|---|---|
| Median age at HIV diagnosis (years) | 0.76 (0.2−4.2) |
| Median age at initiation of ART (years) | 1.3 (0.3−5.3) |
| Median age at initiation of cART (years) | 2.3 (1−6.6) |
| Duration of ART (years) | 16.9 (13.9−19.6) |
| Duration of cART (years) | 15.7 (13.9−18.8) |
| VL in patients with detectable VL (copies/mL), median (IQR) | 537 (190−49026) |
| Patients with undetectable VL (<50 copies/mL) | 29/36 (80.5%) |
| Years with undetectable VL, median (IQR) | |
| Type of HAART | 9.8 (6.8−12.4) |
| PI | 16 (44.4%) |
| INI | 4 (11.1%) |
| NNRTI | 8 (22.2%) |
| Others | 7 (19.4%) |
ART, antiretroviral therapy; cART, combined antiretroviral therapy; HAART, highly active antiretroviral therapy; HCV, hepatitis C virus; IQR, interquartile range; INI, integrase inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; PI, protease inhibitor; VL, viral load.
We recruited a control group of HIV negative (HIV–) individuals (n = 39) by accidental sampling through the snowball method. We matched HIV+ participants and controls for sex, age, years of education and socioeconomic status (SES). The inclusion criteria for the control group were absence of HIV infection in the individual or a close relative, and absence of any other disease or cognitive disorder or impairment.
The study was approved by the ethics committee of participating hospitals. We obtained informed consent from all the participants.
AssessmentWe used 3 standardised assessment tools and a sociodemographic/psychosocial questionnaire:
- •
State-Trait Anxiety Inventory (STAI).28 Questionnaire that evaluates the current level of anxiety (state) and the predisposition of the person to react to stress with anxiety (trait). The possible score of each subscale ranges from 0 to 60 points. We also analysed the scores relative to the cut-off point,29 set at 35 points.
- •
Beck Depression Inventory (BDI).30 A 21-item self-report instrument designed to assess the severity of depressive symptoms. The possible score ranges from 0 to 63 points. We also analysed the scores relative to cut-off points30 used to define different ranges of severity (0–9, no depression; 10–18, mild depression; 19–29, moderate depression; 30–63, severe depression).
- •
Pittsburgh Sleep Quality Index (PSQI).31 Self-administered questionnaire that evaluates the quality of sleep and changes in sleep over a one-month interval, offering seven component scores and a global score. The seven components are subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction. The global score ranges from 0 to 21. We also analysed scores relative to the cut-off point,31 set at 5 points.
- •
A sociodemographic and psychosocial semi-structured self-report questionnaire, used by our group in previous works32,33 and created specifically for this project to collect data on sociodemographic characteristics, clinical manifestations, academic performance and lifestyle habits (substance use and physical activity). We used the International Standard Classification of Education (ISCED)34 to categorize the educational attainment of participants. We defined current psychological distress as a subjective experience of unpleasant feelings or emotions with an impact on daily functioning. Some examples of situations that can elicit distress are moving to a new city, transfer to a different school/starting a new job, exams, job dissatisfaction, experiencing a breakup or being in an unstable relationship. We used the term traumatic event to refer to personally experiencing a life-threatening situation or witnessing a loved one in such a situation, but without subsequent development of post-traumatic stress disorder. Some examples are neglect, emotional or sexual abuse, bullying, divorce or bereavement. Although these terms could be confused with specific definitions used in the field of psychology by specialised readers, we decided to use words that are common in everyday language rather than more complex terms that could be misinterpreted by participants and hinder comprehension. These terms do not fit any official standard classification and are mere descriptors of subjective emotional experiences in individuals, and are the same terms used in the questionnaire given to participants.
We summarised data on factors associated with HIV infection using the median and interquartile range (IQR) in case of continuous variables and absolute and relative frequencies in case of categorical variables. We compared continuous data with the Mann-Whitney U test and frequencies with the Fisher exact test. The normality of the distribution was assessed by means of the Shapiro-Wilk test. We fitted univariate and multivariate Poisson regression models to analyse the association between the BDI score, HIV infection and psychosocial factors, and to analyse the association between the PSQI score, HIV infection and psychosocial factors. We included variables in the multivariate model using stepwise selection with the Akaike information criterion (AIC). The statistical analysis was performed with the software R.35
ResultsWe recruited 36 HIV+ youth (mean age, 19.92 ± 3.17 years; 55.6% female; 69.7% white) and 39 HIV– youths matched for sex, age, educational attainment and income bracket (mean age, 20.26 ± 2.73 years; 61.5% female; 55.9% white). The most frequent annual household income bracket in both groups was the 12,000–20,000 euro bracket. We did not find differences between groups in the economic difficulties reported by participants, with difficulties reported by 40%–50% of participants in each group. Most participants in both groups had an educational attainment categorised as “low” (71.4% in each group), although grade retention was significantly most frequent in the HIV+ group (P = .01) (Table 2).
Sociodemographic and psychosocial characteristics.
| HIV+ (n = 36) | HIV- (n = 39) | P* | |
|---|---|---|---|
| Age (years) | 19.92 ± 3.175 | 20.26 ± 2.73 | .62 |
| Female sex | 20 (55.6%) | 24 (61.5%) | .59 |
| Caucasian | 23 (69.7%) | 19 (55.9%) | .01 |
| Annual household income | .6 | ||
| <12,000 | 8 (25.8%) | 9 (30%) | |
| 12,000−20,000 | 13 (41.9%) | 16 (53.3%) | |
| 20,000−30,000 | 8 (25.8%) | 4 (13.3%) | |
| >30,000 | 2 (6.5%) | 1 (3.3%) | |
| Self-reported economic difficulties | 14 (41.2%) | 17 (50%) | .46 |
| Highest level of education attained** | .6 | ||
| Low | 25 (71.4%) | 25 (71.4%) | |
| Medium | 8 (22.9%) | 6 (17.1%) | |
| High | 2 (5.7%) | 4 (11.4%) | |
| Repeated grades | 32 (94.1%) | 25 (71.4%) | .01 |
| Experienced a traumatic event | .22 | ||
| No | 18 (51.4%) | 23 (65.7%) | |
| Yes | 17 (48.6%) | 12 (34.3%) | |
| Psychological distress | .13 | ||
| No | 10 (28.65%) | 16 (45.7%) | |
| Yes | 25 (71.4%) | 19 (54.3%) | |
| Other medical diagnoses- no HIV (in life time) | 8 (24.2%) | 4 (11.4%) | .16 |
| Other psychological disorders (in life time) | 3 (8.6%) | 5 (14.3%) | .7 |
| Physical exercise | .65 | ||
| No | 17 (51.5%) | 14 (41.2%) | |
| 1–3 days | 9 (27.3%) | 10 (29.4%) | |
| 4–7 days | 7 (21.2%) | 10 (29.4%) | |
| Alcohol*** | 20 (58.8%) | 26 (74.3%) | .17 |
| Tobacco*** | 11 (31.4%) | 14 (40%) | .45 |
| Other drugs*** | 4 (11.8%) | 7 (20.6%) | .32 |
Nearly half of the participants reported experiencing traumatic events (48.6% in the HIV+ group vs 34.3% in the HIV– group) and more than half reported current psychological distress (71.4% in HIV+ group vs 54.3% in HIV– group). We did not find differences during the follow-up in terms of medical and psychiatric diagnoses, physical activity and substance use. Nearly 59% of HIV+ participants and 74.3% of HIV–reported habitual consumption of alcohol.
The comparison of the STAI, BDI and PSQI total and component scores in the groups under study did not reveal significant differences except in the duration of sleep, for which scores were lower in the HIV+ group (Table 3). When considering the cut-off criteria,29–31 the results were similar between the groups. We found depressive symptoms in 33.3% of the HIV+ group (severe in 5.6%) compared to 47.4% of the HIV– group (severe in 5.3%), poor sleep quality in 52.8% of the HIV+ group versus 66.7% of the HIV– group, and a a lower prevalence of anxiety in both groups (HIV+ vs HIV–: STAI-T, 13.9% vs 15.8%; STAI-S: 11.1% vs 7.7%) (Table 3).
Psychological testing outcomes.
| HIV– (n = 39) | HIV+ (n = 36) | ||
|---|---|---|---|
| Psychological assessment tools | P | ||
| STAI- Trait | 21.0 (13.2−31.0) | 19.0 (12.5−30.0) | .837 |
| Clinical levela | 6 (15.8%) | 5 (13.9%) | 1 |
| STAI- State | 13.0 (9.00−22.5) | 16.5 (10.0−27.0) | .172 |
| Clinical levela | 3 (7.69%) | 4 (11.1%) | .704 |
| BDI | 8.00 (5.00−12.8) | 6.00 (2.00−12.0) | .298 |
| Milda | 13 (34.2%) | 7 (19.4%) | .512 |
| Moderatea | 3 (7.89%) | 3 (8.33%) | .512 |
| Severea | 2 (5.26%) | 2 (5.56%) | .512 |
| PSQI global score | 6.00 (3.50−8.50) | 5.00 (2.75−7.00) | .097 |
| PSQI subjective sleep quality | 1.00 (1.00−2.00) | 1.00 (0.00−2.00) | .225 |
| PSQI sleep latency | 1.00 (1.00−2.00) | 1.00 (0.00−2.00) | .156 |
| PSQI sleep duration | 1.00 (0.00−1.00) | 0.00 (0.00−1.00) | .030 |
| PSQI habitual sleep efficiency | 0.00 (0.00−1.00) | 0.00 (0.00−1.00) | .695 |
| PSQI sleep disturbances | 1.00 (1.00−1.00) | 1.00 (1.00−1.00) | .482 |
| PSQI use of sleeping medication | 0.00 (0.00−0.00) | 0.00 (0.00−0.00) | .484 |
| PSQI daytime dysfunction | 1.00 (0.00−1.00) | 1.00 (0.00−1.00) | .378 |
| Poor sleepa | 26 (66.7%) | 19 (52.8%) | .322 |
Values expressed as median (interquartile range) or n (%).
As can be seen in Table 4, the regression models showed depression scores 20% lower in HIV+ patients compared to HIV– participants independently of the psychosocial profile. Patients with anxiety had depression scores that were 5% greater compared to the scores of patients with low anxiety scores, adjusting for HIV infection and other psychosocial factors in the model. In addition, the risk of having a high depression score was lower in patients with a high household income. Patients that had experienced traumatic events or had a mental health diagnosis had a 2-fold risk of experiencing depression compared to the rest of the patients (Table 4).
Association of depression with HIV infection and psychosocial variables.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Exp (β), 95% CI, P | Exp (β), 95% CI, P | |||
| HIV+ | 0.87 [0.74−1.06] | .062 | 0.79 [0.66−0.94] | .008 |
| Household income | ||||
| Reference <12,000 | ||||
| 12,000−20,000 | 0.92 [0.75−1.13] | .435 | ||
| 20,000−30,000 | 0.63 [0.46−0.86] | .004 | ||
| >30,000 | 0.47 [0.27−0.79] | .007 | ||
| Traumatic event | 1.91 [1.6−2.29] | <.001 | ||
| Current stress | 0.81 [0.67−0.99] | .036 | ||
| Mental health diagnosis | 1.75 [1.38−2.22] | <.001 | ||
| Anxiety | 1.05 [1.04−1.06] | <.001 | ||
We assessed the interactions between psychosocial factors and HIV infection in the model and identified no significant interaction terms.
The results presented in Table 5 show that HIV infection did not have a significant effect on total sleep in the univariate or multivariable analysis adjusting for household income, history of traumatic events and the interaction between traumatic event and HIV infection. Participants that had experienced traumatic events exhibited a 55% increase in the risk of having low quality sleep, although in this sample, the presence of HIV infection reduced this effect by 38% (Table 5).
Association of sleep with HIV infection and psychosocial variables.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Exp (β), 95% CI, P | Exp (β), 95% CI, P | |||
| HIV+ | 0.29 [0.06−1.32] | .150 | 1.04 [0.76−1.41] | .801 |
| Household income | ||||
| Reference <12,000 | ||||
| 12,000−20,000 | 0.93 [0.73−1.22] | .630 | ||
| 20,000−30,000 | 0.72 [0.51−1.02] | .071 | ||
| >30,000 | 1.18 [0.71−1.90] | .492 | ||
| Traumatic event | 1.55 [1.15−2.09] | .004 | ||
| Interaction traumatic event and HIV+ | 0.62 [0.4−0.97] | .037 | ||
HIV– individuals had higher PSQI scores (poorer sleep quality) if they had experienced a traumatic event. However, we did not observe this effect in HIV+ individuals.
In the HIV+ group, there was no significant association between medical variables, the STAI score and the PSQI score (P > .05). While we found a positive association between the BDI score and viral load (Pearson correlation coefficient, 0.38; P = .02), this correlation did not persist in the outcomes of the model with stepwise inclusion of variables or the multivariate regression analysis.
DiscussionThe main objective of our study was to identify symptoms of anxiety and depression and assess sleep quality in individuals with perinatal HIV infection in the CoRISpe cohort. We found that 33.3% of HIV+ individuals had depressive symptoms of varying severity based on the established thresholds30 and 52.8% had poor sleep quality.
As for anxiety, based on the criteria used to identify associated features,36 13.9% of individuals had high scores for trait anxiety, and 11.1% for state anxiety.
When it comes to establishing a framework to analyse these results, it is difficult to identify a widely used reference to compare the proportions found in our study due to the considerable variability in the literature. We can present several comparisons to illustrate this issue. For example, our findings were consistent with those described by Scharko et al.,26 who reviewed the prevalence of mental health disorders in paediatric patients with HIV/AIDS. They reported an average prevalence of anxiety disorder of 24.3% and a prevalence of depression of 25%, corresponding to risk ratios of 3.8 and 7.1, respectively. These percentages were higher compared to those reported by other authors, such as LePrevost et al.,11 who found percentages of 15% for anxiety/depression, and more similar to those reported by Mendoza et al.,36 who found a prevalence of depression of 30% in patients with HIV infection. Other studies have found mental health disorders in 50%36 or 53%7 of individuals with HIV infection.
The considerable heterogeneity of the previous literature motivated the secondary objective of our study. In order to contribute additional information on this matter, we decided to fit a multivariate model (Table 4), which showed that psychosocial factors had the same effect in both the HIV+ and HIV– groups. We found that depression was strongly associated with traumatic events, the presence of other mental health disorders and anxiety scores.
Otherwise, the multivariate analysis showed that HIV infection had a protective effect (Table 4), although this effect has not been described in the reviewed literature. Nevertheless, there is another possible explanation to the effect observed in our sample: the regular contact with health care services of HIV+ patients in Spain. This variable is associated with the HIV+ status and could have a protective effect by allowing access to specialised care more frequently and faster. This highlights the need to develop larger and more precise studies that include enough variables and greater power to determine their effect to further investigate this contradictory outcome.
In another aspect comprehended in the same objective, the frequency of sleep disturbances in HIV+ individuals, we found results that were similar to the mental health results. We did not find statistically differences in either the total score or any of the component scores, except in sleep duration. This result diverged from those of other authors that have found differences in sleep quality between individuals with and without HIV infection.16 A different study carried out in the CoRISpe cohort found sleep disturbances in up to 76% of patients with HIV.37 However, most studies have not controlled for all the factors that could be at play in this outcome, and therefore it is difficult to establish with certainty the role of HIV infection or of any of the other factors (sleep habits, emotional circumstances…) in the final outcomes.
ConclusionIn conclusion, our study established the prevalence of psychological symptoms in a representative sample of young adults with vertically transmitted HIV infection. The findings did not evince significant differences between the HIV+ and HIV– groups in trait or state anxiety scores, total score in the depression scale or total or component scores in the sleep quality scale, except for sleep duration.
These results contrast with previous studies that have found clear differences between individuals with HIV infection versus individuals without exposure to HIV,6,12,13 but are consistent with the findings of other studies that analysed environmental variables and determined that the HIV status in and of itself is not a determinant for the development of mental health disorders.11,17–19 In agreement with the authors of the latter, we believe that it is the environment of the individual that acts as a protector or a trigger through different factors.
We applied stringent matching criteria in our sample, as in addition to sex and age, we took into account educational attainment and household annual income (most participants were in the 12,000–20,000 euro bracket), which allowed us to study comparable groups, facilitating an analysis of psychological disorders in the context of a similar social environment.
Previous studies that analysed the psychosocial context of individuals have even found that the prevalence of symptoms does not differ between individuals with HIV infection and individuals that have been exposed but not infected, leading to the conclusion that symptoms could be attributed directly to environmental factors.20,21 A meta-analysis published by Ciesla38 reached similar conclusions, for while it found a frequency of depression that was more than double in HIV+ individuals compared to HIV– individuals, the findings suggested that HIV infection was not directly associated with the development of depressive disorders. This supports the lack of observed differences between groups in our study, as both groups were comparable in terms of a large set of factors, such as age, sex, educational attainment and socioeconomic status (with most of the sample conspicuously in the in medium-low range compared to the general population of Spain), current stress and past trauma.
In support of this conclusion, the individuals included in both groups of our study were also very similar in other psychosocial aspects, such as presence of medical or psychiatric comorbidity, economic difficulties and days of physical activity per week, factors that have been found to be related to mood.39 We did not find significant differences between the groups, except in being held back a year in school, which was more frequent in the HIV+ group (94.1% compared to 71.4% in the HIV– group). We did not find differences in the use of alcohol, tobacco or other drugs that have also been found to be associated with depression, anxiety and sleep disorders in other studies.40 In fact, the results obtained for these variables did not differ from reference data for the general population in Spain.41
We ought to mention that most individuals in our sample had reported a low socioeconomic status and experiencing stressful situations. In addition, substance use was frequent in both groups. These characteristics may have had an impact on the results we found in our sample.
The discussion of the importance of the psychosocial environment on the presence of symptoms of depression or anxiety is not new in psychology. Rigorous evidence has been published in the past, including the systematic review by Lyubomirsky, King and Diener (not specifically in the HIV+ population).42 Their findings support the importance of the social environment as one of the factors most strongly correlated to emotional state identified to date. In addition, a study by Nöthling et al.37 reported significant covariation between the psychological disorders in HIV+ mothers with psychological disorders in children, and between alcohol abuse in mothers and behavioural problems in children. Other studies on individuals living with HIV corroborate the importance of a wide range of factors in the development of risk behaviours43,44 and mental disorders,17 specifically the environment where children develop,17–19 which has been identified as a relevant factor in the increased prevalence observed in infected or exposed individuals.20
Lastly, when it came to the impact of factors related to the disease, we ought to highlight that most of our patients had low and stable levels of viraemia. In this regard, although we found an initial association between viral load and the BDI score, the association was not confirmed on further analysis. Nevertheless, the fact that few patients had a detectable viral load may have affected these results.
Hence, based on the results of our study and the previous literature, it is reasonable to conclude that psychological symptoms are probably correlated to psychosocial factors, possibly more strongly than to medical conditions.
Furthermore, the high prevalence of psychological symptoms found in the study highlights the need of addressing them in everyday clinical practice, offering psychological support to these patients.
LimitationsAmong the limitations of the study, first, there is the smaller than expected sample size that resulted from the strict matching procedure, and which may have affected the results due to the low frequency of different factors such as substance use, which required clustering variables. This limits the ability to draw conclusions from the current results, but we chose this alternative due to the importance of peers in psychosocial factors, which were the variables in relation to which we chose to compare the presence of psychological symptoms.
Another limitation of the study was the lack of a standardised questionnaire for the assessment of psychosocial factors and quality of life, which would have improved the quality of the obtained data.
Future researchTo improve our knowledge of multifactorial variables associated with mental health in HIV+ patients in the Spanish population, it is important to continue conducting comprehensive studies that analyse several areas and to increase the sample size.
FundingThis work was funded by the Instituto de Salud Carlos III (FIS 15/00694) with co-funding by the European Regional Development Fund (ERDF): “Una manera de hacer Europa” and the Fundacion para la Investigación y Prevención de SIDA en Espana (FIPSE) (24691/07, 3608229/09, 240800/09, 361910/10 and 36-0910-1). The CorispeS cohort is integrated the Red Española de Investigación del SIDA (Spanish AIDS Research Network, RIS) (RD16/0025/0017-ISCIII-FEDER, RD16/0025/0019-ISCIII-FEDER, RD16/0025/0024-ISCIII-FEDER and RIS EPICLIN-12/2012). CV has received a grant from the Government of the Community of Madrid, funded from the ERDF (grants for hiring research assistants and laboratory technicians//Order 2524/2016, of 1 August, BOCM no. 188 of August 8, 2016).
Conflicts of interestThe authors have no conflicts of interest to declare.
This study would not have been possible without the collaboration of all the patients, medical and nursing staff, and data managers who have participated in the project. We also thank all the members of NeuroCoRISpe project and CoRISpe cohort (Paediatric HIV National Network).
Please cite this article as: Velo Higueras C, García MM-B, Domínguez-Rodríguez S, Ruiz Sáez B, Cuéllar-Flores I, García-Navarro C, et al. Prevalencia y factores de riesgo de síntomas psicológicos en una muestra española de jóvenes con VIH en comparación con pares no infectados. An Pediatr (Barc). 2022;96:203–212.