Breastfeeding has important benefits for population health. The aims of this study are: (i) to determine the prevalence and duration of breastfeeding and exclusive breastfeeding; (ii) analyse the reasons for not starting or abandoning of breastfeeding, and (iii) describe the factors associated with the initiation and duration of exclusive breastfeeding.
Material and methodsCross sectional study using the baseline data of the ELOIN cohort, obtained using an epidemiological questionnaire. A sample of 2627 children born in 2008–2009 from the Community of Madrid was studied. Logistic regression models were used.
ResultsPrevalence of exclusive breastfeeding and breastfeeding was 77.6% and 88% respectively; prevalence of exclusive breastfeeding at 6 months 25.4%, and prevalence of breastfeeding at 2 years was 7.7%. The most common reasons for abandoning breastfeeding were insufficient milk (36%), and incorporation to work (25.9%). The variables associated with starting or maintaining of exclusive breastfeeding were: mother older than 35 years, medium-high economic status, foreigner residing in Spain less than 10 years, and having participated in a breastfeeding workshop.
ConclusionsBreastfeeding prevalence in the Community of Madrid did not reach the international recommendations in 2008–2009. It is necessary to intensify strategies for breastfeeding promotion, protection, and support, including their periodic monitoring.
La lactancia materna tiene importantes beneficios para la salud poblacional. Los objetivos de este estudio son: a)conocer la prevalencia y duración de la lactancia materna y lactancia materna exclusiva; b)analizar las razones de no inicio y de abandono de la lactancia materna, y c)describir los factores asociados a la lactancia materna exclusiva y con su mantenimiento durante 6meses.
Material y métodosEstudio transversal a partir de datos basales de la cohorte ELOIN, obtenidos por cuestionario epidemiológico. Se estudió una muestra de 2.627 niños de 4años nacidos en 2008-2009 de la Comunidad de Madrid. Se utilizaron modelos de regresión logística.
ResultadosLa prevalencia de lactancia materna exclusiva y lactancia materna fue del 77,6 y del 88%, respectivamente; la lactancia materna exclusiva a los 6meses fue del 25,4%, y la lactancia materna a los 2años, del 7,7%. Las razones principales de finalización de la lactancia fueron la producción insuficiente de leche (36%) y la incorporación al trabajo (25,9%). Las variables asociadas con el inicio o mantenimiento de la lactancia materna exclusiva fueron: madre de más de 35años, estatus económico medio-alto, extranjera con menos de 10años de residencia en España y haber participado en taller de lactancia tras el parto.
ConclusionesLa prevalencia de lactancia materna en la Comunidad de Madrid no alcanzó en 2008-2009 las recomendaciones internacionales. Es necesario intensificar estrategias de promoción, protección y apoyo a la lactancia materna, incluyendo su monitorización periódica.
Human milk is the natural and optimal food for infants in the first 6 months of life, as it provides all the necessary nutrients for their growth and development. In addition, breastfeeding (BF) promotes mother–child bonding, is associated with a decreased risk of infection and disease during childhood (asthma, dermatitis, obesity or diabetes) and with higher IQ scores, and, in the mother, with a reduced risk of breast and ovary cancer and of type 2 diabetes.1–3 The WHO, health care authorities and scientific societies in Spain and abroad recommend exclusive breastfeeding (EBF) in the first 6 months of life and continued breastfeeding combined with complementary foods until at least age 2 years.4–6
The literature describes numerous factors associated with not initiating EBF or with discontinuing it before age 6 months: lower maternal age, low socioeconomic status and educational attainment, unsupportive work environment, inadequate care during birth and in the postnatal period, low birth weight, perceived insufficient milk supply, previous negative experiences with BF or attitudes regarding EBF before birth, among others.7–9
Despite the risks associated with artificial formula feeding or early discontinuation of EBF and the decades-long efforts made by several countries to protect, promote and support EBF, its prevalence remains low worldwide. In 2010, the prevalence of EBF in the first 6 months of life was 39% in developing countries.10 In Spain, based on the 2006 Encuesta Nacional de Salud de España (National Health Survey of Spain [ENSE]), the percentage of infants that were exclusively or partially breastfed at 6 months was 38.8%, a proportion that had increased to 46.9% in 2011.11 The global target for year 2025 is to increase the rate of EBF in the first 6 months of life to at least 50%.12 To this end, in 2009 the Consejería de Sanidad (Department of Health) of the Community of Madrid, through the Madrid Public Health System, signed a collaboration agreement with UNICEF to improve health care practices and promote satisfactory BF in the region.13 Since then, the prevalence of BF and associated factors have been analysed in non-representative samples of the population of the Community of Madrid.14
The goals of this study were: (a) to determine the prevalence and duration of BF and EBF; (b) to analyse the reasons for not initiating and for discontinuing BF, and (c) to describe the factors associated to EBF and its maintenance for 6 months, with all of the above applying to the population of the Community of Madrid.
Materials and methodsDesignWe conducted a cross-sectional study by reviewing the baseline data of the Estudio Longitudinal de Obesidad Infantil (Longitudinal Study of Childhood Obesity [ELOIN]).15 The ELOIN is a population-based cohort study whose objectives are to describe variations in childhood overweight and obesity, establish their association with sociodemographic factors and estimate their impact on health. An email was sent to the parents of the selected children informing them of the study and requesting their participation, and participants whose parents agreed to it were enrolled with the signing of an informed consent form. The baseline data were collected between January 2012 and December 2013 by means of a physical examination conducted by paediatricians employed in primary care centres and an ad hoc epidemiological questionnaire on diet and lifestyle habits that was administered by phone to the adults in charge of the participants (mothers and/or fathers).
Study sampleThe ELOIN cohort comprises a representative sample (n=4571) of the population born in 2008–2009 residing in the Community of Madrid included in the caseloads of the 31 paediatricians of the Primary Care Sentinel Physician Network16 and selected though multistage sampling. For our study, we selected the ELOIN participants that had completed the epidemiological questionnaire (n=2627).
VariablesSociodemographic: sex of participant; maternal age at birth (<20 years/20–35 years/>35 years); duration in years of mother's residence in Spain (Spanish mother/≥10 years/<10 years); maternal educational attainment (elementary education or less/secondary education/university); social class of family (I/II/III/IV/V/never employed); socioeconomic status of family (low/middle/high).
The variable “duration in years of mother's residence in Spain” included every mother; the ≥10 years and <10 years categories applied to mothers that were not born in Spain. Maternal educational attainment was defined as the highest education level achieved by the mother at the time of administration of the epidemiological questionnaire. The social class of the family was determined based on the highest-level occupation in the household, as proposed by the Sociedad Española de Epidemiología (Spanish Society of Epidemiology), and comprised 5 categories, of which social class I was the most privileged.17 We defined family socioeconomic status (SES) based on the Family Affluence Scale (FAS),18 with a score of 0–2 points corresponding to low SES, a score of 3–5 to middle SES and a score of 6 points 9 to high SES.
Breastfeeding: BF (yes/no), duration of BF (months), EBF (yes/no), duration of EBF (months), participation in BF workshop after delivery (yes/no), main reason for not initiating BF, main reason for discontinuing BF.
We used the definitions of the WHO: BF refers to the infant receiving breast milk, possibly combined with artificial formula or other foods; EBF refers to the infant being fed breast milk only, allowing for administration of vitamin or mineral supplements or medicines.19 Participation in the BF workshop was voluntary and limited to mothers that intended to breastfeed. The variable “main reason for not initiating BF” comprised 7 categories: (1) mother's choice; (2) difficulty establishing BF; (3) maternal health problems; (4) infant health problems; (5) infant was adopted; (6) return to work and (7) recommendation of health professional. The variable “main reason for discontinuing BF” comprised 9 categories: (1) insufficient milk supply; (2) return to work; (3) mother's choice; (4) child self-weaning; (5) breast problems; (6) maternal health problems; (7) child health problems; (8) new pregnancy and (9) advice/recommendation of health professional (Appendix A).
Data collectionWe obtained all the data for this study from one section of the epidemiological questionnaire used in the ELOIN study (Appendix A). When it came to BF, this questionnaire used an adaptation of items 64–69 in the Questionnaire on Minors of the 2011–2012 ENSE health survey20 in addition to items of our own making with multiple-choice answers regarding the reasons to not initiate or to discontinue BF that we developed after consulting with paediatricians expert in the subject.
The study protocol was approved by the Clinical Research Ethics Committee of the Hospital Universitario Ramón y Cajal of Madrid.
Statistical analysisWe performed a descriptive analysis of the variables. We have expressed qualitative variables as frequency distributions. We calculated the prevalence of BF and EBF and their duration through age 12 months and performed an inferential analysis with calculation of 95% confident intervals (CIs). We analysed variables associated with EBF and its maintenance for 6 months using the chi square test and included associations with p-values of 0.10 or less in the multivariate logistic regression analysis. In fitting the final regression model, we considered variables with p-values of 0.05 or less statistically significant. We performed the analyses with the statistical packages SPSS version 15.0 (SPSS Inc; Chicago, IL, United States) and STATA version 13.0 (StataCorp; College Station, TX, United States).
ResultsOf the 2627 completed epidemiological questionnaire, 87% had been administered to mothers. The mean maternal age at birth was 32.5 years (SD, 5.1). Table 1 summarises the rest of the sample characteristics.
Sample characteristics (sample of the population born in 2008–2009 in the Community of Madrid, ELOIN 2012–2013 study).
| n | % | |
|---|---|---|
| Sex of participant | ||
| Male | 1334 | 50.8 |
| Female | 1293 | 49.2 |
| Maternal age at birth | ||
| <20 years | 51 | 1.9 |
| 20–35 years | 1825 | 69.5 |
| >35 years | 718 | 27.3 |
| Not documented | 33 | 1.3 |
| Maternal country of birth | ||
| Spain | 1940 | 73.9 |
| Other than Spain | 628 | 23.9 |
| Not documented | 59 | 2.2 |
| Duration of mother's residence in Spain, years | ||
| Spanish mother | 1940 | 73.9 |
| Foreign-born mother, residence ≥10 years | 358 | 13.6 |
| Foreign-born mother, residence <10 years | 263 | 10.0 |
| Not documented | 66 | 2.5 |
| Maternal educational attainment | ||
| Elementary education or less | 93 | 3.5 |
| High school | 1431 | 54.5 |
| University | 1099 | 41.8 |
| Unknown/Not answered | 4 | 0.2 |
| Social class of family | ||
| I | 503 | 19.1 |
| II | 481 | 18.3 |
| III | 510 | 19.4 |
| IV | 866 | 33.0 |
| V | 234 | 8.9 |
| Never employed | 19 | 0.7 |
| Not documented | 14 | 0.5 |
| Family socioeconomic status | ||
| Low | 488 | 18.6 |
| Middle | 803 | 30.6 |
| High | 1333 | 50.7 |
| Not documented | 3 | 0.1 |
| Participation in breastfeeding workshop after delivery (n=2313) | ||
| Yes | 251 | 10.9 |
| No | 1987 | 85.9 |
| Not documented | 75 | 3.2 |
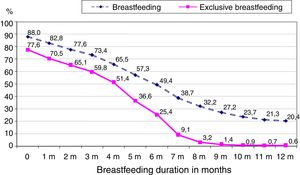
The number of mothers that established BF or EBF at some point were 2313 and 2039, respectively, corresponding to an 88% prevalence of BF (95% CI, 86.4–89.2%) and a 77.6% prevalence of EBF (95% CI, 76.0–79.2%). Both percentages decreased with duration of BF, and by 6 months of age were down to 49.4% (95% CI, 47.7–51.1%) for BF and 25.4% (95% CI, 23.7–27.1%) for EBF. Fig. 1 shows the prevalence of BF and of EBF by months of BF duration.
The 12% of mothers that did not initiate BF reported the reasons for this outcome (Table 2). The 3 most frequent reasons were maternal choice (29% of cases), difficulties establishing BF (28.6%) and maternal health problems (27.3%).
Main reasons to not initiate breastfeeding (mothers in the sample of the 2012–2013 ELOIN study).
| Reported reasons | n | % |
|---|---|---|
| Mother's choice | ||
| “I did not want to breastfeed” or “The idea of breastfeeding was unpleasant” | 73 | 23.5 |
| “Bottle feeding was easier/more convenient” | 8 | 2.6 |
| “I consider artificial formula as healthy/adequate as breast milk” | 2 | 0.6 |
| “Personal reasons” | 7 | 2.3 |
| Difficulties establishing breastfeeding | ||
| “I had no milk letdown” | 74 | 23.8 |
| “my baby would not latch on” | 15 | 4.8 |
| Maternal health problems | 85 | 27.3 |
| Infant health problems | 21 | 6.8 |
| Infant was adopted | 11 | 3.5 |
| Maternal employment | 9 | 2.9 |
| Advice from a health professional | 6 | 1.9 |
| Total | 311 | 100 |
Table 3 summarises the main reasons for BF cessation. The 2 most frequent reasons were insufficient milk supply/I produced no milk/I stopped producing milk (32.3%) and returning to work (25.9%).
Main reasons for BF cessation reported by mothers (mothers in the sample of the 2012–2013 ELOIN study).
| Main reasons reported | n | % |
|---|---|---|
| Insufficient milk supply | ||
| “insufficient milk supply/I had no milk/I stopped producing milk” | 716 | 32.3 |
| “low weight gain in infant” | 74 | 3.3 |
| “infant was still hungry after BF” | 8 | 0.4 |
| Return to work | 575 | 25.9 |
| Mother's choice | ||
| “I wanted to/I felt it was time to stop” | 351 | 14.2 |
| “I did not like BF/found it uncomfortable. Bottle feeding was easier/more convenient” | 20 | 0.9 |
| “Personal reasons” | 7 | 0.3 |
| Infant self-weaned | 276 | 12.4 |
| Problems with breasts (pain, cracked nipples, mastitis) | 76 | 3.4 |
| Maternal health problem | 64 | 2.9 |
| Infant health problem | 34 | 1.5 |
| New pregnancy | 29 | 1.3 |
| Advice of health professional | 23 | 1 |
| Total | 2217 | 100 |
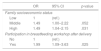
Logistic regression showed that mothers in families of middle to high socioeconomic status were 1.49 times more likely to practice EBF compared to mothers of low socioeconomic status, and that the probability of EBF was nearly double in mothers that attended a BF workshop after delivery compared to mothers that did not (Table 4).
Variables associated to the practice of exclusive breastfeeding based on the multivariate logistic regression model (sample of the 2012–2013 ELOIN study).
| OR | 95% CI | p-value | |
|---|---|---|---|
| Family socioeconomic status | |||
| Low | 1 | (ref.) | |
| Middle | 1.49 | 1.00–2.22 | .052 |
| High | 1.49 | 1.04–2.15 | .031 |
| Participation in breastfeeding workshop after delivery | |||
| No | 1 | (ref.) | |
| Yes | 1.99 | 1.09–3.63 | .025 |
CI, confidence interval; OR, odds ratio.
Maintenance of EBF for 6 months was associated with greater maternal age, maternal residence in Spain of less than 10 years, participation in BF after delivery and not belonging to the middle class (Table 5).
Variables associated with maintenance of exclusive breastfeeding for 6 months based on the multivariate logistic regression model (sample of the 2012–2013 ELOIN study).
| OR | 95% CI | p-value | |
|---|---|---|---|
| Infant sex | |||
| Male | 1 | (ref) | |
| Female | 1.18 | 0.98–1.43 | .087 |
| Maternal age at birth | |||
| <20 years | 1 | (ref) | |
| 20–35 years | 2.45 | 1.05–5.72 | .039 |
| >35 years | 2.76 | 1.16–6.53 | .021 |
| Duration of mother's residence in Spain, years | |||
| Spanish mother | 1 | (ref) | |
| ≥10 years | 1.10 | 0.83–1.47 | .512 |
| <10 years | 1.55 | 1.13–2.12 | .007 |
| Family social class | |||
| Classes I and II (managers, university graduates, artists, athletes) | 1 | (ref) | |
| Class III (administrative, security and services) | 0.65 | 0.48–0.87 | .004 |
| Classes IV and V (skilled and non-skilled manual labour) | 1.07 | 0.82–1.40 | .622 |
| Never employed | 1.77 | 0.58–5.41 | .316 |
| Participation in breastfeeding workshop after delivery | |||
| No | 1 | (ref) | |
| Yes | 1.49 | 1.12–1.99 | .007 |
CI, confidence interval; OR, odds ratio; ref, reference.
In children born between 2008 and 2009 in the Community of Madrid, the prevalence of EBF at 6 months was 25.4%, and the prevalence of BF at 2 years was 7.7%. The most frequent reasons for not initiating BF were personal choice of the mother, difficulties establishing BF and maternal health problems. The main reasons for BF cessation were insufficient milk supply and returning to work. Middle-to-high socioeconomic status and participation in a BF workshop were associated with an increased prevalence of EBF. Maintenance of EBF for 6 months was associated with greater maternal age, lower duration of residence in Spain and participation in BF workshops.
The prevalence of EBF at 6 months was similar to that reported for Spain in 200621 and for Castilla y León in 2009,9 slightly greater than that reported the same year for Gipuzkoa8 or Aragon22 and lower than the prevalence reported for Spain in the 2011–2012 period.20 The prevalence of BF at 6 months was similar to the prevalence reported for Spain in 2011–201220 and for Aragon,22 and greater than the prevalence reported for Castilla y León.9 These differences may be due to differences in the methodology used for data collection or in the characteristics or BF habits of the populations under study.
When it comes to the Community of Madrid, our study found a prevalence of EBF at 6 months similar to the one reported by the 2006 ENSE health survey for the Community of Madrid21 and higher than the prevalence calculated based on the electronic health records of the primary care system for 2011.23 These differences may be due to the latter defining BF at 6 months as excluding formula feeding, which may not have corresponded exactly with the definition of EBF used in this study. In any case, the population born in 2008 and 2009 residing in the Community of Madrid has not met the global target of a 50% prevalence of EBF at 6 months,12 and the recommendation of continuing BF until age 2 years was also not met.6
As for the reasons to not initiate BF, several studies have suggested that many women do not pursue BF because they are not aware of how important it is for health.24 Difficulties in establishing BF usually involve problems with BF technique that could be minimised with correct health care and adequate training of the mother.25 With a few exceptions, health problems are not a contraindication for BF.26 These data suggest that there is a significant opportunity for intervention in BF promotion through improving the information and training provided to mothers. We would propose following the recommendations of the Estrategia de Atención al Parto Normal (Care Strategy for Normal Deliveries)27 and the Iniciativa para la Humanización de la Asistencia al Nacimiento y la Lactancia (Initiative for the Humanization of Care in Childbirth and Lactation [IHAN]).28
There were also 2.9% of mothers that reported they did not initiate BF due to work-related reasons, and another 1.9% on the advice of a health professional. These data diverge from the findings of other studies in which the main reason for not initiating BF were immediate return to work in 33.8% of mothers and lack of support from health professionals in 32.4%.29
One third of mothers reported a perceived insufficient milk supply as the reason that led to BF cessation. One of the most frequent causes of insufficient milk production is poor BF technique, which can be resolved by providing adequate support to the mother.4,30 In addition, insufficient milk production may be associated with infant self-weaning, which is another of the reasons given for BF cessation. If the two were truly associated, training the mother on adequate technique could both improve milk production and motivate the infant to continue nursing.
More than 25% of the mothers reported returning to work as the main reason for discontinuing BF. There are studies that show that the prolongation of maternity leave and a supportive work environment after the return to work protect and help maintain BF.30,31 Businesses and governmental institutions should study this factor in order to guarantee a duration of maternity leave that would facilitate maintenance of EBF for at least 6 months.
Only 3.4% of mothers reported discontinuing BF due to breast problems (pain, cracked nipples, mastitis). This percentage was low, which could be due to recall bias; as years go by, mothers tend to have better recall of child health problems or external pressures as reasons for BF cessation. At any rate, some of the problems involving the breasts can be resolved with adequate BF support services.24,29
The proportion of mothers from families of middle-to-high socioeconomic status that initiated BF was 1.5 times that of mothers of low socioeconomic status. The association of EBF with high socioeconomic status has been described previously,29 and mothers with a privileged economic situation may be more aware of the importance of BF and probably have better access to help and resources to address any difficulties that arise.32–34 Ensuring universal access to BF support programmes would help narrow this social inequality gap.
Nearly 3 times as many mothers aged more than 35 years maintained EBF for 6 months compared to mothers aged less than 20 years. This association between age and EBF has already been described in other studies.7 Maintenance of EBF for 6 months was also more frequent in mothers that had been residing in Spain for less than 10 years. It is possible that this association is due to mothers that have been in Spain for few years maintaining the BF culture of their country of origin.
Participation in a BF workshop after delivery was associated with the establishment of EBF and its maintenance for 6 months. It is possible that mothers that attended the workshops did it because they were more motivated to breastfeed so that workshop attendance was an effect of this motivation rather than a factor that promoted BF, or that, on the contrary, they were mothers experiencing BF difficulties that were resolved by attending the workshop, so that attendance did facilitate the establishment and continuation of BF. There is sufficient scientific evidence suggesting that workshops help overcome difficulties associated with BF and raise awareness in mothers of the importance of BF and its impact on health.30 In this regard, we ought to highlight that fewer than 10% of mothers in the ELOIN study reported having participated in BF workshops after delivery. The development and implementation of strategies for promoting maternal participation in BF workshops in primary care centres may be beneficial in this regard.33
Limitations of the studyWe obtained the data from the ELOIN study, whose main focus was not BF, so that data on some significant determinants of BF were not recorded and, therefore, could not be analysed. For instance, the ELOIN study did not assess factors that may facilitate BF, such as the type of pregnancy, the information on BF received during pregnancy, perinatal care, physical contact of mother and newborn, early initiation of BF7,35 or previous experiences with BF that may influence its current establishment and duration. The cross-sectional design of the study also precluded followup of BF. The information was collected retrospectively, 4 years after delivery, so we cannot rule out recall bias in the responses given in the questionnaires. In this sense, it is possible that the reported BF rates overestimated the actual rates. The proportion of mothers that had a high school or a university education and of middle or high socioeconomic status was slightly above the average of the Community of Madrid, a finding that was consistent with those of previous studies, which have reported a greater participation of university-educated individuals in health surveys.30 These two characteristics may have led to an overestimation of the prevalence of BF in our study, as both high maternal educational attainment and high household income facilitate BF.
In the Community of Madrid, in the 2008–2009 period, the recommendation of the WHO of maintaining EBF through age 6 months was not met in 3 out of 4 infants, and continued BF through age 2 years only occurred in 20%. Breastfeeding rates were higher in mothers of greater age, higher socioeconomic status, who had resided in Spain for less than 10 years and who attended BF workshops. The practice of BF is associated with social inequalities, does not depend exclusively on the personal decisions of mothers, and depends on factors that can be remedied with public health measures: adequate support of mothers during gestation, delivery and the postpartum period, and interventions to promote, protect and support BF in multiple sectors of society.24,36 Studies on the prevalence of BF are absolutely necessary to monitor the status quo and temporal trends in its practice.
FundingThe ELOIN study was funded by a research grant from the Department of Health of the Community of Madrid (project number: RS_AP10-13).
Conflicts of interestThe authors have no conflicts of interest to declare.
We thank Lucia Diez-Gañan for her contribution to the design of the questionnaire.
Please cite this article as: Ramiro González MD, Ortiz Marrón H, Arana Cañedo-Argüelles C, Esparza Olcina MJ, Cortés Rico O, Terol Claramonte M, et al. Prevalencia de la lactancia materna y factores asociados con el inicio y la duración de la lactancia materna exclusiva en la Comunidad de Madrid entre los participantes en el estudio ELOIN. An Pediatr (Barc). 2018;89:32–43.