The objective of this study was to describe the current practice regarding the preparation of the sedation–analgesia (SA) procedures performed in the paediatric emergency centres in Spain.
Material and methodsA multicentre, observational and prospective analytical study was carried out on the SA procedures that were performed on children under 18 years old in 18 paediatric emergency departments between February 2015 and January 2016.
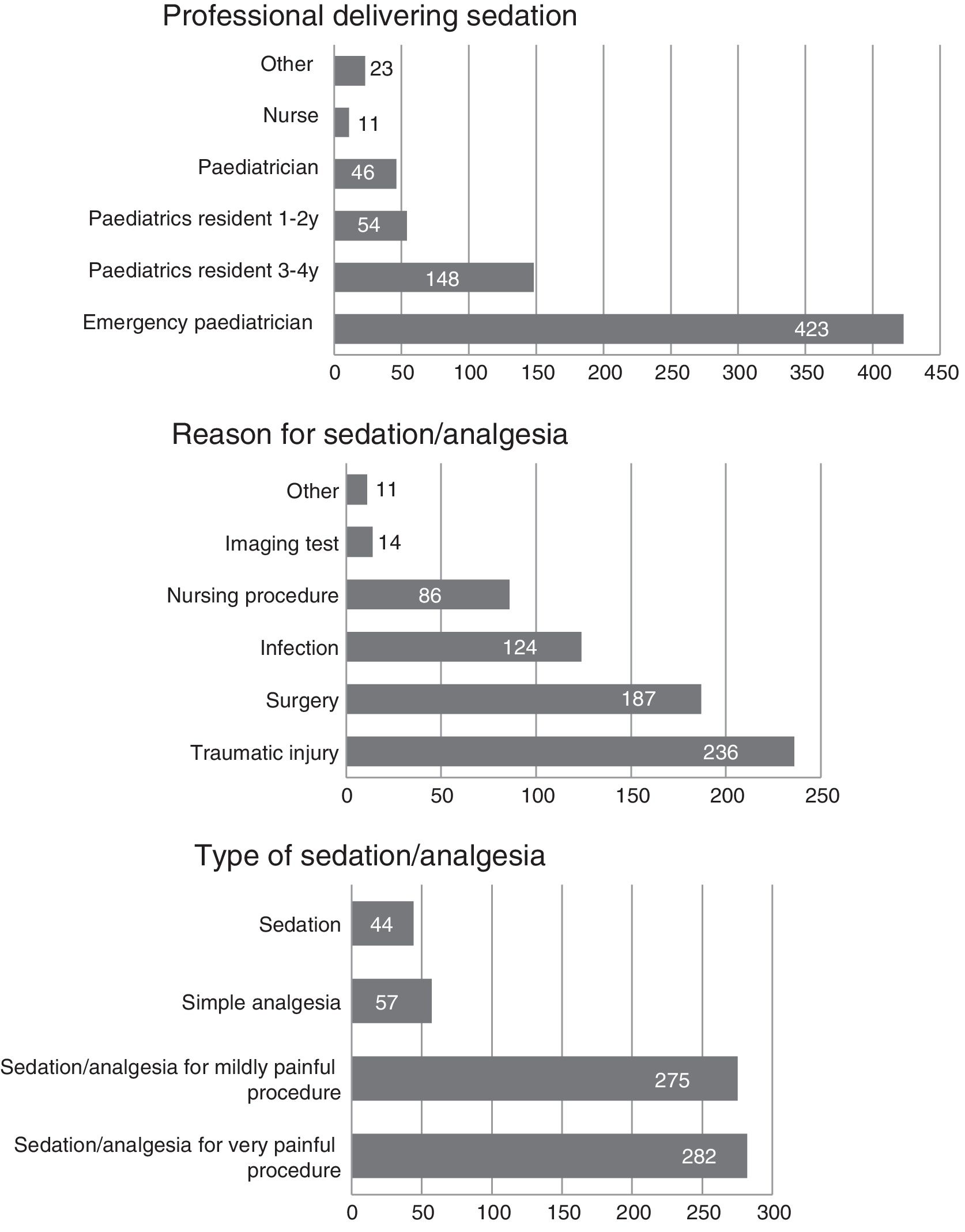
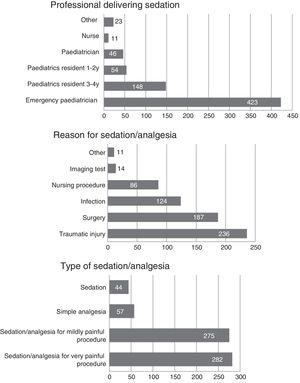
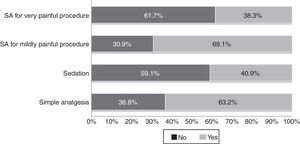
ResultsA total of 658 SA procedures were registered in 18 hospitals of Spain, most of them to children older than 24 months. The type of the procedure was: simple analgesia in 57 (8.6%), sedation in 44 (6.7%), SA for a not very painful procedure in 275 (41.8%), and SA for a very painful procedure in 282 (42.9%). Informed consent was requested in 98.6% of the cases. The written form was more frequently preferred in the group of patients that received SA for a very painful procedure (76.6%) in comparison to a painful procedure or to simple analgesia (62.9% and 54.4%, respectively, p<.001). The staff that most frequently performed the SA procedures were the paediatricians of the emergency departments (64.3%), followed by paediatrics residents (30.7%). The most frequent reasons for the SA were traumatological (35.9%) and surgical (28.4%). Fasting was observed in 81% of the cases. More than two-thirds (67.3%, n=480) children were monitored, the majority (95.8%) of them using pulse oximetry. The pharmacological strategy used was the administration of one drug in 443 (67.3%) of the cases, mostly nitrous oxide, and a combination of drugs in 215 (32.7%), especially midazolam/ketamine (46.9%).
ConclusionThe majority of the SA procedures analysed in this study have been carried out correctly and prepared in accordance with the current guidelines.
El objetivo de este estudio fue describir la práctica clínica actual de la preparación de los procedimientos de sedoanalgesia (SA) realizados en servicios de urgencias pediátricas (SUP) españoles.
Material y métodosEstudio multicéntrico, observacional y analítico prospectivo de los procedimientos de SA realizados a niños menores de 18 años en 18 SUP entre febrero del 2015 y enero del 2016.
ResultadosSe registraron 658 procedimientos de SA en 18 hospitales de España, la mayoría (90,7%) en mayores de 24 meses. El tipo de procedimiento fue: 57 (8,6%) analgesia simple, 44 (6,7%) sedación, 275 (41,8%) SA para procedimiento poco doloroso y 282 (42,9%) SA para procedimiento muy doloroso. Se solicitó consentimiento informado al 98,6%, siendo más frecuentemente escrito en el grupo de SA para procedimientos muy dolorosos (76,6%) que en procedimientos poco dolorosos o en analgesia simple (el 62,9 y el 54,4%, respectivamente, p<0,001). El personal que más frecuentemente realizó la SA fueron los pediatras de urgencias (64,3%), seguidos de los residentes de pediatría (30,7%). Los motivos de la SA más frecuentes fueron los traumatológicos (35,9%) y quirúrgicos (28,4%). El ayuno se valoró en el 81%. Se monitorizaron 480 (73%) niños, la mayoría de ellos con pulsioxímetro (95,8%). La estrategia farmacológica utilizada fue la administración de un fármaco de forma aislada en 443 (67,3%) de los casos, siendo más frecuente el óxido nitroso (50%) y una combinación de fármacos en 215 (32,7%), destacando la combinación midazolam/ketamina (46,9%).
ConclusiónLa mayoría de los procedimientos de SA analizados en este estudio han tenido una preparación correcta y acorde a las recomendaciones actuales.
Pain and fear of pain cause a great part of the suffering experienced by children when they visit a health care facility. Both may be present in the child on arrival to the facility, or may be caused or elicited by the diagnostic or therapeutic procedures required by the patient.1,2
Pain must be managed safely and effectively, regardless of age, maturity or severity of disease for physiological, moral, humane and ethical reasons.3–5 Furthermore, it is known that untreated pain has physiological and psychological consequences, increasing the pain associated with future procedures.6
Until recent years, the management of pain and anxiety in children was one of the most neglected aspects of care in paediatric emergency departments (PEDs) due to the very nature of emergency care, in which time is a critical factor.7 However, in the past few years there has been a growing interest among paediatric emergency physicians in providing adequate sedation and analgesia (SA) to their patients.2
Today, the need for sedation and analgesia is considered indisputable. It is also understood that the correct management of SA and patient safety during its administration require not only the identification of the need for SA, but also adequate training of the staff that delivers SA to minimise and correctly address its risks.3,4 Thus, adequate staff training and protocol development are crucial to the safety of paediatric patients.4
In 2009, the Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría (Spanish Society of Paediatric Emergency Medicine [SEUP]) developed the first manual on analgesia and sedation in the paediatric emergency setting, followed by the introduction in 2015 of a nationwide register of SA procedures performed in Spanish PEDs.
ObjectiveThe aim of our study was to analyse the preparation of SA procedures in 18 PEDs in Spain, and to find out the characteristics of the patients that underwent these procedures.
Materials and methodsStudy designWe conducted a multicentre, prospective, observational and analytical study of the SA procedures performed in a 1-year period in participating PEDs.
The study was approved by the institutional research ethics committees of each participating centre and adhered to the principles of the Declaration of Helsinki.
We obtained the informed consent of the parents or legal guardians of each of the patients included in the study.
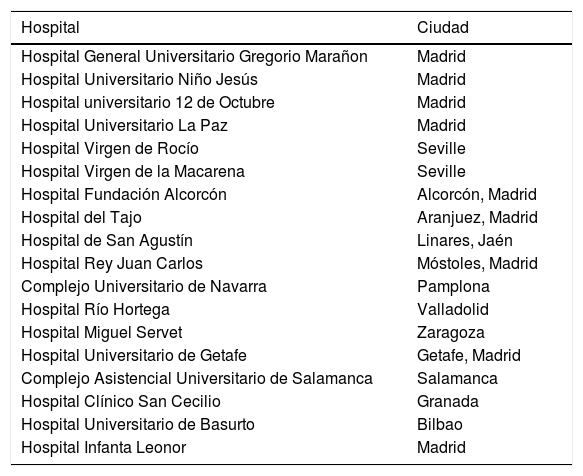
Study universe and settingWe conducted the study in 18 PEDs associated with the Working Group on Sedation and Analgesia of the SEUP (Table 1) between February 1, 2015 and January 31, 2016.
List of participating paediatric emergency departments.
| Hospital | Ciudad |
|---|---|
| Hospital General Universitario Gregorio Marañon | Madrid |
| Hospital Universitario Niño Jesús | Madrid |
| Hospital universitario 12 de Octubre | Madrid |
| Hospital Universitario La Paz | Madrid |
| Hospital Virgen de Rocío | Seville |
| Hospital Virgen de la Macarena | Seville |
| Hospital Fundación Alcorcón | Alcorcón, Madrid |
| Hospital del Tajo | Aranjuez, Madrid |
| Hospital de San Agustín | Linares, Jaén |
| Hospital Rey Juan Carlos | Móstoles, Madrid |
| Complejo Universitario de Navarra | Pamplona |
| Hospital Río Hortega | Valladolid |
| Hospital Miguel Servet | Zaragoza |
| Hospital Universitario de Getafe | Getafe, Madrid |
| Complejo Asistencial Universitario de Salamanca | Salamanca |
| Hospital Clínico San Cecilio | Granada |
| Hospital Universitario de Basurto | Bilbao |
| Hospital Infanta Leonor | Madrid |
We selected children that visited any of the participating PEDs and underwent some type of SA procedure with a dissociative drug, opioid analgesic and/or sedative.
The inclusion criteria were age 0–18 years and signing of informed consent form by the parents or legal guardians and, in patients aged more than 12 years, the patient as well.
We excluded children that did not meet the inclusion criteria or for whom we were unable to obtain signed informed consent.
Data collectionA data collection notebook was filled out for each study participant.
Each facility encoded the notebooks with an alphanumeric code to safeguard the confidentiality of patients.
Every month, the researchers in each centre submitted the data on the procedures performed in their facilities electronically to the principal investigator, who was responsible for the study database.
We collected epidemiological variables, patient-related variables (physical status classification of the American Society of Anesthesiologists [ASA],8 ongoing pharmacological treatment, fasting, anticipatory anxiety, level of pain before treatment, physical examination), variables related to the preparation of the SA procedure (reason for SA, type of procedure, monitoring, pharmacological approach used, professional in charge of providing SA, request for informed consent, and presence of parents during the procedure).
Outcome measurementWe classified the type of SA procedure based on the clinical situation into simple analgesia (isolated administration of an opioid drug for the prevention of procedural pain without the intent of producing a state of sedation), sedation (administration of sedative or antianxiety agents to achieve a depressed level of consciousness of varying degree with the purpose of facilitating patient cooperation in a painless procedure, such as an imaging test) or SA (administration of opioid analgesic and/or topical/local anaesthesia combined with a sedative or administration of dissociative anaesthesia to allow the patient tolerate an unpleasant and painful procedure). The latter included SA for a mildly painful procedure (such as venepuncture, lumbar puncture or simple wound repair) and SA for very painful procedures (such as closed reduction of fractures or electrical cardioversion).8
Pain was measured by means of age-appropriate validated scales (the FLACC observational pain assessment scale,9 the Wong-Baker FACES rating scale10 and a numerical scale). Anticipatory anxiety was measured by means of a scale designed to assess anxiety related to short procedures comprising 2 items: crying and muscle tension (Groningen distress scale).11
Statistical analysisWe analysed the collected data using the software SPSS version 21.0.
We have expressed categorical variables as absolute frequencies and percentages.
We summarised normally distributed variables as mean and standard deviation. Normality was assessed by means of the Shapiro–Wilk test.
We compared means using parametric tests (Student t and ANOVA) or nonparametric tests (Mann–Whitney U and Kruskal–Wallis tests).
We analysed the association between qualitative variables with the chi square test or the Fisher exact test. We calculated odds ratios with their corresponding confidence intervals to measure the strength of association.
Results with p-values of less than 0.05 were considered statistically significant.
ResultsA total of 658 SA procedures were registered between February 1, 2015 and January 31, 2016, of which 404 (61%) were performed in male patients. The mean patient age was 6.6 years (SD, 4 years), and 592 children (90.7%) were aged more than 2 years.
Out of all SA procedures, 69% were performed on weekdays. Also, 311 (47.9%) were performed in the afternoon, 254 (38.6%) in the morning and 89 (13.5%) at night.
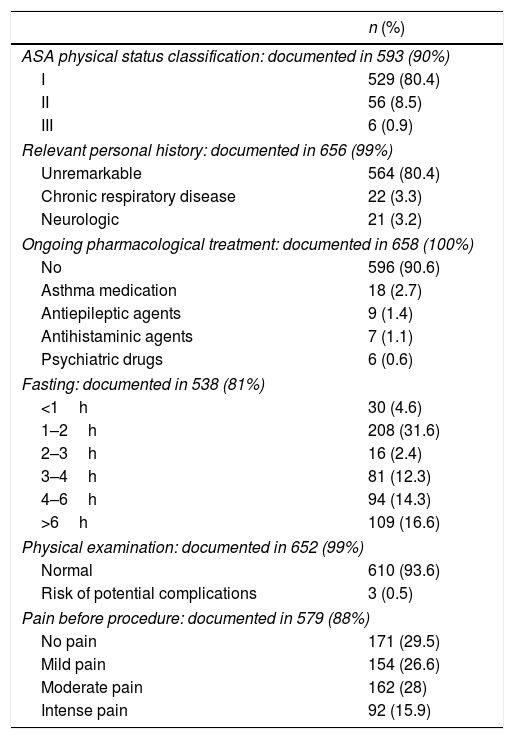
Table 2 summarises the characteristics of the evaluation prior to SA performed in the children included in the study. We ought to note that 6 of the included patients were classified as ASA III, and that 4 of them were managed by paediatric emergency physicians with appropriate training for performing SA procedures in this type of patient.
Characteristics of patient evaluations preceding sedation and analgesia.
| n (%) | |
|---|---|
| ASA physical status classification: documented in 593 (90%) | |
| I | 529 (80.4) |
| II | 56 (8.5) |
| III | 6 (0.9) |
| Relevant personal history: documented in 656 (99%) | |
| Unremarkable | 564 (80.4) |
| Chronic respiratory disease | 22 (3.3) |
| Neurologic | 21 (3.2) |
| Ongoing pharmacological treatment: documented in 658 (100%) | |
| No | 596 (90.6) |
| Asthma medication | 18 (2.7) |
| Antiepileptic agents | 9 (1.4) |
| Antihistaminic agents | 7 (1.1) |
| Psychiatric drugs | 6 (0.6) |
| Fasting: documented in 538 (81%) | |
| <1h | 30 (4.6) |
| 1–2h | 208 (31.6) |
| 2–3h | 16 (2.4) |
| 3–4h | 81 (12.3) |
| 4–6h | 94 (14.3) |
| >6h | 109 (16.6) |
| Physical examination: documented in 652 (99%) | |
| Normal | 610 (93.6) |
| Risk of potential complications | 3 (0.5) |
| Pain before procedure: documented in 579 (88%) | |
| No pain | 171 (29.5) |
| Mild pain | 154 (26.6) |
| Moderate pain | 162 (28) |
| Intense pain | 92 (15.9) |
ASA, American Society of Anesthesiologists.
The duration of fasting was assessed in 538 children (81%). Fasting time was less than 2h in 50.9% of children that underwent simple analgesia, 46.2% of children that underwent sedation, 31.6% of children that received SA for a very painful procedure and 25.5% of children that received SA for mildly painful procedures, and the difference was only statistically significant between the simple analgesia group and the SA for mildly painful procedures group (p<.01).
Anticipatory anxiety was assessed in 608 children (92%). When it came to patient age, and excluding the subset of patients that experienced panic, we observed that anticipatory anxiety increased with decreasing age, although the correlation was weak (rho, 0.18; p<.01).
Fig. 1 summarises the reasons for use of SA, the type of SA procedures performed, and the type of professional that carried out the procedures.
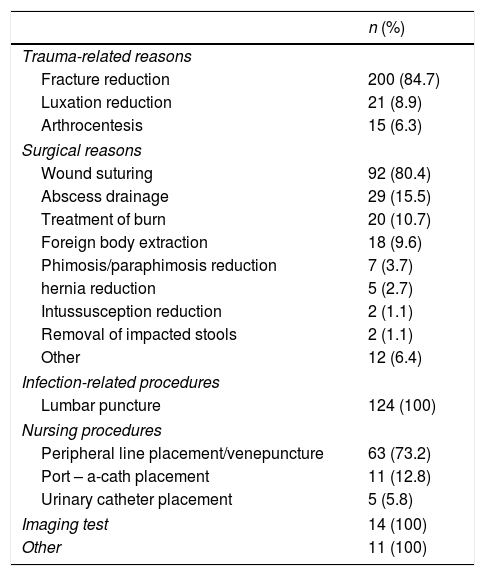
Table 3 summarises the most frequent reasons that led to the use of SA in our study.
Reason for use of sedation and analgesia.
| n (%) | |
|---|---|
| Trauma-related reasons | |
| Fracture reduction | 200 (84.7) |
| Luxation reduction | 21 (8.9) |
| Arthrocentesis | 15 (6.3) |
| Surgical reasons | |
| Wound suturing | 92 (80.4) |
| Abscess drainage | 29 (15.5) |
| Treatment of burn | 20 (10.7) |
| Foreign body extraction | 18 (9.6) |
| Phimosis/paraphimosis reduction | 7 (3.7) |
| hernia reduction | 5 (2.7) |
| Intussusception reduction | 2 (1.1) |
| Removal of impacted stools | 2 (1.1) |
| Other | 12 (6.4) |
| Infection-related procedures | |
| Lumbar puncture | 124 (100) |
| Nursing procedures | |
| Peripheral line placement/venepuncture | 63 (73.2) |
| Port – a-cath placement | 11 (12.8) |
| Urinary catheter placement | 5 (5.8) |
| Imaging test | 14 (100) |
| Other | 11 (100) |
We analysed the type of SA used based on the type of professional that delivered it and found that paediatric emergency physicians and third- and fourth-year paediatrics residents used SA for mildly or very painful procedures more frequently than nurses or first-year paediatrics residents, who were more likely to use simple analgesia and sedation (p<.01).
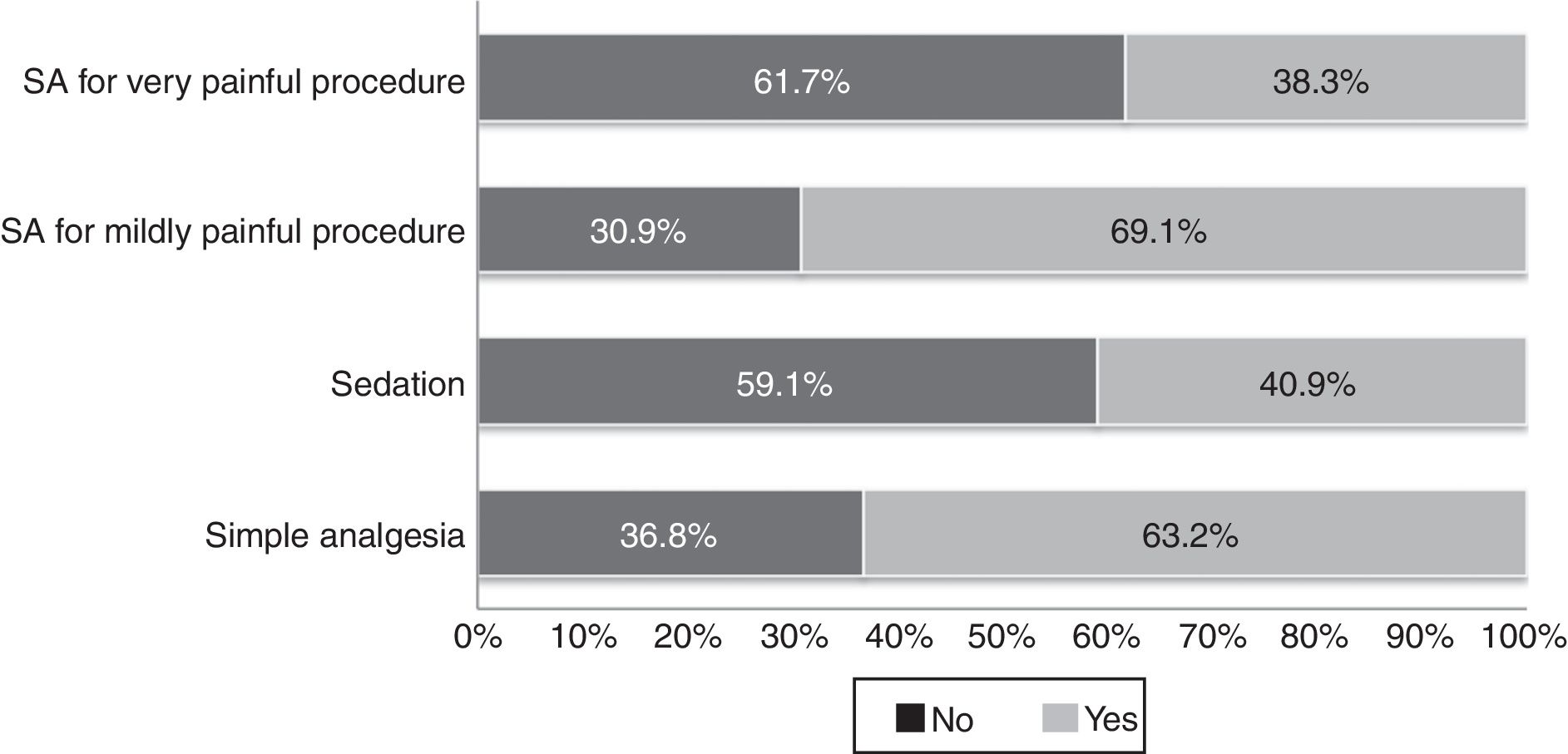
Informed consent for performance of SA was requested in 649 (98.6%) procedures; it was obtained in writing in 444 cases (67.5%) and verbally in the remaining 205 (31.2%).
We analysed whether consent was obtained in writing or verbally based on the type of SA procedure to be performed, and found that consent was obtained in writing more frequently for SA for very painful procedures (76.6%) compared to SA for mildly painful procedures or simple analgesia (62.9% and 54.4%, respectively; p<.001).
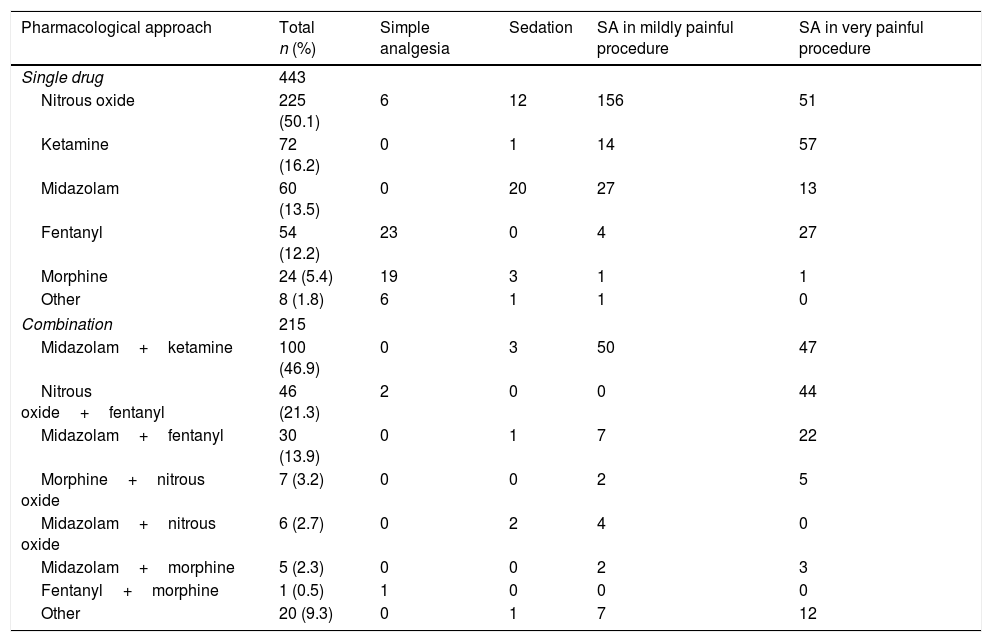
The pharmacological strategy consisted in the administration of a single drug in 443 of cases (67.3%) and of a combination of drugs in 215 (32.7%) (Table 4).
Drugs used in sedation and analgesia procedures.
| Pharmacological approach | Total n (%) | Simple analgesia | Sedation | SA in mildly painful procedure | SA in very painful procedure |
|---|---|---|---|---|---|
| Single drug | 443 | ||||
| Nitrous oxide | 225 (50.1) | 6 | 12 | 156 | 51 |
| Ketamine | 72 (16.2) | 0 | 1 | 14 | 57 |
| Midazolam | 60 (13.5) | 0 | 20 | 27 | 13 |
| Fentanyl | 54 (12.2) | 23 | 0 | 4 | 27 |
| Morphine | 24 (5.4) | 19 | 3 | 1 | 1 |
| Other | 8 (1.8) | 6 | 1 | 1 | 0 |
| Combination | 215 | ||||
| Midazolam+ketamine | 100 (46.9) | 0 | 3 | 50 | 47 |
| Nitrous oxide+fentanyl | 46 (21.3) | 2 | 0 | 0 | 44 |
| Midazolam+fentanyl | 30 (13.9) | 0 | 1 | 7 | 22 |
| Morphine+nitrous oxide | 7 (3.2) | 0 | 0 | 2 | 5 |
| Midazolam+nitrous oxide | 6 (2.7) | 0 | 2 | 4 | 0 |
| Midazolam+morphine | 5 (2.3) | 0 | 0 | 2 | 3 |
| Fentanyl+morphine | 1 (0.5) | 1 | 0 | 0 | 0 |
| Other | 20 (9.3) | 0 | 1 | 7 | 12 |
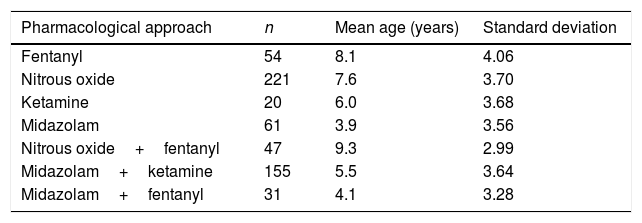
Table 5 shows the mean age of the patients for each pharmacological strategy. We found that the combination of nitrous oxide and fentanyl was used more frequently in older children (9.34 years) compared to the combination of midazolam and ketamine (5.51 years) or of midazolam and fentanyl (4.1 years), differences that were statistically significant (p<.001).
In 258 SA procedures (39%), a topical or local analgesic was added to the administration of systemic drugs (lidocaine/prilocaine in 16.7%, lidocaine-adrenaline-tetracaine [LAT] gel in 2.9% and local anaesthesia in 15.8%).
Monitoring was used in 480 children (73%), in most cases by pulse oximetry (95.8%). In addition, 95 patients (19.5%) underwent heart rate continuous ECG monitoring of the heart rate, 127 (26.4%) intermittent blood pressure measurements, and 21 (3.2%) monitoring of carbon dioxide partial pressure via nasal cannulae.
We assessed the potential association of monitoring and the type of SA procedure and found that monitoring was less frequent in simple analgesia procedures (19%) compared to the rest (87% of sedation procedures, 70% of SA for mildly painful procedures and 87% of SA in very painful procedures; p<.001).
The parents of 352 patients (53.5%) were present during the procedure, and their presence was more frequent in nursing procedures (80%) and surgical procedures (69%) compared to all other procedures in which SA was used (p<.01).
The presence of parents in relation to the type of SA procedure was more frequent in children that received simple analgesics (73%) or SA for less painful procedures (68%) compared to the rest of SA procedures (40% of patients that underwent sedation and 38% of patients that underwent SA for very painful procedures; p<.01) (Fig. 2).
We also observed that parental presence decreased the more pain the child expressed before the procedure (p=.09) and the deeper the target level of sedation (p<.01).
The length of stay in the emergency department was less than 1h in 125 procedures (19%), 1–2h in 359 (54.6%) and more than 3h in 154 (23.4%). We observed that the stay in the PED was longer (>3h) in patients that underwent sedation (34.6%) or when SA was used for mildly painful procedures (34.9%) compared to the rest of SA procedures (1.7% of patients that received simple analgesia and 16% of patients that received SA for very painful procedures; p<.01).
The discharge destination was the home in 71.9% of patients (473), while the other 28.1% (175) required hospital admission; adverse reactions to SA were the reason for admission in only 3 patients (1.7%). In these cases, the main adverse effect was dizziness associated with vomiting, requiring a 24-h stay in the paediatric ward. We observed that patients that underwent SA for mildly painful procedures were admitted more frequently than patients that underwent SA for very painful procedures (38.5% vs 15.2%; p<.01).
DiscussionThe purpose of procedural SA is to allow the patient to tolerate painful or unpleasant procedures while maintaining airway reflexes, ventilation and cardiovascular function.1 The guidelines of the American Academy of Pediatrics3 and the American Society of Anesthesiologists5 consider the use of procedural SA safe and appropriate for the management of pain and anxiety resulting from diagnostic and therapeutic procedures and methods. In addition, the prevention and alleviation of pain during diagnosis and treatment is a health care quality indicator in PEDs.4
The correct preparation of SA procedures is essential for their success, and protocols must be established to guarantee a correct and detailed evaluation of patients prior to any SA procedure.1,2,4 The use of checklists to apply specific guidelines can help prepare for SA procedures correctly and minimise potential adverse effects.11
As has been the case in previous studies,12,13 we observed that most paediatric patients were healthy individuals that were not receiving chronic medication and with normal findings on physical examination. According to the American Society of Anesthesiologists, only patients classified as ASA I or II3,5 can be considered candidates for receiving SA from non-anaesthesiologists. In our study, 6 patients were classified as ASA III, and 4 were managed by paediatric emergency physicians with adequate training, a parameter that needs improving, as 2 of these patients were managed incorrectly.
The ASA recommends taking certain precautions prior to SA. It recommends preprocedural fasting in patients undergoing elective procedures to reduce the risk of bronchoaspiration, and does not consider absence of fasting a contraindication in urgent procedures, while recommending an individualised risk-benefit assessment in all other cases.14
To date, several studies have been conducted that failed to establish an association between the incidence of adverse effects and the duration of fasting.15–19 In our study, the duration of fasting had been documented in most patients, however, we found considerable heterogeneity in this variable.
Sedation and analgesia must be considered a medical intervention apart from, and not part of, diagnostic procedures.2,3 Therefore, informed consent must be obtained separately before performing any SA procedures. In our study, informed consent was sought in almost every instance, although it was obtained in writing in only 2/3 of the patients. Whether consent was obtained in writing or verbally varied based on the type of procedure, as written consent was sought more frequently in SA procedures associated with a higher risk of complications, such as sedation or SA for very painful procedures. We did not find similar studies in the reviewed literature analysing how informed consent was obtained.
The pharmacological strategies selected for SA depend on the level of anxiety and pain that may be associated with the procedure.2,20 Drug selection requires a thorough knowledge of the pharmacodynamics, therapeutic effect, dosage and potential adverse effects of the different sedatives and analgesic agents, and providers must unfailingly avoid underdosing for fear of respiratory depression or out of a lack of familiarity with these drugs.4,20
In our study, nitrous oxide was used in nearly half of the procedures. This is an extensively studied drug that is easy to use and associated with few serious adverse effects.21,22 When it came to the combined use of drugs, the most frequent combination was midazolam and ketamine, drugs that are recommended for SA in children1,23 and which have been used frequently in similar studies.24
The use of local or topical anaesthesia in addition to systemic drugs is recommended to reduce pain in some techniques or procedures.23–25 There are numerous topical anaesthetic agents whose administration is not painful, such as lidocaine/prilocaine for intact skin and LAT gel for wounds.25 In our study, a topical or local anaesthetic was used in one third of the patients, most frequently a lidocaine/prilocaine anaesthetic cream.
Monitoring of vital signs is necessary to detect potential adverse effects as soon as possible.2,26 In our study, nearly 3/4 of the children were monitored, and the most frequently used monitoring technique was pulse oximetry, which was consistent with the findings of similar studies.23,24 It seems that most paediatricians are familiar with pulse oximeters, which may be the reason that this technique is used most frequently. Capnography is another method that provides thorough information on the respiratory pattern and the ventilatory status of the patient, and it can detect hypoventilation earlier than other methods; it is a particularly useful approach when providers do not have visual contact with the patient during the procedure.27 In our study, capnography was used in 21 patients (3.2%), probably due to its low availability in PEDs or to physicians not being well acquainted with this technique.
The use of nonpharmacological interventions for the management of anxiety and pain in paediatric patients is also important.9,23,28–30 The presence of the parents during procedures is becoming increasingly important, as it is consistent with the current patient- and family-centred approach to health care delivery.31,32 This strategy is not yet implemented in every PED or by all professionals with the justification that the presence of the family may add to the stress of health care providers and hinder the success of the procedure.32 However, this is not the case when procedures are carried out by experienced paediatricians.33 In our study, family members were present in a little over half of the procedures, and it is worth noting that the more pain the child expressed prior to the intervention, the less likely it was for parents to be present during the procedure. This suggests that not all providers in paediatric emergency settings feel confident in performing procedural SA, something that has already been described in similar studies.6,28
One of the limitations of our study is that although it was conducted in multiple centres, it was not representative of all of Spain, since several autonomous communities were not represented in the sample. Hospitals were randomly included in the study and the sampling method did not include stratification by autonomous community. Another potential limitation is that we do not know whether participating hospitals had protocols for SA at the time of the study, and therefore were unable to determine whether SA procedures were or not performed according to existing guidelines.
We would like to conclude by noting that most of the SA procedures analysed in this study were prepared correctly and in adherence with the recommendations of the American Society of Anesthesiologists and the guidelines of the American Academy of Paediatrics.
Conflicts of interestThe authors have no conflicts of interest to declare.
Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría: Ana Isabel Fernández Lorente, Pilar Storch Gracia de Calvo, Gloria Guerrero Márquez, Eva Benito Ruiz and Elena Sancho Gracia, Olga Serrano Ayestarán, Cristina Cordero Castro, Cecilio Palomino Muñoz, Sofía Mesa García, Cristina Muñoz López, Nuria Clerigué Arrita and Jorge Álvarez García, Isabel Cubero, José L Fernández Arribas, Alberto Barasoain Millán, Juan Antonio Cozar Olmo and José Luis Cuevas Cervera, Clara García and Carlos García Vao Bel, M. José Carbonero Celís and M. José Carpio Linde, Maite Alonso Salas, Vicente Barea.
The members of the Working Group on Analgesia and Sedation of the Sociedad Española de Urgencias de Pediatría are listed in Appendix A.
Please cite this article as: Míguez Navarro C, Oikonomopoulou N, Lorente Romero J, Vázquez López P, en representación del Grupo de Analgesia y Sedación de la Sociedad Española de Urgencias de Pediatría. Preparación de los procedimientos de sedoanalgesia en los servicios de urgencias pediátricos españoles: estudio descriptivo. An Pediatr (Barc). 2018;89:24–31.
Previous presentations: Descriptive study of the preparation of sedation and analgesia procedures in paediatric emergency departments. Concepción Míguez Navarro, Niki Oikonomopoulou, Jorge Lorente Romero, Paula Vázquez López. Hospital General Universitario Gregorio Marañón, Madrid, Spain.