There are no data on the incidence of hypoxic-ischaemic encephalopathy (HIE) and the implementation of therapeutic hypothermia (TH) in Spain.
MethodsThis is a cross-sectional, national study, performed using an on-line questionnaire targeting level III neonatal care units in Spain. Participants were requested to provide data of all newborns≥35 weeks of gestational age diagnosed with moderate-severe HIE over a two year-period (2012–2013), and of the implementation of TH up to June 2015.
ResultsAll (90) contacted hospitals participated. HIE incidence rate was 0.77/1000 live newborns (95% CI 0.72–0.83). During 2012–2013, 86% of the newborns diagnosed with moderate-severe HIE received TH (active or passive). Active TH was increasingly used, from 78% in 2012 to 85% in 2013 (P=.01). Of the 14% that did not receive TH, it was mainly due to a delay in the diagnosis or inter-hospital transfer, and to the fact that the treatment was not offered. More than half (57%) were born in hospitals where TH was not provided, and passive hypothermia was used for inter-hospital patient transfer, and in 39% of the cases by inappropriately trained personnel. By June 2015, 57 out of 90 centres had implemented TH, of which 54 performed whole-body TH (using servo-controlled devices). The geographical distribution of centres with active TH, and the number of newborn that received TH, was heterogeneous.
ConclusionsThe incidence of moderate-severe HIE is homogeneous across Spanish territory. Significant progress is being made in the implementation of TH, however it is necessary to increase the availability of active TH between Autonomous Communities, to improve early diagnosis, and to guarantee high quality patient transfer to referral centres.
La incidencia de la encefalopatía hipóxico-isquémica perinatal (EHI) y la implementación de la hipotermia terapéutica (HT) es desconocida en España.
MétodoEstudio transversal nacional en recién nacidos vivos (RNV) ≥ 35 semanas de gestación mediante cuestionario on-line en las 90 unidades neonatales de nivel iii. Se solicitaron datos de los RNV con EHI moderada-grave en los años 2012 y 2013, y de la implementación de la HT en junio del 2015.
ResultadosSe recibieron datos de los 90 hospitales. La incidencia de EHI moderada-grave fue 0.77/1.000 RNV (IC del 95%, 0.72; 0.83). El 86% de los RNV con EHI recibieron HT (activa o pasiva), aumentando los que recibieron HT activa del 78% en 2012 al 85% en 2013 (p=0.01). El 14% no recibió HT principalmente por retraso en el diagnóstico o en el traslado, o por no indicarse el tratamiento. El 57% de los RN nació en hospitales sin HT, siendo el traslado en hipotermia pasiva; en el 39% por equipos sin formación adecuada. En junio del 2015, 57/90 centros realizaban HT: 54 HT corporal total activa (todos con dispositivos servocontrolados). Existió heterogeneidad en la distribución por comunidades autónomas (CC. AA.) de centros con HT activa y en el número de RN que recibieron HT.
ConclusionesLa incidencia de EHI moderada-grave es homogénea entre CC. AA. Aunque se constata un importante progreso en la implementación de la HT, es preciso mejorar la disponibilidad de HT activa entre CC. AA., así como el diagnóstico precoz y el traslado con garantías desde los centros emisores.
Hypoxic-ischaemic encephalopathy (HIE) is a major cause of neonatal morbidity and mortality in full-term newborns (NBs) as well as permanent disability.1 Therapeutic hypothermia (TH) is a safe and effective treatment for HIE, and is currently considered part of the standard care for this disease.2,3 Several paediatric societies have recommended this treatment in their respective fields.4–8 However, the use of TH varies between Europe,9–13 the United States,14 Canada,15 Australia16 and Japan,6 and even differs between regions or geographical areas within single countries.9,14 In 2009, the Sociedad Española de Neonatología (Spanish Society of Neonatology [SENeo]) published guidelines to facilitate its use in clinical practice.17 The incidence of HIE and the implementation of TH in Spain overall and by autonomous community or city is currently unknown. This information is crucial in order to: (1) assess the current situation in the health care system and identify the needs in different geographical areas to correct inequalities in access to TH and (2) optimise programmes developed with the aim of delivering high-quality care to these patients.
In our study, we analysed the incidence of moderate-to-severe HIE in 2012 and 2013 and the use of TH through June 2015 in Spain overall and in its 17 autonomous communities (ACs) and 2 autonomous cities.
Patients and methodsWe conducted a cross-sectional nationwide study on moderate-to-severe HIE in NBs delivered at 35 or more weeks’ gestation by means of an online questionnaire. The study included every public and private tertiary care hospital with a level III neonatal care unit.18 We sent individual emails to each hospital requesting to have the coordinator with the most experience in the management of HIE complete the questionnaire. We contacted the coordinators when we detected errors or inconsistencies in the submitted data.
We requested the following data: (1) number of NBs delivered at ≥ 35 weeks’ gestation (years 2012 and 2013); (2) Live NBs that received a diagnosis of moderate-to-severe HIE in 2012 and 2013: number, origin (inborn or outborn), neonatal mortality, and (3) implementation of TH in each unit and during patient transport in June 2015: year that TH was first introduced, type of TH (passive or active; whole-body or selective head cooling), number of cooling devices available, number of live NBs treated with TH, reasons why TH was not used.
Operational definitionsWe defined moderate-to-severe perinatal HIE as altered level of consciousness (lethargy, stupor or coma) in the first 6 hours post birth associated with a perinatal history suggestive of a hypoxic-ischaemic insult: pH of cord blood or blood 1 hour post birth of 7 or less, or a base deficit of 16 or greater, and/or a 5-min Apgar score of 5 or less, and/or need of advanced life support.17
We have expressed the incidence rate as the number of live NBs delivered at 35 or more weeks’ gestation with moderate-to-severe HIE relative to the total number of live births reported by the Instituto Nacional de Estadística (National Institute of Statistics). To calculate the incidence relative to the total number of live births at 35 or more weeks’ gestation, we used data provided by the hospitals.
Therapeutic hypothermia: reduction of body temperature to 33°C or 34°C to be maintained for a period of 72h, either: (a) active, attained through manually controlled or servo-controlled devices, or (b) passive, through turning off sources of heat (incubator or radiant mattress) or the use of cold gel pads and/or fans.
Statistical analysisWe have summarised descriptive data as absolute frequencies and percentages. We have compared data for 2012 and 2013 with the chi square or the Fisher exact tests using the statistical package Epidat 3.1. We defined statistical significance as a p-value of less than 0.05 in any of the tests.
ResultsAll 90 level III neonatal units in Spain submitted data.
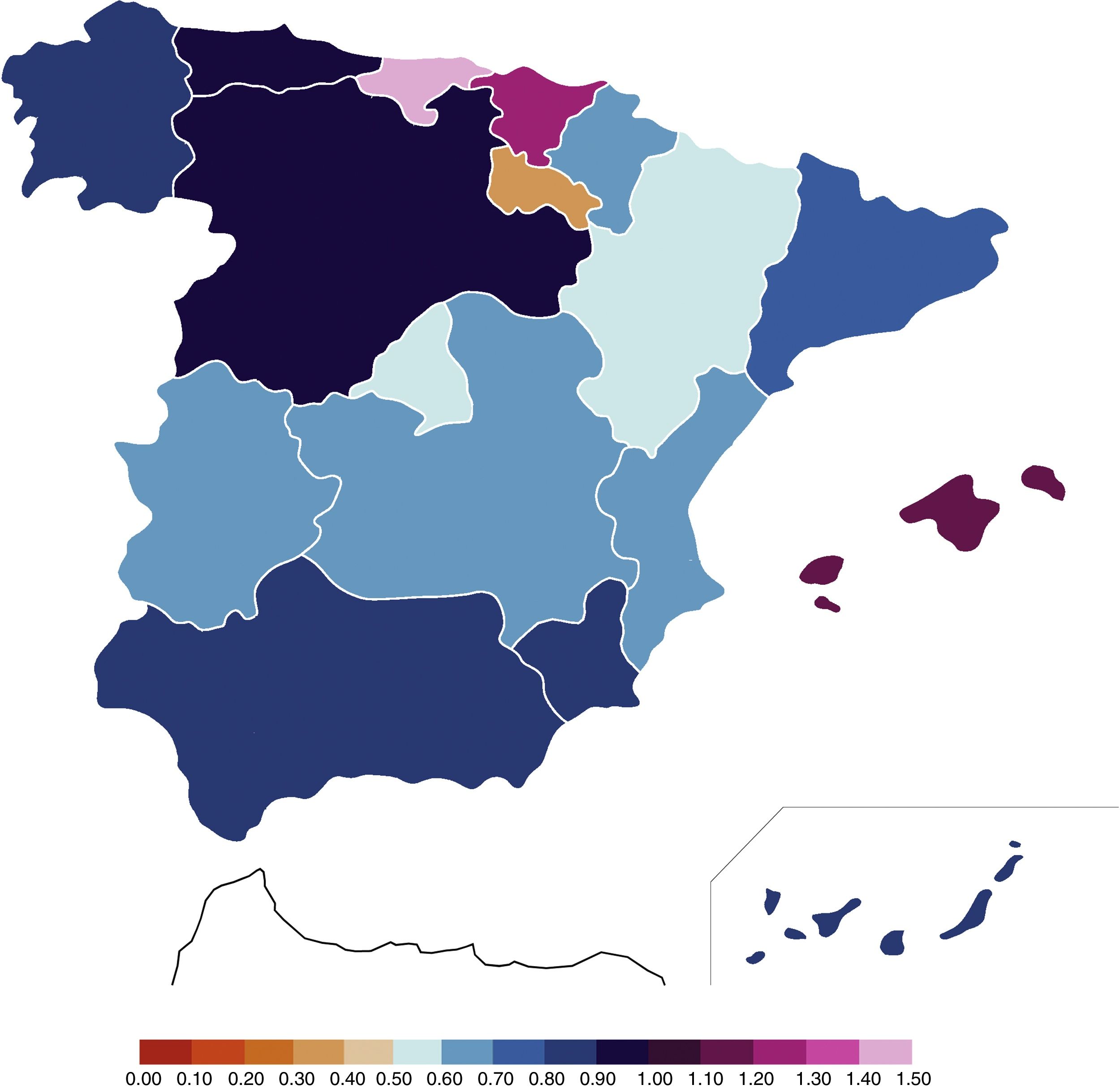
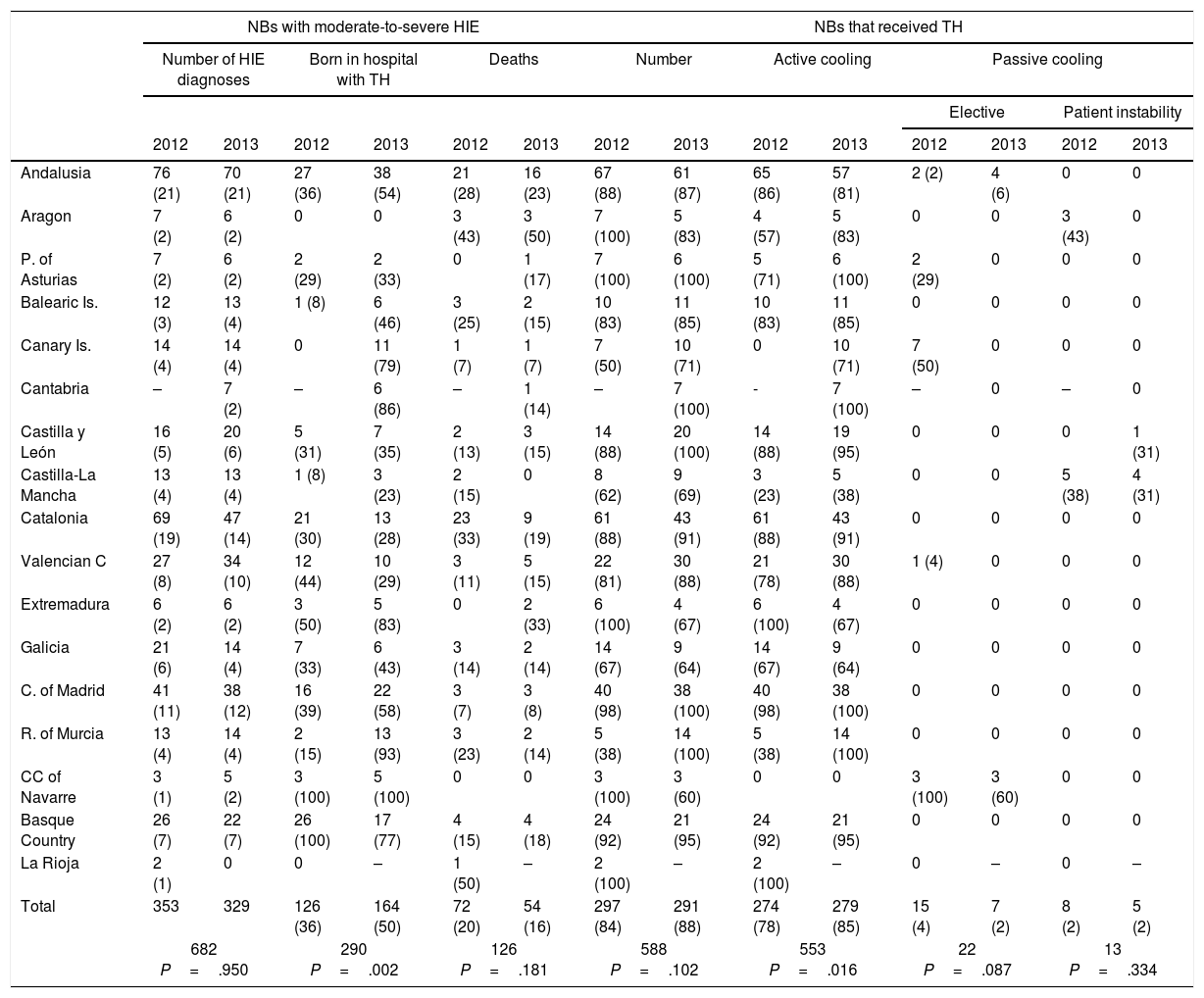
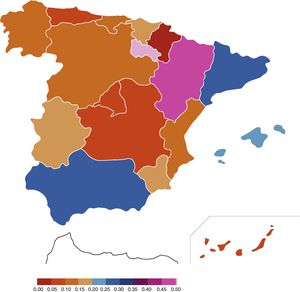
Frequency of hypoxic-ischaemic encephalopathy and management with therapeutic hypothermiaIn the 2012–2013 period, 682 NBs delivered at 35 or more weeks’ gestation received a diagnosis of moderate-to-severe HIE (353 in 2012 and 329 in 2013) which, relative to the total 880363 live births in Spain (454648 in 2012 and 425715 in 2013) corresponded to an incidence rate of 0.77/1000 live births (95% CI, 0.72–0.83), with no significant differences between the two years under study: 0.78 in 2012 (95% CI, 0.69–0.86) versus 0.77 in 2013 (95% CI, 0.69–0.86). Fig. 1 and Table 1 show the distribution by AC.
Data on the number of NBs with a diagnosis of HIE and treatment with TH (years 2012 and 2013).
| NBs with moderate-to-severe HIE | NBs that received TH | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of HIE diagnoses | Born in hospital with TH | Deaths | Number | Active cooling | Passive cooling | |||||||||
| Elective | Patient instability | |||||||||||||
| 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | |
| Andalusia | 76 (21) | 70 (21) | 27 (36) | 38 (54) | 21 (28) | 16 (23) | 67 (88) | 61 (87) | 65 (86) | 57 (81) | 2 (2) | 4 (6) | 0 | 0 |
| Aragon | 7 (2) | 6 (2) | 0 | 0 | 3 (43) | 3 (50) | 7 (100) | 5 (83) | 4 (57) | 5 (83) | 0 | 0 | 3 (43) | 0 |
| P. of Asturias | 7 (2) | 6 (2) | 2 (29) | 2 (33) | 0 | 1 (17) | 7 (100) | 6 (100) | 5 (71) | 6 (100) | 2 (29) | 0 | 0 | 0 |
| Balearic Is. | 12 (3) | 13 (4) | 1 (8) | 6 (46) | 3 (25) | 2 (15) | 10 (83) | 11 (85) | 10 (83) | 11 (85) | 0 | 0 | 0 | 0 |
| Canary Is. | 14 (4) | 14 (4) | 0 | 11 (79) | 1 (7) | 1 (7) | 7 (50) | 10 (71) | 0 | 10 (71) | 7 (50) | 0 | 0 | 0 |
| Cantabria | – | 7 (2) | – | 6 (86) | – | 1 (14) | – | 7 (100) | - | 7 (100) | – | 0 | – | 0 |
| Castilla y León | 16 (5) | 20 (6) | 5 (31) | 7 (35) | 2 (13) | 3 (15) | 14 (88) | 20 (100) | 14 (88) | 19 (95) | 0 | 0 | 0 | 1 (31) |
| Castilla-La Mancha | 13 (4) | 13 (4) | 1 (8) | 3 (23) | 2 (15) | 0 | 8 (62) | 9 (69) | 3 (23) | 5 (38) | 0 | 0 | 5 (38) | 4 (31) |
| Catalonia | 69 (19) | 47 (14) | 21 (30) | 13 (28) | 23 (33) | 9 (19) | 61 (88) | 43 (91) | 61 (88) | 43 (91) | 0 | 0 | 0 | 0 |
| Valencian C | 27 (8) | 34 (10) | 12 (44) | 10 (29) | 3 (11) | 5 (15) | 22 (81) | 30 (88) | 21 (78) | 30 (88) | 1 (4) | 0 | 0 | 0 |
| Extremadura | 6 (2) | 6 (2) | 3 (50) | 5 (83) | 0 | 2 (33) | 6 (100) | 4 (67) | 6 (100) | 4 (67) | 0 | 0 | 0 | 0 |
| Galicia | 21 (6) | 14 (4) | 7 (33) | 6 (43) | 3 (14) | 2 (14) | 14 (67) | 9 (64) | 14 (67) | 9 (64) | 0 | 0 | 0 | 0 |
| C. of Madrid | 41 (11) | 38 (12) | 16 (39) | 22 (58) | 3 (7) | 3 (8) | 40 (98) | 38 (100) | 40 (98) | 38 (100) | 0 | 0 | 0 | 0 |
| R. of Murcia | 13 (4) | 14 (4) | 2 (15) | 13 (93) | 3 (23) | 2 (14) | 5 (38) | 14 (100) | 5 (38) | 14 (100) | 0 | 0 | 0 | 0 |
| CC of Navarre | 3 (1) | 5 (2) | 3 (100) | 5 (100) | 0 | 0 | 3 (100) | 3 (60) | 0 | 0 | 3 (100) | 3 (60) | 0 | 0 |
| Basque Country | 26 (7) | 22 (7) | 26 (100) | 17 (77) | 4 (15) | 4 (18) | 24 (92) | 21 (95) | 24 (92) | 21 (95) | 0 | 0 | 0 | 0 |
| La Rioja | 2 (1) | 0 | 0 | – | 1 (50) | – | 2 (100) | – | 2 (100) | – | 0 | – | 0 | – |
| Total | 353 | 329 | 126 (36) | 164 (50) | 72 (20) | 54 (16) | 297 (84) | 291 (88) | 274 (78) | 279 (85) | 15 (4) | 7 (2) | 8 (2) | 5 (2) |
| 682 P=.950 | 290 P=.002 | 126 P=.181 | 588 P=.102 | 553 P=.016 | 22 P=.087 | 13 P=.334 | ||||||||
“Elective” passive cooling refers to prescription of passive TH for 3 days in whichever hospital the patient is without transferring the patient to a hospital offering active TH once the patient is stable; if the reason for passive cooling was that the patient was too unstable for transport, the data were added to the corresponding column.
Data expressed as n (%). The percentages in each column are calculated relative to the “number of diagnoses” column. We did not have data for Cantabria for 2012. The last row (total) shows the data of the ACs for each year and for the 2 years combined. It also shows the p-value resulting from the comparison of the results for 2012 and 2013.
C, community; CC, charted community; Is, islands; P, principality; R, region.
Of the 90 hospitals, 75 reported the number of inborn (delivered at reporting hospital) live NBs of 35 weeks’ or more gestational age, amounting to a total of 372894 live births out of which 406 NBs delivered at 35 or more weeks’ gestational age received a diagnosis of HIE. Based on these data, the incidence of moderate-to-severe HIE was of 1.09 per 1000 live births (95% CI, 0.98–1.20), with no significant difference between the two years under study (1.07 [95% CI, 0.92–1.22] in 2012 versus 1.11 [95% CI, 0.95–1.26] in 2013).
Forty-three percent (290/682) of NBs with moderate-to-severe HIE were born in hospitals currently using TH, with an increase from 36% (126/353) to 50% (164/329) during the period under study (P=.002) (Table 2). All hospitals reported that inter-hospital transport was conducted under passive hypothermia and that in 61% of transfers (55/90), a neonatologist or a team with specialised training was in charge of patient transport (Table 3).
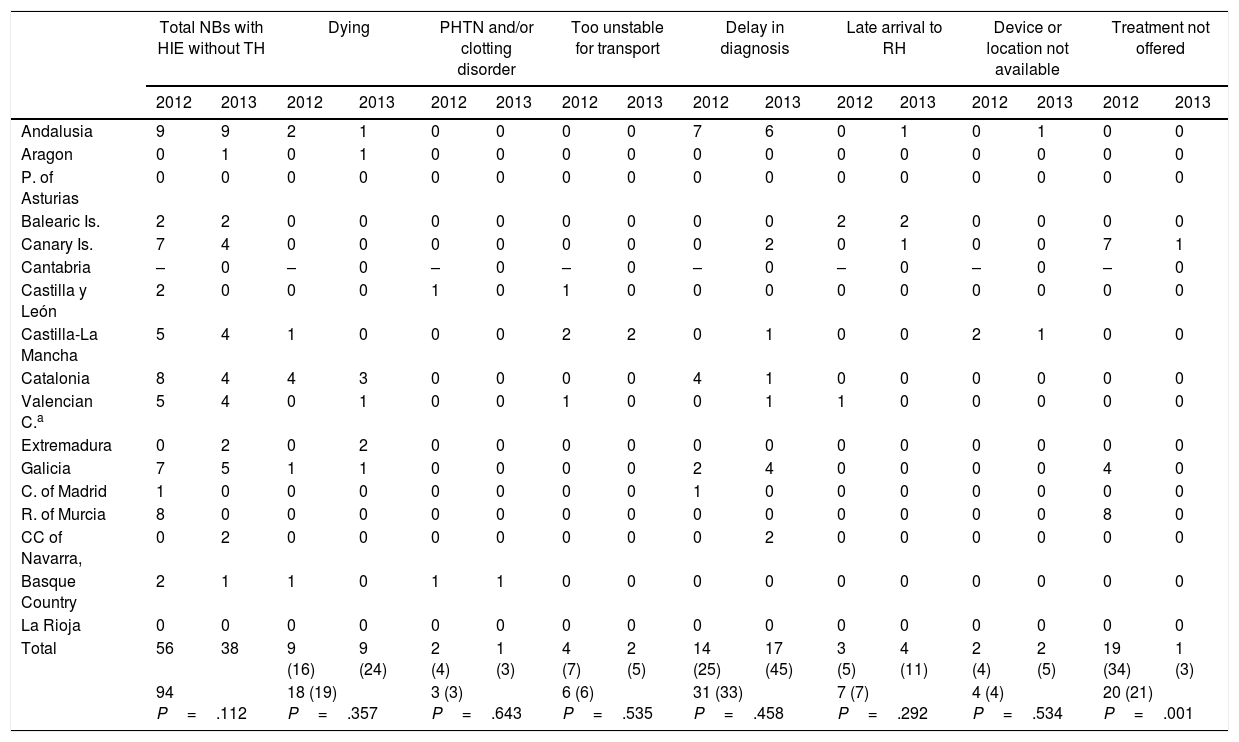
Newborns with moderate-to-severe HIE that did not receive TH (years 2012 and 2013).
| Total NBs with HIE without TH | Dying | PHTN and/or clotting disorder | Too unstable for transport | Delay in diagnosis | Late arrival to RH | Device or location not available | Treatment not offered | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | 2012 | 2013 | |
| Andalusia | 9 | 9 | 2 | 1 | 0 | 0 | 0 | 0 | 7 | 6 | 0 | 1 | 0 | 1 | 0 | 0 |
| Aragon | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| P. of Asturias | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Balearic Is. | 2 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 0 | 0 | 0 |
| Canary Is. | 7 | 4 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 0 | 0 | 7 | 1 |
| Cantabria | – | 0 | – | 0 | – | 0 | – | 0 | – | 0 | – | 0 | – | 0 | – | 0 |
| Castilla y León | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Castilla-La Mancha | 5 | 4 | 1 | 0 | 0 | 0 | 2 | 2 | 0 | 1 | 0 | 0 | 2 | 1 | 0 | 0 |
| Catalonia | 8 | 4 | 4 | 3 | 0 | 0 | 0 | 0 | 4 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
| Valencian C.a | 5 | 4 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 |
| Extremadura | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Galicia | 7 | 5 | 1 | 1 | 0 | 0 | 0 | 0 | 2 | 4 | 0 | 0 | 0 | 0 | 4 | 0 |
| C. of Madrid | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| R. of Murcia | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 0 |
| CC of Navarra, | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 |
| Basque Country | 2 | 1 | 1 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| La Rioja | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Total | 56 | 38 | 9 (16) | 9 (24) | 2 (4) | 1 (3) | 4 (7) | 2 (5) | 14 (25) | 17 (45) | 3 (5) | 4 (11) | 2 (4) | 2 (5) | 19 (34) | 1 (3) |
| 94 P=.112 | 18 (19) P=.357 | 3 (3) P=.643 | 6 (6) P=.535 | 31 (33) P=.458 | 7 (7) P=.292 | 4 (4) P=.534 | 20 (21) P=.001 | |||||||||
Dying refers to NBs with HIE that were born with severe disease and whose vital signs could not be stabilised in the early hours of life, resulting in death.
Data expressed as absolute frequencies and percentages only for total values. Percentages are expressed over the total number of NBs with HIE that were not treated with TH. We did not have data for Cantabria for year 2012. The last row (Total) shows the data of the ACs for each separate year and for the 2 years combined. It also shows the p-values resulting from the comparison of 2012 and 2013.
C, community; CC, charted community; Is, islands; P, principality; PHTN, pulmonary hypertension; R, region; RH, receiving hospital.
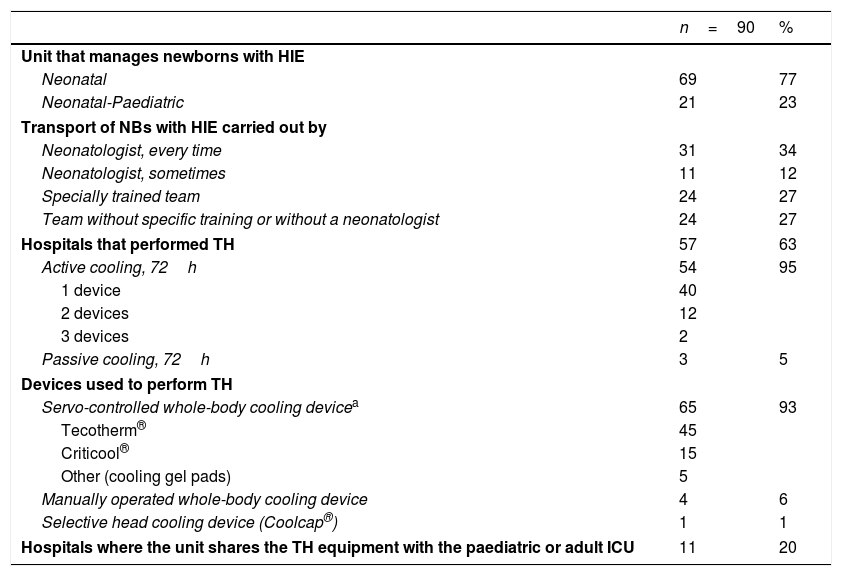
General characteristics of the 90 neonatal units in June 2015.
| n=90 | % | |
|---|---|---|
| Unit that manages newborns with HIE | ||
| Neonatal | 69 | 77 |
| Neonatal-Paediatric | 21 | 23 |
| Transport of NBs with HIE carried out by | ||
| Neonatologist, every time | 31 | 34 |
| Neonatologist, sometimes | 11 | 12 |
| Specially trained team | 24 | 27 |
| Team without specific training or without a neonatologist | 24 | 27 |
| Hospitals that performed TH | 57 | 63 |
| Active cooling, 72h | 54 | 95 |
| 1 device | 40 | |
| 2 devices | 12 | |
| 3 devices | 2 | |
| Passive cooling, 72h | 3 | 5 |
| Devices used to perform TH | ||
| Servo-controlled whole-body cooling devicea | 65 | 93 |
| Tecotherm® | 45 | |
| Criticool® | 15 | |
| Other (cooling gel pads) | 5 | |
| Manually operated whole-body cooling device | 4 | 6 |
| Selective head cooling device (Coolcap®) | 1 | 1 |
| Hospitals where the unit shares the TH equipment with the paediatric or adult ICU | 11 | 20 |
ICU: paediatric intensive care unit.
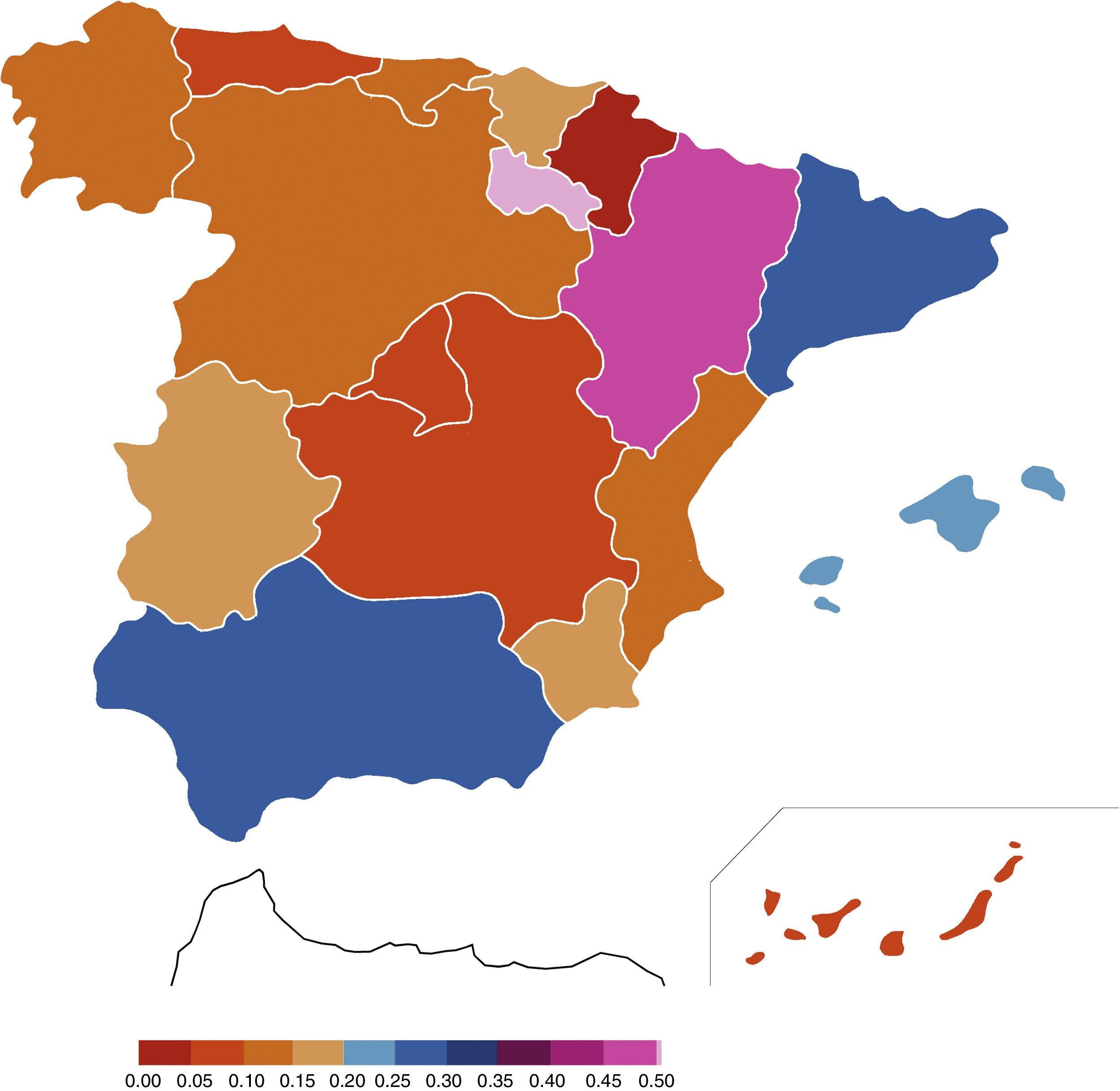
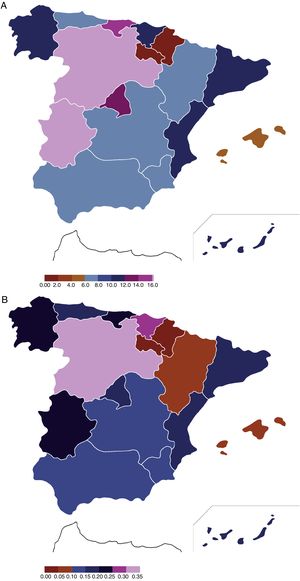
Of the total of 682 NBs with moderate-to-severe HIE, 18% (126/682) died during the neonatal period: 20% (72/353) in 2012 and 16% (54/329) in 2013 (P=.181) (Table 1). These data correspond to a mortality rate due to HIE of 0.14 per 1000 live births (95% CI, 0.12–0.17) in the 2012–2013 period. Table 2 and Fig. 2 show the data broken down by AC, showing the differences between ACs like Catalonia, Andalusia or Aragón, with rates of more than 20%, versus others like Madrid, Castilla-La Mancha, Asturias, Navarre or the Canary Islands, where the proportion of deaths in the population of live NBs with HIE did not exceed 10%.
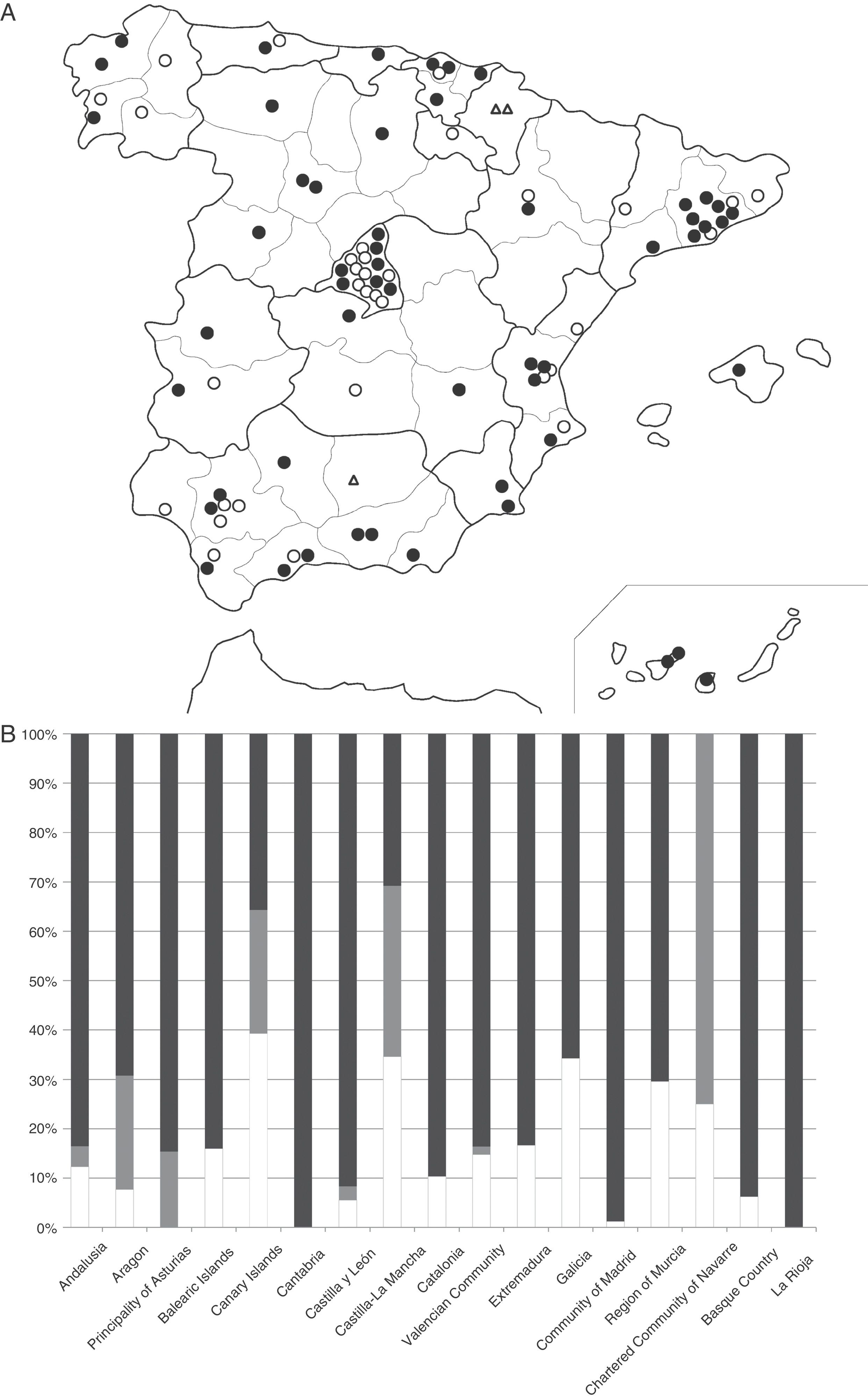
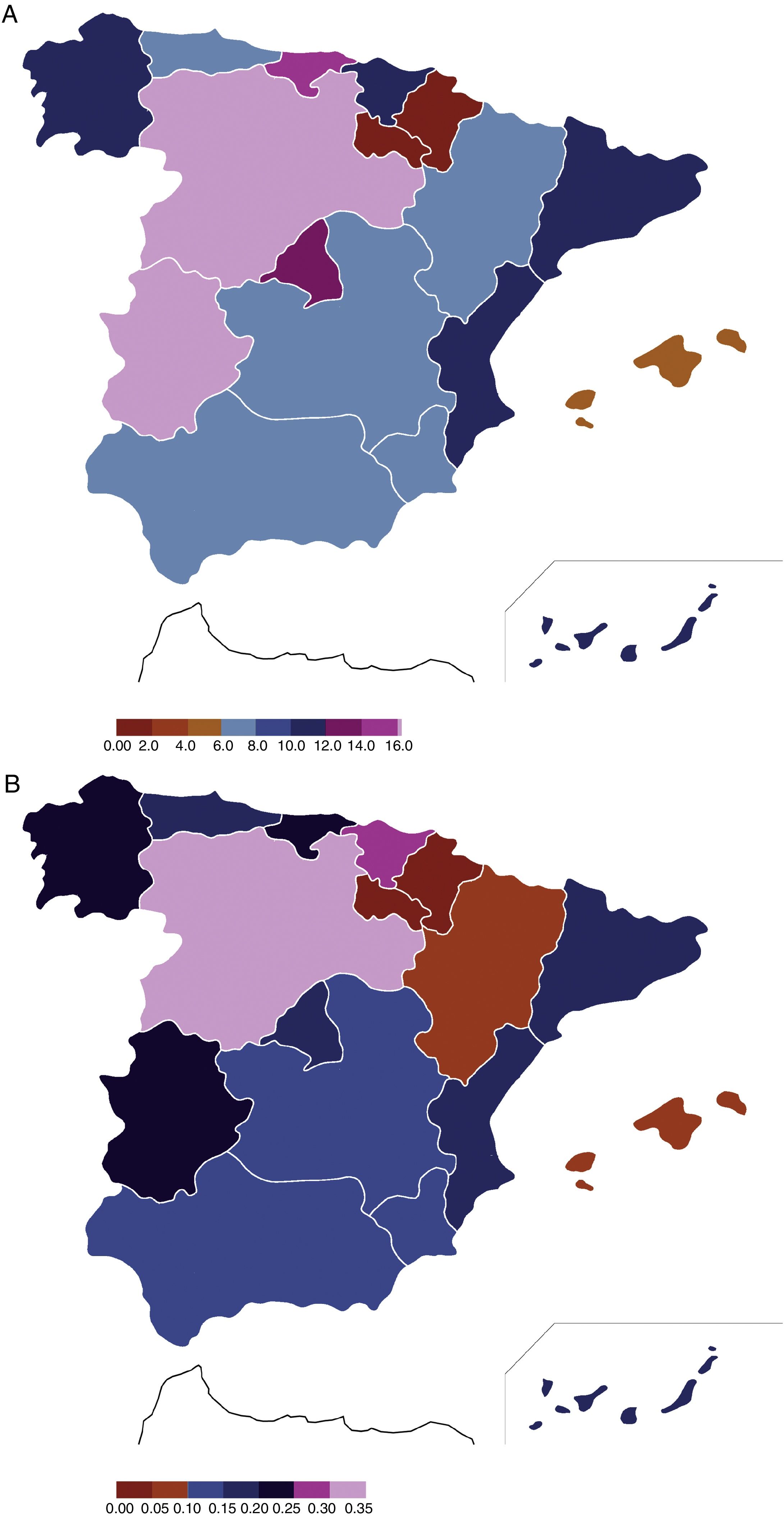
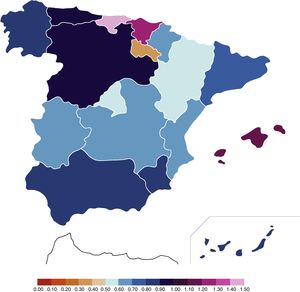
Application of therapeutic hypothermiaThe use of TH in the units grew progressively from its introduction in 2008 to its application in 60% (57/90) of tertiary care hospitals by June 2015 (Fig. 3). Ninety-five percent (54/57) of these hospitals used active HT in the form of servo-controlled whole-body cooling. Only one facility had a device for the selective cooling of the head, in addition to the use of whole-body cooling (Table 3). All ACs but 2 had at least one hospital that practiced active TH, and 26% of neonatal units had more than one device to deliver active TH (Table 1) (Fig. 3). The analysis of the availability of active cooling systems by number of live NBs with moderate-to-severe HIE and by number of live births overall showed an uneven distribution, and Navarre and La Rioja were the ACs with the fewest devices per NB with HIE, followed by Murcia and the Balearic Islands (Fig. 4).
(A) Map showing the 90 hospitals that participated in the survey and their TH capabilities as of June 2015: active TH (solid black circle), passive TH (hollow triangle) or no TH (hollow circle). The autonomous cities of Ceuta and Melilla are not represented because they did not participate in the survey, since none of their hospitals have level III neonatal units and they refer patients requiring this level of care to hospitals in the Iberian peninsula. The progressive increase in the number of hospitals offering TH after its initial introduction in 2 centres in 2008 was of 10 hospitals in 2009, 9 hospitals in 2010, 10 hospitals in 2011, 9 hospitals in 2012, 7 hospitals in 2013, 8 hospitals in 2014 and 2 hospitals in 2015. (B) Distribution of NBs with a moderate-to-severe HIE diagnosis that received TH in the period under study by AC. Dark grey represents children that received active TH, light grey children that received passive TH, and while children that did not receive TH.
Distribution of the number of active cooling systems available as of June 2015 relative to (A) the number of live NBs with moderate-to-severe HIE and (B) the total number of live births; 2012–2013.
In A, data are expressed as number of TH devices/NBs of moderate-severe HIE×1000.
In B, data are expressed as number of TH devices/live births×1000.
In the period under study, 86% (588/682) of NBs with moderate-to-severe HIE received TH, a proportion that increased from 84% in 2012 to 88% in 2013 (P=.102), with an increase in the proportion of NBs treated with active cooling from 78% in 2012 (274/353) to 85% in 2013 (279/329) (P=.01) (Table 1). The distribution by AC showed that active cooling was offered the least in the Canary Islands, Castilla-La Mancha and Navarre (Fig. 3). Six percent of the NBs that received TH (35/588) were treated with passive cooling, with the proportion treated with this method decreasing from 8% in 2012 (23/297) to 4% in 2013 (12/291) (P=.089). This decrease corresponded to a reduction by half in the number of NBs treated for no apparent reason with passive cooling as opposed to being transferred to a hospital offering active cooling (Table 1).
Fourteen percent of NBs with HIE (94/682) did not receive TH. If we exclude the 21 NBs that may not have been eligible because they were dying, had pulmonary hypertension and/or a severe clotting disorder, 11% of NBs with HIE (73/682) were not treated with cooling. The most frequent reasons for this were delay in diagnosis or hospital transfer in 31 cases and TH not being prescribed in 20 patients (a number that decreased from 19 in 2012 to 1 in 2013; P=.001) (Table 2).
DiscussionThis study is the first to describe the incidence of HIE and the use of TH in Spain. These data are needed to understand the frequency and management of HIE in current clinical practice, propose strategies for improvement, and plan policies aimed at reducing the impact of HIE on future health. Data for entire national populations are scarce in the literature, probably due to the intrinsic difficulty of obtaining information from hospitals that manage NBs with HIE according to a homogeneous definition.9,10,12 This is one of the strengths of our study, as we succeeded in obtaining data from every level III neonatal unit in Spain applying a uniform definition of moderate-to-severe HIE.
Incidence of hypoxic-ischaemic encephalopathy in Spain and by autonomous communityThe incidence rate was consistent with those reported in single-centre studies conducted in Madrid and Barcelona and in a population-based multicentre study conducted in Castilla y León.19–21 The overall incidence of HIE (mild, moderate or severe) in developed countries ranges between 1 and 8 per 1000 live births, and reported rates vary according to the type of study (single-centre, multicentre or population-based) and especially to the operational definition of HIE.22 A review that included 40 studies conducted in 26 European countries and the United States between 1980 and 2013 reported a mean incidence rate of 1.6 per 1000 live NBs delivered at term (range, 0.68–3.75), with the proportion of moderate-to-severe HIE estimated at 60% of the total cases of HIE.1 However, since HIE must be graded in the first hours of life to determine the suitability of TH, we need data on the incidence of HIE at this age. We have not found any other population-based study of moderate-to-severe HIE diagnosed in the first 6 hours of life, information that is essential for the purpose of assessing the health care needs of this population. Our data provide a more accurate picture of the epidemiological situation of HIE, as our study included NBs with HIE delivered between 35 and 37 weeks’ gestation, the population subset currently considered eligible for TH.11,19–21,23
When it came to the distribution by AC, we found considerable homogeneity, the incidence was similar in all of them, although given the nature of the study we cannot be certain that grading was correctly done by all centres. For example, several case have reported that up to 20% of NBs with mild HIE are treated with TH.9,16,23,24 However, it is very likely that the severity criteria applied throughout Spain were very homogeneous, where there are clear national guidelines.17
Nationwide application of therapeutic hypothermiaThe use of this therapeutic intervention in Spain has not been introduced following a structured territorial plan, but rather on the initiative of individual neonatologists with the support of the administration of their corresponding hospitals. All participating hospitals had servo-controlled whole-body cooling devices, which have been demonstrated to successfully maintain a stable body temperature without fluctuations.12,25 The proportion of NBs with moderate-to-severe HIE treated with TH (86%) was higher compared to the proportions reported in other countries,10,14 and the use of passive cooling was minimal by the end of the study period (4%). Although good outcomes have been reported with the use of passive TH16 and there are situations where patients are severely unstable and cannot be transported to a hospital equipped to provide active TH, servo-controlled cooling systems offer unquestionable advantages.12,23,25
Another relevant finding in our study was the improvement in the use of TH between 2012 and 2013, which the number of eligible NBs that did not receive this treatment declining from 16% to 12%. This proportion is below those reported in other case series, which can be as high as 35%.10,14,15,26 The reduction in the number of NBs that were not offered this treatment for no apparent reason was particularly significant. Although our study did not allow for the identification of the factors that led to the rapid spread in the use of this treatment, we believe that in addition to the scientific evidence on its efficacy,2,3 the recommendations published by the SENeo17 and the courses or educational programmes specifically focused on the comprehensive management of newborns with HIE20,27 may have contributed to this development.
However, we did not find any improvement in the most frequent reason that HT is not given: a delay in the diagnosis of HIE or in the transfer to a hospital equipped to provide TH.9–11,28 More than half of the NBs with HIE were born in hospitals that did not provide TH, so in order to reduce the number of NBs with moderate-to-severe HIE that do not receive TH in Spain, it is necessary that: (1) hospitals that do not offer TH train their staff to identify NBs with HIE and develop specific protocols for patient stabilisation and safe implementation of passive cooling until the time of transport; transfer in these cases must be considered urgent, but it is possible to delay it a few hours to stabilise the patient, maintaining a stable body temperature of 33–34°C through passive cooling,15,29 and (2) transfer to the referral hospital is carried out under appropriate conditions. Although our study did not analyse the efficacy and safety of patient transport, we found that in a considerable number of instances, transport was carried out by teams without specific training. This underscores the need to have well-trained and specialised teams available in each AC in order to maximise patient safety and maintain body temperature within the therapeutic range, avoiding temperature fluctuations and, above all, overcooling.30,31 An analysis by AC of the travel times and distances from the referring hospital to the receiving hospital may evince the need for portable servo-controlled devices for transport, especially in those ACs where travel times may be long or transfers delayed.
The map of the distribution of hospitals that can provide this treatment in Spain reveals some inequality between ACs and shows those where TH was offered less frequently and should strive to rise to the average standard to improve health care equity. On the other hand, our study also revealed significant differences in the availability of cooling devices. While a large number of devices fitting the number of diagnosed cases of HIE were available in Madrid and Catalonia, there were significant differences between ACs, with some better equipped, like Castilla y León, compared to others like Castilla-La Mancha, Andalusia or Aragón. The differences between ACs in size and in the travel distances to referral hospitals call for alternative solutions, such as collaboration between neighbouring ACs, to develop feasible plans to provide health care to these patients. While another option would be to increase the number of hospitals that offer TH, given the low incidence, complexity of care and need for a multidisciplinary approach in HIE, where TH is but one of the essential elements of care,32 it would be more practical to centralise the management of these infants in hospitals that offer comprehensive multidisciplinary care.7,14,33,34
Mortality due to hypoxic-ischaemic encephalopathyThe mortality due to moderate-to-severe HIE in the 2012–2013 period (18%) was similar to the mortality reported in other case series, which ranges between 15% and 20%,9,10,16,24,26,29 although it was clearly lower than the mortality reported in other studies that estimate it at 27–35%11,19–21 and the 26% mortality reported by the initial clinical trials of TH.2 A recent literature review1 reported an overall neonatal mortality attributable to HIE in countries of similar characteristics to those of Spain of 10% (7.9–11.9%), although the calculation did not include deaths that occurred minutes or hours after birth that are mainly due to perinatal hypoxic-ischaemic episodes. If we were to exclude the group of NBs that die within a few hours of birth from the calculation in our study, the mortality would be 16%, close to the figures reported by Lee et al.1
It is known that most deaths due to HIE take place after end-of-life decisions that include withdrawal of life support.35 Due to the nature of our study, we were unable to determine whether there were differences between hospitals and ACs in this regard or whether the observed differences in mortality were mainly due to differences in HIE severity, but there was considerable variability in mortality between ACs, as some had hospitals reporting mortalities of less than 10% and others hospitals reporting mortalities of more than 20%.
There are some limitations to our study. Although this type of study can provide evidence on actual clinical practice outside the narrow framework of clinical trials,13,23,29,36 its retrospective nature and design (survey) carry a risk of bias, as the collected data may be incomplete or inaccurate. Although there is a possibility that our study underestimated or overestimated the incidence of HIE, we believe this is unlikely, as we obtained responses from every tertiary care centre that may or may not offer TH and that manage NBs with moderate-to-severe HIE, either inborn or transferred from lower-level health care facilities. Furthermore, we carefully reviewed the data submitted by the hospitals that received transferred patients and compared them to the data reported by the referring hospitals in each AC. On the other hand, it is possible that other hospitals have introduced active cooling in the months that elapsed since the survey was completed.
In conclusion, the incidence of moderate-to-severe HIE was similar across ACs. The data of our survey reflect significant progress in the use of TH since its initial introduction in 2008, as nearly 90% of NBs with moderate-to-severe HIE now receive this treatment. Although these findings are encouraging, there are still many areas for improvement, including reducing the unequal distribution of hospitals that can provide TH between ACs, the development of recommendations and specific multicentre programmes for the provision of comprehensive care for HIE involving referring and receiving hospitals and transport teams, and auditing of health care processes and outcomes.
Conflicts of interestThe authors have no conflicts of interest to declare
Neonatal units. Tertiary care hospitals, Spain: J. Diez-Delgado (Torrecárdenas, Almería), I. Tofé (Reina Sofía, Córdoba), A.E. Jerez (S. Cecilio, Granada), J.A. Hurtado (Virgen de las Nieves, Granada), J.M. Ceballos (J.R. Jiménez, Huelva), M.L. Millán (C. Hospitalario, Jaén), M.D. Esquivel (Materno-Infantil, Jerez), C. Ruiz (Costa del Sol, Marbella), M. Baca (Quirón, Malaga), E. Tapia (General Universitario, Malaga), M. Losada (Quirón, Sagrado Corazón, Seville), E. Torres (Valme, Seville), A. Pavón (Virgen del Rocío, Seville), P.J. Jiménez (Virgen Macarena, Seville), F. Jiménez (S. Ángela de la Cruz, Seville), M.P. Ventura (Lozano Blesa, Zaragoza), S. Rite (Miguel Servet, Zaragoza), T. González (Cabueñes, Gijón), R.P. Arias (Central Asturias, Oviedo), P.R. Balliu (Son Espases, Majorca), J.M. Lloreda-García (S. Lucía, Cartagena), J.L. Alcaráz (Virgen de la Arrixaca, Murcia), C. Tapia (General, Alicante), A. de la Morena (S. Juan, Alicante), I. Centelles (General, Castellón), I. Güemes (Casa de Salud, Valencia), J. Estañ (Clínico, Valencia), A. Alberola (La Fe, Valencia), S. Aparici (Quirón, Valencia), R. López (Nisa-9 de Octubre, Valencia), J. Beceiro (Príncipe de Asturias, Alcalá de Henares), B. García (General, Fuenlabrada), L. Martínez (General, Getafe), E. González (Severo Ochoa, Leganés), L. Arruza (Clínico San Carlos, Madrid), M.D. Blanco (Gregorio Marañón, Madrid), B. Arias (La Zarzuela, Madrid), F. Mar (Ruber Internacional, Madrid), J. Jiménez (Sanitas-La Moraleja, Madrid), G. Romera (Montepríncipe, Madrid), A. Cuñarro (Alcorcón), C. Muñóz (Puerta de Hierro-Majadahonda, Madrid), F. Cabañas (Hospital Universitario Quirón Madrid), R. Montero (Nisa-Pardo de Aravaca, Madrid), J.C. Tejedor (General, Móstoles), C. Santana (Materno Insular, Las Palmas), B. Reyes (Universitario de Canarias, Tenerife), S. Romero (N.S. de Candelaria, Tenerife), A. Orizaola (Marqués de Valdecilla, Santander), M. Baquero (General, Albacete), D. Hernández (General, Ciudad Real), A. Pantoja (Virgen de la Salud, Toledo), C. Vega (HUBU, Burgos), L. Castañón (CAULE, León), E.P. Gutiérrez (Universitario, Salamanca), M. Benito (Clínico, Valladolid), M.J. García (Santa Creu i Sant Pau, Barcelona), M.A. López-Vílchez (Hospital del Mar, Barcelona), L. Castells (General de Catalunya, Barcelona), M. Domingo (Parc Taulí, Sabadell), W. Coroleu (Germans Trias i Pujol, Badalona), H. Boix (Vall d’Hebron, Barcelona), R. Porta (Instituto Dexeus-Quirón, Barcelona), S. Martínez-Nadal (SCIAS, Barcelona), E. Jiménez (Dr. J. Trueta, Girona), E. Sole (Arnau de Vilanova, Lleida), M. Albújar (Joan XXIII, Tarragona), E.M. Fernández (Infanta Cristina, Badajoz), A.R. Barrio (S. Pedro de Alcántara, Cáceres), E. Piñán (Mérida), A. Avila-Alvarez (CHU A Coruña), M.E. Vázquez (Lucus Augusti, Lugo), N. Balado (CHU, Orense), P.A. Crespo (CHU, Pontevedra), M.L. Couce (Clínico, Santiago de Compostela), A. Concheiro-Guisán (Xeral, Vigo), I. Esteban (S. Pedro, Logroño), A. Lavilla (CH, Navarra), V. Alzina (C. Universidad de Navarra), A. Aguirre (Basurto, Bilbao), B. Loureiro (Cruces, Bilbao), I. Echániz (Quirón, Bilbao), M.D. Elorza (H.U. Donostia, San Sebastián), A. Euba (HUA Txagorritxu, Vitoria).
Please cite this article as: Arnaez J, García-Alix A, Arca G, Valverde E, Caserío S, Moral MT, et al. Incidencia de la encefalopatía hipóxico-isquémica e implementación de la hipotermia terapéutica por regiones en España. An Pediatr (Barc). 2018;89:12–23.
The members of the Working Group on HIE-Spain (EHI-ESP) are listed in Appendix A.
Previous presentations: XVIII Curso de Excelencia en Pediatría “Actualización en Neonatología.” March 2015; Zamora, Spain. XXV Congreso de Neonatología y Medicina Perinatal de la Sociedad Española de Neonatología. May 2015; Seville, Spain.