Magnesium sulphate (MgSO4) therapy has shown to be useful as a neurological protector in the preterm newborn below 32 weeks of gestation. The most documented adverse effect is cardiorespiratory failure, whereas its relationship with meconium obstruction is controversial. The main objective of this study was to analyse the possible association between prenatal MgSO4 therapy and meconium obstruction.
Patients and methodsAn analytical retrospective study was conducted on <32 weeks preterm babies admitted to a tertiary-level hospital (January 2016–December 2017). Epidemiological, prenatal and postnatal data on the outcomes were obtained, analysed and compared in both groups (exposed to MgSO4 and not exposed).
ResultsThe study included 201 patients (146 exposed and 55 non-exposed). There were no significant differences in the mean gestational age (28.4 ± 2.2 vs. 28.7 ± 2.8 weeks, respectively), or in the rest of epidemiological and perinatal variables. Prenatal corticosteroid therapy was more frequent in the MgSO4 group (75.9 vs. 53.7%; p = .002), and in the non-exposed group there were more multiple pregnancies (52.7 vs. 36.6%; p = .027), and female gender (56.4 vs. 37%; p = .013). There were no statistically significant differences in the presence of meconium obstruction (75.9% in exposed vs. 67.3% in non-exposed; p = .23), although repeated rectal stimulation was more frequent in the exposed group (43.2 vs. 27.9%; p = .08). Furthermore, there were no significant differences in the main cardiorespiratory variables: 1-min Apgar score (6.2 in MgSO4− exposed vs. 5.6 in non-exposed; p = .75), 5-min Apgar score (7.9 vs. 7.6; p = .31), advanced newborn resuscitation (26 vs. 31.5%; p = .44), maximum FiO2 (45.5 vs. 48; p = .58), and initial inotropic requirements (10.3 vs. 20.8%; p = .55).
ConclusionsThis study found no correlations between MgSO4 therapy and meconium obstruction or cardiorespiratory failure.
El sulfato de magnesio (SMg) ha demostrado eficacia como neuroprotector en pretérminos < 32 semanas. Su efecto adverso más documentado es la depresión cardiorrespiratoria, siendo dudosa su relación con la obstrucción meconial. El objetivo principal del estudio es analizar la posible asociación entre el SMg antenatal y la obstrucción meconial.
Pacientes y métodosEstudio retrospectivo analítico, de neonatos < 32 semanas de edad gestacional ingresados en un hospital terciario (enero del 2016 a diciembre del 2017). Se recogieron datos epidemiológicos, perinatales y de evolución posnatal, comparando expuestos y no expuestos a SMg.
ResultadosSe incluyeron 201 pacientes (146 recibieron SMg y 55 no). No existieron diferencias en la edad gestacional media (28,4 ± 2,2 vs. 28,7 ± 2,8 semanas, respectivamente) ni el resto de variables epidemiológicas y perinatales, salvo en expuestos la administración más frecuente de corticoides antenatales (75,9 vs. 53,7%; p = 0,002), y en no expuestos el parto múltiple (52,7 vs. 36,6%; p = 0,027), y el sexo femenino (56,4 vs. 37%; p = 0,013). No hubo diferencias significativas en la obstrucción meconial (75,9% expuestos vs. 67,3% no expuestos; p = 0,23), aunque la estimulación rectal repetida fue más frecuente en el grupo tratado (43,2 vs. 27,9%; (p = 0,08). Tampoco hubo diferencias en las principales variables de depresión cardiorrespiratoria: Apgar al primer minuto 6,2 vs. 5,6 en expuestos y no expuestos respectivamente (p = 0,75) y a los cinco minutos 7,9 vs. 7,6 (p = 0,31), reanimación avanzada 26 vs 31,5% (p = 0,44), FiO2 máxima 45,5 vs. 48 (p = 0,58) y necesidad inicial de inotrópicos 10,3 vs 20,8% (p = 0,55).
ConclusionesEl presente estudio no halló asociación entre la administración de SMg y la obstrucción meconial o la depresión cardiorrespiratoria.
Magnesium sulphate (MgSO4) is a mainly intracellular cation that can depress neuronal excitability and neuromuscular transmission used widely in medicine.1 Its mechanism of action has not been fully established,2,3 although several hypotheses have been proposed to explain its different effects. Among other indications, it is used for treatment of arrhythmias,1 severe asthma exacerbations4 or electrolyte abnormalities.1 At present, in the field of obstetrics, it is mainly used for prophylaxis or treatment of maternal seizures associated with preeclampsia (having proved superior to diazepam and phenytoin5–8) and for neuroprotection of infants in gestations of 24–31+6 weeks’ duration in the case of risk of imminent birth or the need for induction of labour within 24 h for reasons related to the mother or the foetus, as it has been proven to reduce the incidence and severity of cerebral palsy in preterm (PT) infants.3,6
The adverse effects on the mother have been well documented. Most are minor (vomiting, redness, dizziness), although severe effects have also been reported, such as respiratory failure, cardiac failure or death, which are rare and usually associated with significant elevation of magnesium serum levels.5 However, the safety profile of the antenatal use of MgSO4 in preterm infants is still unclear and there are few published data on the subject.5,9 There is evidence suggesting that maternal exposure to MgSO4 may be associated with an increased risk of neonatal complications, some of which are better documented, such as respiratory or central nervous system (CNS) depression, and others for which there is little published data that may also be contradictory, for instance intestinal obstruction caused by meconium.10,11
Although in adults hypermagnesemia is associated with paralytic ileus,12 there is still uncertainty regarding the association between antenatal exposure to MgSO4 and delayed passage of meconium, meconium plug syndrome and spontaneous intestinal perforation,13,14 with few sources on the subject.13
The primary objective of our study was to analyse the potential association of antenatal administration of MgSO4 for neuroprotection in PT infants and the development of meconium obstruction. The secondary objective was to assess the potential role of MgSO4 in respiratory depression at birth.
Sample and methodsWe conducted a retrospective, descriptive and analytical study including all neonates delivered before 32 weeks’ gestation and admitted between January 1, 2016 and December 31, 2017 to the Hospital General Universitario Gregorio Marañón. We excluded infants with major congenital anomalies. The study was approved by the Research Ethics Committee.
In the sample size calculation, we estimated that a sample of 201 patients could detect significant differences of at least 23% (28%–55%) with a power 81% and an alpha level of 0.05.
We collected epidemiological data regarding the gestation and perinatal periods and data on clinical outcomes and laboratory results of the infants in the first week of life. We compared these variables in infants exposed to MgSO4 and infants that were not exposed.
The administration of MgSO4 to pregnant women adhered to the protocol of the hospital, which was based on the recommendations of the Sociedad Española de Ginecología y Obstetricia (Spanish Society of Gynaecology and Obstetrics, SEGO): a loading dose of 4 g delivered over 5−20 min, followed by a maintenance dose of 1–2 g per hour delivered intravenously.
We defined meconium obstruction as delayed passage of meconium of at least 48 h and/or need of repeated rectal stimulation to achieve a bowel movement and/or an interval of 48 or more hours between the first and second bowel movements. We defined repeated rectal stimulation as 2 or more digital stimulations, performed based on the judgment of the physician/nurse in the absence of spontaneous passage of meconium and/or presence of clinical manifestations such as abdominal distension or discomfort. The impact of obstruction was described in terms of the time elapsed to initiation of enteral nutrition (EN), time elapsed to discontinuation of parenteral nutrition (PN) or development of necrotising enterocolitis (NEC).
The variables used to analyse respiratory depression were the Apgar score at birth, type of resuscitation and maximum fraction of inspired oxygen (FiO2) used in the delivery room, acidosis and need of inotropic drugs in the first hours post birth.
In the statistical analysis, we summarised categorical data as percentages and quantitative data as mean and standard deviation (SD) or median and interquartile range, depending on whether the data followed a normal distribution. We compared categorical variables with the χ2 test or Fisher exact test, and quantitative data with the Student t test or the Mann–Whitney U test depending on the distribution. We considered p-values of less than 0.05 statistically significant. The analysis was performed with the statistical software SPSS, version 22 (IBS SPSS Statistics, 2013; IBM Corp.; Armonk, NY, USA).
ResultsBetween January 2016 and December 2017, a total of 219 infants were born preterm before 32 weeks’ gestation. We included 201 patients (146 whose mothers received MgSO4 and 55 whose mothers did not), excluding those with major malformations.
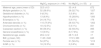
Table 1 summarises the main maternal, obstetric and infant-related variables. The salient characteristics were a higher frequency of multiple gestation and maternal hypothyroidism and lower frequency of antenatal steroid therapy in the group not exposed to MgSO4. When it came to infant characteristics, we only found significant differences in sex between the groups, with a higher frequency of female infants in the group not exposed to MgSO4.
Baseline characteristics of the sample.
| MgSO4 exposure (n = 146) | No MgSO4 (n = 55) | p | |
|---|---|---|---|
| Maternal age, years (mean ± SD) | 32.5 ± 6.3 | 33 ± 4.9 | .672 |
| Multiple gestation (n, %) | 52 (36.6%) | 29 (52.7%) | *.027 |
| Gestational diabetes (n, %) | 9 (6.3%) | 3 (5.8%) | .901 |
| Hypothyroidism (n, %) | 13 (8.9%) | 15 (28.8%) | *.000 |
| Eclampsia (n, %) | 24 (16.7%) | 5 (9.1%) | .176 |
| Antenatal steroids (n, %) | 110 (75.9%) | 29 (53.7%) | *.002 |
| Chorioamnionitis (n, %) | 18 (12.5%) | 5 (9.1%) | .501 |
| Caesarean section (n, %) | 86 (59.3%) | 32 (59.3%) | .995 |
| General anaesthesia (n, %) | 13 (9.5%) | 8 (17.8%) | .131 |
| Gestational age, weeks | 28.4 ± 2.2 | 28.7 ± 2.8 | .17 |
| BW, g (mean, SD) | 1145 ± 348 | 1172 ± 383 | .643 |
| Female sex (n, %) | 54 (37%) | 31 (56.4%) | *.013 |
| IUGR (n, %) | 18 (12.3%) | 2 (3.6%) | .066 |
BW, birth weight; IUGR, intrauterine growth restriction; MgSO4, magnesium sulphate; SD, standard deviation.
Gestational diabetes: diabetes newly diagnosed during pregnancy (basal glucose ≥126 mg/dL on 2 different days or ≥200 mg/L or abnormal glucose tolerance test). Eclampsia: development of grand mal seizures in a pregnant woman with preeclampsia that cannot be attributed to other causes. Intrauterine growth restriction: estimated foetal weight (EFW) <3rd percentile, or EFW <10th percentile and abnormal cerebral-umbilical flow or uterine arterial flow).
We did not find differences in the frequency of meconium obstruction or the time elapsed between the first and second bowel movement, the hours to initiation of EN or the time to attainment of full EN. There were also no differences in the incidence of NEC or the time of NEC development. Although the difference was not statistically significant, we found a greater probability of requiring repeated rectal stimulation to trigger a bowel movement in the group exposed to MgSO4 (43.2% vs. 27.9% in the group without MgSO4 exposure; p = .08) (Table 2).
Association of magnesium sulphate with paralytic ileus and respiratory depression. Outcome variables.
| MgSO4 exposure (n = 146) | No MgSO4 (n = 55) | p | |
|---|---|---|---|
| Length of stay, days (mean, SD) | 102 ± 7.8 | 90 ± 12.8 | .431 |
| Death (n, %) | 17 (11.6%) | 9 (16.4%) | .374 |
| Meconium obstruction (n, %) | 105 (75.9%) | 35 (67.3%) | .23 |
| Meconium passage >48 h post birth (n, %) | 52 (28%) | 17 (34%) | .62 |
| Repeated need for rectal stimulation to start bowel movements (n, %) | 41 (43.2%) | 12 (27.9%) | .08 |
| Time between bowel movements >48 h (n, %) | 62 (51.2%) | 19 (43.2%) | .36 |
| Hours from birth to initiation of enteral nutrition (mean, SD) | 30.6 ± 1.8 | 31.6 ± 3.8 | .81 |
| Days from birth to full enteral nutrition (mean, SD) | 10.7 ± 0.9 | 11.6 ± 1.6 | .21 |
| NEC (n, %) | 26 (17.8%) | 15 (27.3%) | .12 |
| Days from birth to NEC (mean, SD) | 14, ± 2 | 12.8 ± 1.9 | .5 |
| 1-min Apgar (mean, SD) | 6.2 ± 1.9 | 5.6 ± 2 | .75 |
| 5-min Apgar (mean, SD) | 7.9 ± 1.4 | 7.6 ± 1.5 | .31 |
| NALS (n, %) | 38 (26%) | 17 (31.5%) | .44 |
| pH in first blood gas analysis (mean, SD) | 7.26 ± 0.01 | 7.25 ± 0.1 | .87 |
| Lactate in first blood gas analysis (mean, SD) | 2.86 ± 1.9 | 2.83 ± 1.8 | .5 |
| Maximum FiO2 in delivery room (mean, SD) | 45.5 ± 2.1 | 48 ± 4.2 | .58 |
| Inotropic drugs within 72 h of birth (n, %) | 15 (10.3%) | 11 (20.8%) | .55 |
FiO2, fraction of inspired oxygen; NALS, neonatal advanced life support (type 4: orotracheal or nasotracheal intubation; type 5: cardiac massage); NEC, necrotising enterocolitis (diagnosed and graded based on clinical, imaging and laboratory features); SD, standard deviation.
When it came to perinatal respiratory depression, we did not find statistically significant differences between groups in any of the variables under study (Table 2).
DiscussionIn the past decade, MgSO4 has been included in international guidelines for antenatal neuroprotection of PT infants. The impact on the neonate and its safety profile in PT infants have not been well established, and there are few sources on the subject in the medical literature.5,9 In this context, our study contributes information on the potential effects at the intestinal level of antenatal MgSO4 exposure in PT newborn infants.
The potential increase in the incidence of meconium obstruction is a controversial hypothesis that has rarely been addressed in the literature. To complicate matters further, although meconium obstruction of prematurity has been described with growing frequency in recent decades,15 there is no definitive consensus on the criteria to be used for its diagnosis. In our study, we defined meconium obstruction based on the existing literature.15–17
Our study did not evince differences in the incidence of meconium obstruction based on antenatal exposure to MgSO4. In this regard, the results of the studies published to date have been contradictory. In 1972, Sokal et al. described the cases of 2 neonates with antenatal exposure to MgSO4 and absence of passage of meconium in the first 24 h post birth associated with abdominal dissension and vomiting. Both patients had been born after 35 weeks of gestation and had elevated serum levels of magnesium. None of the other 10 infants with hypermagnesemia in the study developed abdominal distension, although they had lower serum levels of magnesium.18 Since then, different studies have tried to establish the association between these 2 events, with results that were either not statistically significant19,20 or inconclusive.16 Cuenca et al.16 conducted a retrospective study of several factors associated with meconium obstruction, including antenatal treatment with MgSO4. The study included 61 newborn infants with a diagnosis of meconium obstruction, of who 16% had a known history of antenatal MgSO4 exposure. However, since the median gestational age of the sample was 35 weeks, it is not possible to compare these results to those in our sample. We did not find any other studies on the association of a meconium obstruction diagnosis and antenatal neuroprotection with MgSO4.
However, there are some articles analysing the variables used to define meconium obstruction. One of the variables that we analyse in the study was delayed passage of meconium, beyond 48 h post birth, and did not find significant differences between groups. Although the association is not well established, some authors have found an association between antenatal exposure to MgSO4 and delayed passage of meconium. Riaz et al.21 published one of the few studies on the subject. They reported delayed passage of meconium in 38% of neonates with hypermagnesemia compared of 15% of controls, although the difference was not statistically significant. A more recent study13 compared prospective data for 56 PT infants born before 32 weeks’ gestation exposed antenatally to MgSO4 for neuroprotection to data for 51 historical controls. The authors found a higher frequency of delayed passage of meconium in the exposed group (9.6 vs. 2% in the control group), a difference that was not significant. On the other hand, unexpectedly, they found that in the subset of infants born before 30 weeks, a higher proportion in the group exposed to MgSO4 passed meconium within 48 h of birth compared to the control group. In our study, we did not a subgroup analysis of infants delivered before 30 weeks, but we did not find that difference in the total sample of preterm infants delivered before 32 weeks, with the first meconium passage occurring before 48 h post birth in 72% of the MgSO4 group vs 66% of the control group (p = .62).
Gursoy et al.20 analysed the impact of antenatal MgSO4 exposure in intestinal blood flow in PT newborns, and found a similar mesenteric flow in both groups and no difference in the time of the first bowel movement. However, the authors noted that drawing conclusions was difficult, as the only variable that was documented was the time of the first meconium passage, without taking into account other parameters involved in bowel transit.
We also found no differences in the proportion of infants with an interval greater than 48 h between the first and second bowel movements. We found a greater proportion that required rectal stimulation to initiate a vowel movement in the MgSO4 group, although this difference was not statistically significant. To our knowledge, there are no other studies in the literature that analysed these variables.
We also analysed the association between MgSO4 exposure and feeding. In this regard, we also found no significant differences in the time to initiation of EN or to full EN. These findings were consistent with those of Gursoy et al.,20 who also reported no differences in the time to achievement of exclusive EN.
Last of all, as concerns the potential intestinal complications associated with MgSO4, we compared the incidence of NEC in the two groups and did not find differences. Other studies have not found an association between antenatal MgSO4 and NEC.22 Downey et al. analysed the incidence of NEC and isolated intestinal perforation in newborn infants in 323 neonatal intensive care units to determine whether in utero magnesium exposure was associated with spontaneous intestinal perforation in extremely low birth weight newborns (<1000 g). Their study included 28 035 neonates, of who 11,789 had been exposed to MgSO4 in utero. The mean gestational age of both exposed and not exposed infants was lower compared to our patients (26 vs. 28 weeks). The study did not find an association between antenatal exposure and an increased risk of spontaneous intestinal perforation or NEC, which our own findings are consistent with.
Neonatal cardiorespiratory abnormalities are also among the adverse events potentially associated with antenatal exposure to MgSO4 described in the literature. Although the hypothesis regarding these effects have not yet been proven,23 the seventh edition of the Textbook of Neonatal Resuscitation, el includes MgSO4 in the list of drugs that may cause neonatal respiratory depression when administered to the mother during gestation.24
We did not find significant differences between groups in the 1- or 5-min Apgar score, the need for resuscitation at birth, the maximum FiO2 in the delivery room, the pH and lactate values in the first blood gas analysis or the need for inotropic drugs in the first 72 h post birth. Although more studies have provided data on these outcomes compared to intestinal complications, the results are not homogeneous and in some cases are completely contradictory.
Thus, 50 years ago, Lipsitz and English10 described hypotonia, hyporeflexia and respiratory depression in 16 neonates that they attributed to antenatal administration of MgSO4 to the mother. Later, Lipsitz25 published a larger case series that included 37 neonates, reporting that the Apgar score was lower in the group with antenatal MgSO4 exposure. Riaz et al. found a higher incidence of hypotonia and lower Apgar scores in neonates exposed to MgSO4,21 although their findings are not comparable to ours since their study was conducted in infants delivered after 34 weeks whose mothers had received MgSO4 for maternal health problems as opposed to foetal neuroprotection. The authors did not have an association between those outcomes and neonatal or maternal serum magnesium levels or the dose and duration of treatment with MgSO4. More recent studies26 have found features of CNS depression or cardiorespiratory alterations, such as changes in heart rate or decreased breathing movements, even with maternal serum magnesium levels in the therapeutic range (4−8 mg/dL), although the study was performed in mothers that received MgSO4 as a tocolytic agent and did not document serum magnesium levels in the infants. Most of the studies that reported lower Apgar scores and a higher frequency of hypotonia and intubation compared these outcomes to maternal magnesium levels, usually in term neonates and with exposure to doses used for treatment of preeclampsia and eclampsia, and therefore their conclusions cannot be compared to ours.
On the other hand, as we mentioned before, a fair number of studies have found that these neuromuscular effects on the neonate are not clinically significant,5,13,27–29 which was also the case in our study. Furthermore, many of these studies were conducted in populations similar to our sample of PT neonates delivered before 32 weeks of gestation whose mothers had received MgSO4 for foetal neuroprotection. For instance, in 2008 Rouse et al. published the results of a clinical trial with random allocation to MgSO4 infusion or placebo of 2241 women that gave birth between 24 and 31 weeks’ gestation. The authors did not find an increase in perinatal mortality, neonatal hypotonia or other morbidity in exposed infants. However, exposure to MgSO4 was associated with a significant decrease in the incidence of cerebral palsy, especially in infants born between 24 and 27 weeks.28 De Jesus et al. made a retrospective comparison of cardiorespiratory events in PT neonates (23+0–28+6 weeks of gestation) with and without exposure to MgSO4, without documenting the reason for administration of MgSO4. The study did not find an association between antenatal exposure to MgSO4 and an increased risk of cardiorespiratory events in the immediate postnatal period. The need for invasive mechanical ventilation on day 3 post birth and for treatment for hypotension on day 1 were less frequent in the infants exposed to MgSO4, despite a lower birth weight and gestational age. The authors did not find an increased probability of neonatal resuscitation, neonatal morbidity or mortality, a greater delay in enteral nutrition or a longer length of stay in the exposed group.5 The results of Lloreda et al.13 were similar to those of De Jesus et al. and our own in a study of similar characteristics (gestational age <32 weeks, exposed to MgSO4 given for neuroprotection) a prospective design. These authors did not find statistically significant differences in the advanced neonatal resuscitation, invasive mechanical ventilation, mortality or some of the associated clinical features, like the delay to first passage of meconium. On the other hand, a meta-analysis conducted in adherence with the 2016 PRISMA guideline30 found an increased risk of a 5-min Apgar score of less than 7 and need of supplemental oxygen at 36 weeks and mechanical ventilation in exposed infants, although the differences were not statistically significant. This review also did not find differences in mortality. Our results were consistent with the findings of other systematic reviews, for instance, the one conducted by Magee et al.,29 who concluded that exposure to MgSO4 is not associated with the probability of a 5-min Apgar score under 7, neonatal hypotonia or the need of respiratory support.
The chief limitation of our study is its retrospective design, which has intrinsic drawbacks and risks of bias. We were not able to report or analyse the dose and duration of antenatal MgSO4 treatment nor maternal or neonatal magnesium levels and the association between them, aspects on which the evidence published to date is contradictory, or the reason why certain patients received MgSO4 and others did not, as these data were not expressly documented in health records in most cases. However, the greater proportion of multiple gestation and lower proportion of antenatal steroid therapy in the unexposed group could be explained by their probable association with precipitous labour, an event that leaves no time to initiate treatment with MgSO4.
In addition, we did not establish different groups based on gestational age (despite the known differences in physiological maturation and adaptation to extrauterine life associated with it) due to the reduction in statistical power that this would entail given the small size of the subgroups.
Lastly, we did not analyse the subsequent detection of diseases like aganglionic megacolon or cystic fibrosis, which could be a source of bias in intestinal complication results, although patient outcomes at the time of discharge were favourable enough to not warrant screening for these conditions before sending the infants home.
We may close the discussion by highlighting that the sample under study was homogenous in terms of the main gestational, perinatal and neonatal characteristics, with the sole differences being a higher proportion of multiple gestation and lower proportion of antenatal steroid therapy in the MgSO4, as noted above. Based on the greater frequency of antenatal steroid therapy in this group, we could have expected better respiratory outcomes compared to the group without MgSO4 exposure. However, we did not find short-term differences in the need for advanced resuscitation, the Apgar scores, the initial FiO2 or the length of stay. Lastly, the authors did not find any evidence in the existing literature that could explain the higher frequency of hypothyroidism and female sex in the unexposed group. When it came to maternal hypothyroidism, the frequency was 28.8% in the group treated with MgSO4 compared to 8.9% in the group that did not receive it (p = .000), and the authors did not find an explanation of this phenomenon. Still, the authors did not believe that this interfered with the results, as all mothers received adequate hormone replacement therapy.
ConclusionThe study did not find evidence of an association between antenatal maternal treatment with MgSO4 and the development of meconium obstruction or respiratory depression in newborn infants.
In the future, performance of prospective studies with consideration of the association between neonatal serum magnesium levels and the described potential adverse events would be useful to improve the understanding and management of perinatal outcomes following antenatal administration of MgSO4 for neuroprotection.
FundingThe authors did not receive any form of funding from the public, private or non-profit sectors for the purpose of the study.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Gochi Valdovinos A, Arriaga-Redondo M, Dejuan Bitriá E, Pérez Rodríguez I, Márquez Isidro E, Blanco Bravo D. Terapia prenatal con sulfato de magnesio y obstrucción intestinal por meconio en recién nacidos pretérmino. An Pediatr (Barc). 2022;96:138–144.