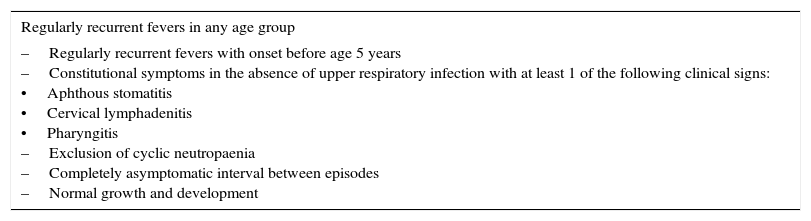
Periodic fever, aphthous stomatitis, pharyngitis, and adenitis syndrome (PFAPA) is the most common type of recurrent fever in the paediatric age group. It was first described in 1987 by Marshall et al.,1 and it is characterised by episodes of fever of three to six days duration that recur periodically every three to eight weeks. Typically, the onset occurs before age 5 years and it subsides without resulting in sequelae between 9 and 11 years of age, with an excellent prognosis. It is diagnosed based on a series of clinical criteria that are presented in Table 1.2
Diagnostic criteria used for PFAPA.
| Regularly recurrent fevers in any age group |
|---|
| –Regularly recurrent fevers with onset before age 5 years –Constitutional symptoms in the absence of upper respiratory infection with at least 1 of the following clinical signs: •Aphthous stomatitis •Cervical lymphadenitis •Pharyngitis –Exclusion of cyclic neutropaenia –Completely asymptomatic interval between episodes –Normal growth and development |
Source: Thomas et al.2
Its aetiopathogenesis is unknown, although it is believed that it is an autoinflammatory disease with an underlying dysregulation in the production of proinflammatory cytokines in response to specific stimuli. The excellent response of PFAPA to corticosteroid therapy seems to support this hypothesis.
There are cases with a family history, but no reports of a directly associated mutation.
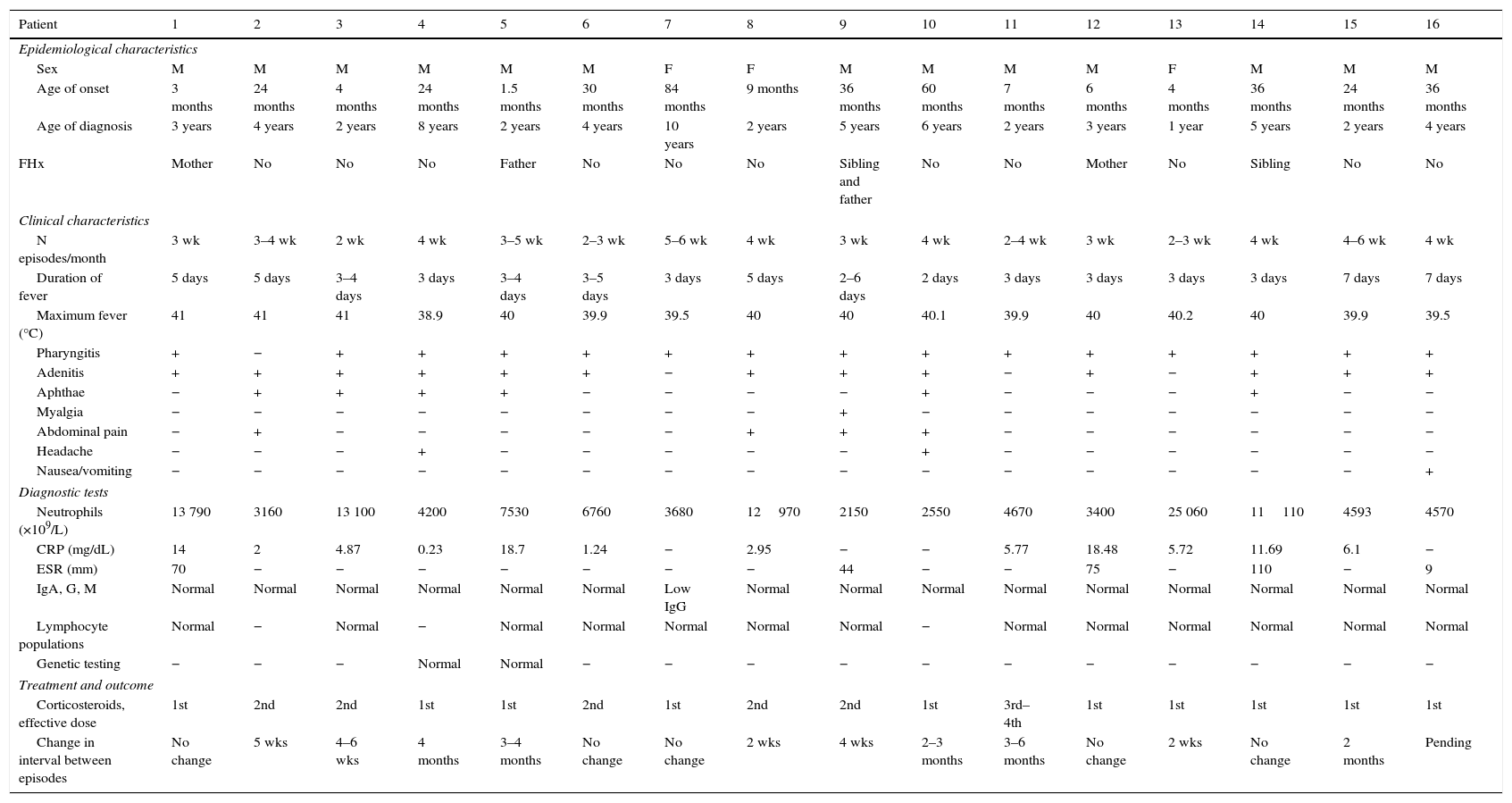
We present our experience by retrospectively reviewing the 16 cases of PFAPA followed up in the unit of paediatric allergy and clinical immunology of our hospital since 2009.
Table 2 summarises the clinical and epidemiological characteristics of the patients.
Clinical and epidemiological characteristics of patients.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Epidemiological characteristics | ||||||||||||||||
| Sex | M | M | M | M | M | M | F | F | M | M | M | M | F | M | M | M |
| Age of onset | 3 months | 24 months | 4 months | 24 months | 1.5 months | 30 months | 84 months | 9 months | 36 months | 60 months | 7 months | 6 months | 4 months | 36 months | 24 months | 36 months |
| Age of diagnosis | 3 years | 4 years | 2 years | 8 years | 2 years | 4 years | 10 years | 2 years | 5 years | 6 years | 2 years | 3 years | 1 year | 5 years | 2 years | 4 years |
| FHx | Mother | No | No | No | Father | No | No | No | Sibling and father | No | No | Mother | No | Sibling | No | No |
| Clinical characteristics | ||||||||||||||||
| N episodes/month | 3 wk | 3–4 wk | 2 wk | 4 wk | 3–5 wk | 2–3 wk | 5–6 wk | 4 wk | 3 wk | 4 wk | 2–4 wk | 3 wk | 2–3 wk | 4 wk | 4–6 wk | 4 wk |
| Duration of fever | 5 days | 5 days | 3–4 days | 3 days | 3–4 days | 3–5 days | 3 days | 5 days | 2–6 days | 2 days | 3 days | 3 days | 3 days | 3 days | 7 days | 7 days |
| Maximum fever (°C) | 41 | 41 | 41 | 38.9 | 40 | 39.9 | 39.5 | 40 | 40 | 40.1 | 39.9 | 40 | 40.2 | 40 | 39.9 | 39.5 |
| Pharyngitis | + | − | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Adenitis | + | + | + | + | + | + | − | + | + | + | − | + | − | + | + | + |
| Aphthae | − | + | + | + | + | − | − | − | − | + | − | − | − | + | − | − |
| Myalgia | − | − | − | − | − | − | − | − | + | − | − | − | − | − | − | − |
| Abdominal pain | − | + | − | − | − | − | − | + | + | + | − | − | − | − | − | − |
| Headache | − | − | − | + | − | − | − | − | − | + | − | − | − | − | − | − |
| Nausea/vomiting | − | − | − | − | − | − | − | − | − | − | − | − | − | − | − | + |
| Diagnostic tests | ||||||||||||||||
| Neutrophils (×109/L) | 13 790 | 3160 | 13 100 | 4200 | 7530 | 6760 | 3680 | 12970 | 2150 | 2550 | 4670 | 3400 | 25 060 | 11110 | 4593 | 4570 |
| CRP (mg/dL) | 14 | 2 | 4.87 | 0.23 | 18.7 | 1.24 | − | 2.95 | − | − | 5.77 | 18.48 | 5.72 | 11.69 | 6.1 | − |
| ESR (mm) | 70 | − | − | − | − | − | − | − | 44 | − | − | 75 | − | 110 | − | 9 |
| IgA, G, M | Normal | Normal | Normal | Normal | Normal | Normal | Low IgG | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal | Normal |
| Lymphocyte populations | Normal | − | Normal | − | Normal | Normal | Normal | Normal | Normal | − | Normal | Normal | Normal | Normal | Normal | Normal |
| Genetic testing | − | − | − | Normal | Normal | − | − | − | − | − | − | − | − | − | − | − |
| Treatment and outcome | ||||||||||||||||
| Corticosteroids, effective dose | 1st | 2nd | 2nd | 1st | 1st | 2nd | 1st | 2nd | 2nd | 1st | 3rd–4th | 1st | 1st | 1st | 1st | 1st |
| Change in interval between episodes | No change | 5 wks | 4–6 wks | 4 months | 3–4 months | No change | No change | 2 wks | 4 wks | 2–3 months | 3–6 months | No change | 2 wks | No change | 2 months | Pending |
CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; F, female; FHx, family history; M, male.
Thirteen patients were male (81.25%) and three female (18.75%). The median age at onset was 24 months (range, 1.5–84 months) and the median age at diagnosis was 3.5 years (range, 1–10 years), with a median delay in diagnosis of one year and six months (range, 5 months–6 years).
Six patients had a family history of recurrent fever of unknown source. Two patients were siblings (patients 9 and 14).
The mean duration of the intervals between fever episodes was 3.5 weeks, and the mean duration of the episodes before initiation of treatment was four days (range, 2–7 days), with a mean temperature during the episodes of 40°C (range, 38.9–40.2°C).
All patients had at least one of the key symptoms: fourteen had pharyngitis (87.5%), thirteen cervical adenitis (81.2%), seven oral aphthae (43.75%) and five all three symptoms (31.25%). Eight patients had other associated symptoms (abdominal pain in five, headache in two, and myalgia in one). All patients were in general good health between episodes.
It is not rare for these patients to receive antibiotic treatment during the febrile episodes before the diagnosis. Fourteen of the sixteen patients in the study received antibiotherapy that were concurrent with some of the episodes in the past.
The literature has described the presence of leukocytosis with predominance of neutrophils and elevated acute phase reactants during the episodes.3 Consistent with these reports, we found elevated levels of C-reactive protein in 11 patients.
The differential diagnosis must include other periodic fever syndromes such as familial Mediterranean fever, mevalonate kinase deficiency and tumour necrosis factor receptor-associated periodic syndrome. Although the absence of articular or cutaneous manifestations and/or serositis and the rapid response to corticosteroids did not suggest any of these syndromes, genetic testing was ordered in patients with a Gaslini Institute score that indicated a high risk of developing hereditary syndromes with periodic fever.4
Cyclic neutropaenia should also be considered, as it may manifest as episodes of fever every 18–24 days associated with pharyngitis and oral aphthae. During the episodes, there is a marked neutropaenia (<200cells/mm3) of three to five days duration that subsequently normalises. Unlike PFAPA, this condition does not respond to treatment with oral corticosteroids.5
Primary immunodeficiencies (PIDs) are another possibility to consider in patients with recurrent fever. None of the patients in our study presented with warning signs indicative of PID,6 and patients that underwent lymphocyte counts and measurement of immunoglobulin levels had normal results.
As for treatment, all our patients were given oral prednisone (1mg/kg) at the onset of episodes. Eleven responded to the first dose, five to the second dose, and one patient required between three and four doses. The intervals between the febrile episodes after initiation of treatment became longer in eight patients (median, 8 weeks; range, 1–12 weeks).
At present, we consider that only three patients are in remission, having been free of episodes compatible with PFAPA for at least six months. The rest of the patients remain symptomatic, and currently have a median age of 5 years (range, 1–13 years).
Periodic fever, aphthous stomatitis, pharyngitis, and adenitis syndrome is a disease diagnosed based on clinical manifestations that must be considered in patients with recurrent fever. It is important to inform families of its benign nature and that in most cases it goes into remission in adolescence or even earlier.
Please cite this article as: Muinelo Segade A, Vila Sexto L. Síndrome de fiebre periódica, estomatitis aftosa, faringitis y adenitis cervical: Estudio y seguimiento de 16 casos. An Pediatr (Barc). 2017;86:159–161.