Asthma is one of the most prevalent chronic diseases with effective treatment in paediatrics. The aim of this study is to describe the paediatric prescribing of anti-asthmatics in Castilla-León, analyzing its geographic variability and temporal evolution.
Materials and methodsAn analysis was made of prescriptions dispensed in pharmacies of R03 therapeutic subgroup (anti-asthmatic agents), and the active ingredients mepyramine and ketotifen, prescribed in children less than 14 years of age in the Castilla-León health service from 2005 to 2010 in Primary Care. Data is presented in prescribed daily doses per thousand inhabitants per day (PDHD) for each active ingredient being calculated raw rates and age-adjusted to the variables health area, type of health zone and year of study.
ResultsA total of 462,354 prescriptions of anti-asthmatic agents were dispensed to a population of 1,580,229persons/year. There was wide variation between areas in the type and intensity of anti-asthmatic agents used, partly explained by differences in the prevalence of asthma. Montelukast predominated as controller drug in most of them (PDHD 3.1–7.7), being similar the consumption intensity in the three types of health zones (PDHD 4.7–4.8). The annual variability was low.
ConclusionsThe study describes the paediatric prescribing pattern of anti-asthmatic agents in Castilla-León between 2005 and 2010. It shows wide geographical variation, as well as inadequacies regarding current recommendations of asthma treatment.
El asma es una de las enfermedades crónicas con tratamiento eficaz más prevalentes en pediatría. El objetivo de este trabajo es describir la prescripción pediátrica de antiasmáticos en Castilla y León, analizando su variabilidad geográfica y su evolución temporal.
Material y métodosSe estudiaron las prescripciones dispensadas en farmacias del subgrupo terapéutico R03 (medicamentos antiasmáticos) y de los principios activos mepiramina y ketotifeno, realizadas a menores de 14 años en atención primaria en el Sistema Nacional de Salud entre 2005 y 2010. Los datos se presentan en dosis diarias prescritas por 1.000 habitantes/día (PDHD) para cada principio activo, calculándose tasas crudas y ajustadas por edad para las variables área sanitaria, tipo de zona de salud y año del estudio.
ResultadosSe realizaron 462.354 prescripciones de antiasmáticos a una población expuesta de 1.580.229 personas-año. Hubo amplia variabilidad entre las áreas en el tipo e intensidad de los antiasmáticos utilizados, en parte explicada por diferencias en su prevalencia de asma. Montelukast predominó como fármaco controlador en la mayoría de ellas (3,1-7,7 PDHD), siendo su intensidad de consumo similar en los 3 tipos de zonas de salud (4,7-4,8 PDHD). La variabilidad anual fue escasa.
ConclusionesEl estudio describe el patrón pediátrico de prescripción de antiasmáticos en Castilla y León entre 2005 y 2010. Muestra gran variabilidad geográfica, así como inadecuaciones respecto a las recomendaciones actuales de tratamiento del asma.
Anti-asthmatics are one of the most commonly prescribed and consumed drug groups among the general population in Spain1,2 and worldwide.3 In paediatrics they are frequently used not only for asthma treatment but also to treat conditions such as bronchiolitis and recurrent wheezing in small children.4–7 All these diseases are very common in the paediatric age group. Asthma is the most prevalent effectively treatable chronic disease in childhood, and it is estimated that 10% of children and adolescents have it.8 Every year, moreover, 10–13% of infants suffer bronchiolitis and between 30 and 45% of children experience wheezing in the first years of life.6,9,10 Pharmacological treatment of asthma11–14 is based on the use of short-acting inhaled β2-agonists during attacks and monotherapy with inhaled corticosteroids (ICS) as the main maintenance medication. However, the use of anti-asthmatics in children with bronchiolitis and recurrent wheezing is controversial, as they constitute a disparate group of patients whose response to treatment is not uniform.15–17
On the other hand, variations in medical practice are very common,18 and also affect drug prescription. In Castilla-León this variability has been documented in paediatric primary care with antibiotics for systemic use19 and anticatarrhals.20 Similarly, evidence has been published showing geographical variability in the treatment of acute bronchiolitis in primary care in Spain.7
In the case of childhood asthma, outpatient prescription of anti-asthmatics also varies in different parts of the world.21 In Spain some studies reveal how they are used at a local level,22–25 but there are few that describe their use at autonomous community level.26–28 They show wide geographical variability.
This study seeks to provide further information on current prescribing of anti-asthmatics to children in Spain. Its objective is to describe the consumption of anti-asthmatics prescribed to patients under the age of 14 in primary care in the public health system of Castilla-León, analysing its geographical and temporal variability during the period 2005–2010.
Population and methodsThis is an observational, descriptive, retrospective study performed in the autonomous community of Castilla-León, which has a population of 2,550,000 (12% of whom are under 14). Its asthma prevalence in the paediatric population in 2010 was 7.4%, according to medical diagnosis data from computerised primary care medical records.
The exposed population consisted of children under 14 with an individual health card in Castilla-León between 2005 and 2010. The population data were provided by the Primary Care Technical Department of the Castilla-León Regional Health Service (Sacyl), which covers 96% of the population.
The prescribing data comes from the Sacyl Pharmacy Information System (Concylia). It consists of details of computerised official prescriptions issued in primary care from 1 January 2005 to 31 December 2010 and dispensed in pharmacies. Those from specialist care are not included, as they are not computerised, nor are prescriptions from the private sector. They correspond to the R03 therapeutic subgroup (drugs for obstructive airway diseases) and to the active ingredients mepyramine (R06AC01) and ketotifen (R06AX17) in the World Health Organization's Anatomical Therapeutic Chemical (ATC) Classification System. The reasons for including mepyramine and ketotifen are the indications in their Summaries of Product Characteristics. Mepyramine has bronchodilator action due to its xanthine component (acefyllinate) and is indicated as a bronchodilator in acute and chronic bronchitis. Ketotifen has an indication for prophylaxis of bronchial asthma. In the prescriptions, we analysed the active ingredient, the year of prescription, the health area in which it was prescribed (Castilla-León is divided into 11 areas) and the type of district in which it arose: urban, semi-urban or rural. These health districts are an official classification based essentially on population criteria for each town. Urban health districts are those containing a population centre with more than 20,000 inhabitants and semi-urban districts are those that have a centre with more than 7,000 inhabitants but fewer than 20,000. In urban and semi-urban districts the child population has a specialist paediatrician as its regular primary care doctor; in rural districts it is usually a general practitioner. The identification details of the patient, the prescribing physician and the commercial brand used were not collected, to preserve anonymity.
The principal unit of analysis was the prescribed daily dose (PDD), which is the mean daily dose of a given drug prescribed in its main indication. PDDs were calculated taking account of the recommended doses by age or weight in the Summaries of Product Characteristics of the drugs being studied and the main childhood asthma guidelines. PDDs were estimated for 26 active ingredients with 59 different pharmaceutical presentations. For some drugs the PDD was calculated per kilogram of body weight per day, using reference weight charts for the current Spanish child population.29 For others, the PDD was estimated by age group. The methodology is described in detail in another article.30 To measure the use density, prescribed daily doses per 1000 inhabitants per day (PDHD) was used; this represents the average number of daily doses prescribed every day to 1000 exposed persons. The raw and age-adjusted PDHDs were calculated for each active ingredient and analysed in relation to the variables: year of prescription (2005–2010), health area in which prescription took place and type of district, urban, semi-urban or rural, in which it was prescribed (an indirect method of measuring the differences in prescribing by paediatricians and general practitioners, since the population denominator was not available in the study design to calculate specific prescription rates for each type of professional). The numbers of PDHD were analysed using raw (RR) and age-adjusted (RRaj) rate ratios. For this purpose, the age-adjusted PDHDs (PDHDaj) for the various health areas were compared with the average PDHD for Castilla-León (geographical variability), the PDHDaj for semi-urban and rural health districts with those for urban health districts (variability by district) and the PDHDaj for each year from 2006 to 2010 with that for 2005 (temporal variability). To produce the territorial information maps, the areas were categorised into tertiles, taking their asthma prevalence into account and dividing them into areas of high prevalence (>8%: Bierzo, León, Burgos), intermediate prevalence (6.5–8%: Palencia, Salamanca, Zamora, Soria) and low prevalence (<6.5%: East and West Valladolid, Segovia, Ávila). Prescribing was classified as low when it was at least 20% below the regional mean (RRaj≤0.8), high if it was at least 20% above the mean (RRaj≥1.2) and intermediate with respect to the mean (RRaj>0.8–< 1.2). Spearman's correlation coefficient (coef) was used to evaluate the association between asthma prevalence and rate of prescription of the main anti-asthmatics in the various health areas, with figures over 0.7–0.8 being considered significant (showing the existence of a correlation). SPSSv15 and Excel spreadsheet programming were used for the analysis.
ResultsDuring the 6 years of the study period 462,354 prescriptions of anti-asthmatics were made to an exposed population of 1,580,229 person-years. Of these prescriptions 82.3% were issued by paediatricians, 14.5% by general practitioners, 2.5% by emergency service doctors and 0.7% by others. Paediatricians issued 42.5% of the prescriptions in rural districts, 92% in semi-urban districts and 98.5% in urban districts.
Table 1 shows the total amount of anti-asthmatics consumed. Among the bronchodilators, the inhalation route was the most frequently used (5.9 PDHD) and inhaled salbutamol was the most commonly consumed (4.4 PDHD). For maintenance therapy the main subgroup prescribed was leukotriene antagonists (montelukast: 5.2 PDHD), followed by single-drug inhaled corticosteroids (ICS) (4.6 PDHD) and long-acting β2-agonists combined with ICS (β2 in combination: 2.2 PDHD).
Total prescriptions of anti-asthmatics by sub-groups in number and percentage of prescriptions and of PDHD, Castilla-León 2005–2010.
| ATC Code | Type of anti-asthmatic | No. of prescriptions | % Of prescriptions | PDHD | % of PDHD |
|---|---|---|---|---|---|
| R03AC, R03BB, R03CC | Bronchodilators | 189,088 | 40.90 | 7.52 | 36.36 |
| R03AK | β2 combined with inhaled corticosteroids | 25,213 | 5.45 | 2.21 | 10.04 |
| R03BA | Single-drug inhaled corticosteroids | 73,456 | 15.89 | 4.86 | 22.08 |
| R03BC | Cromones | 334 | 0.07 | 0.01 | 0.06 |
| R03DA | Xanthines | 57 | 0.01 | 0.00 | 0.00 |
| R03DC | Antileukotrienes | 106,728 | 23.08 | 5.18 | 23.55 |
| TOTAL R03 | 394,876 | 85.40 | 19.79 | 90.90 | |
| R06AC01 R06AX17 | Mepyramine+ketotifen | 58,233+9245 | 12.6+1.99 | 1.76+0.30 | 9.10 |
| Total R03+mepyramine+ketotifen | 462,354 | 100 | 21.84 | 100 | |
PDHD: prescribed daily doses per 1000 inhabitants per day.
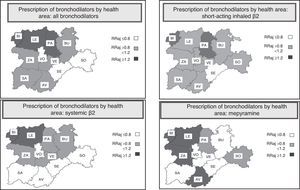
There was great variability between health areas in the prescribing of anti-asthmatics. In Fig. 1 we can see the use density of the principal anti-asthmatics in these areas. In the case of bronchodilators, inhalation predominates in the Palencia, El Bierzo, León and Burgos areas, and the use of mepyramine was strikingly high in León, Zamora and Ávila. For maintenance therapy, montelukast was the most commonly used active ingredient in most areas, except El Bierzo, Palencia and Burgos, where ICS predominated over the other subgroups. A significant correlation was found between asthma prevalence and total prescribing of bronchodilators, short-acting β2-agonists, and ICS and β2 in combination (coef 0.7–0.8). There was no correlation with the use of montelukast and mepyramine.
Use density of the principal anti-asthmatics in the various health areas, Castilla-León 2005–2010. (A) Use density of the principal bronchodilators. (B) Use density of the principal maintenance therapy sub-groups. β2 in combination: β2 in combination with inhaled corticosteroids; ICS: inhaled corticosteroids. AV: Ávila; BIER: El Bierzo; BU: Burgos; LE: León; PAL: Palencia; SAL: Salamanca; SEG: Segovia; SO: Soria; VA-E: East Valladolid; VA-O: West Valladolid; ZA: Zamora.
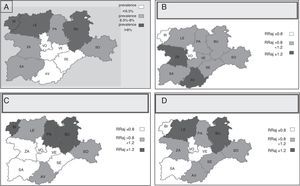
Figs. 2 and 3 show maps with territorial information on the use of the most commonly consumed anti-asthmatics and on the prevalence of asthma in the various areas.
Maps showing information on geographical variability in the use of the principal maintenance therapy anti-asthmatics in the health areas of Castilla-León (2005–2010). (A) Map showing asthma prevalence in the health areas of Castilla-León. (B) Prescription of maintenance therapy by health area: antileukotrienes. (C) Prescription of maintenance therapy by health area: single-drug ICS. (D) Prescription of maintenance therapy by health area: β2 in combination. RRaj: age-adjusted rate ratio for each health area, in relation to the mean for all areas of Castilla-León.
Fig. 4 reports the rate of prescription of the principal anti-asthmatics in the different types of district: urban, semi-urban and rural. Overall, more anti-asthmatics were prescribed in urban and semi-urban districts. Montelukast had a similar consumption rate in all 3 types of district.
Fig. 5 shows the year-by-year changes in prescribing of the principal anti-asthmatics. The annual variations were slight.
DiscussionThis study describes the pattern of paediatric prescribing of anti-asthmatics in the various health areas and basic health zones of Castille-León and how it developed over time from 2005 to 2010. It shows great geographical variability in prescribing in the different areas, both in the quantity and in the type of anti-asthmatics used. This is related in part to the prevalence of asthma, but not for all active ingredients, since montelukast and mepyramine do not correlate with it, probably because they were used to treat bronchiolitis and recurrent wheezing. It also displays variability in the 3 types of health districts, with a predominance of consumption in urban and semi-urban districts mostly served by paediatricians, except for montelukast, which was used similarly in all 3 types of districts. There was little annual variation in the prescribing of anti-asthmatics in the period analysed.
Geographical variability in the paediatric use of anti-asthmatics has also been reported at an international level. A recent systematic review analysed outpatient prescriptions of anti-asthmatics,21 revealing that from 5% to 26% of children received them and identifying 2 types of patterns: those of countries with high prescription levels (Italy, Canada, USA) and those of countries with low levels (Norway, the Netherlands). In addition, the authors observed that the prevalence of anti-asthmatic prescription and of asthma did not coincide in some countries. They also described intra-country variability in prescribing, both in quantity (Italy, 5%–32%; the Netherlands, 3.5%–8%) and in the type of anti-asthmatics used. They argue that these differences could be due to different prevalences of asthma between countries, different national drug regulation policies, the diversity of the studies analysed and different attitudes on the part of prescribing doctors.
In Spain, similarly, differences and inappropriate treatment practices have been observed in paediatric prescribing of anti-asthmatics in primary care in some autonomous communities. In Cantabria26 (2006) there was a predominance of ICS, with montelukast and β2 in combination a long way behind. Asturias (2008)28 had high consumption of montelukast compared with ICS (ratio 1:1) and an inappropriate prescription ratio for ICS/β2 in combination (ratio 1:1), and prescription of montelukast was very variable in number of packages between the different health areas (from 15 to 39%: data supplied by the authors). For Andalusia27 (2009), a study was published showing high geographical variability which was not justified either by differences in etiopathogenesis or by the severity of the asthma found. Further Spanish data on asthmatic children at a local level clearly reveal variability.22,23,25
Another question that should be highlighted is the pattern of use of some anti-asthmatics found in Castilla-León.30 For example, the prescribing of systemic β2-agonists is worth mentioning (20% of all bronchodilators). There was a strikingly high use of mepyramine, an antihistamine with bronchodilatory properties consumed basically by children under 2 years old and not recommended in any clinical guideline or protocol on asthma or on management of wheezing in small children, nor as an anticatarrhal. Use of this drug remained constantly high throughout the study period. This result cannot be compared with other autonomous communities, because there is no information, although a study from Valencia31 describes frequent use in the children studied. Moreover, there was predominant consumption of montelukast as the main asthma control drug. We do not know the reason for this kind of prescribing in Castilla-León. Although age is a determining factor in prescribing these drugs,30 it is not a cause of the differences observed in the geographical distribution of prescriptions, as there are no appreciable differences in the age distribution of the child population in the various health areas. The different prevalence of asthma between areas and the use of this drug to treat conditions with symptoms similar to those of asthma partly explain the variability.
The possible causes of high prescription of montelukast could include induced prescription from specialist care (prescription initiated in specialist care but renewed by the primary care doctor) and pressure from the pharmaceutical industry.30 Entrenched habits of prescribing certain active ingredients could be a reason for the use of systemic β2-agonists, mepyramine and ketotifen, and other factors, such as unequal access to training activities, large caseloads, pressure from parents, and doctors’ communication skills, could also be involved.
As regards variability in prescribing between urban and rural districts, in our study we observed a lower overall use of bronchodilators, ICS and β2 in combination in rural than in urban and semi-urban districts, with a uniformly high consumption of antileukotrienes in all 3. These data could mean that paediatricians use anti-asthmatic therapy more than general practitioners. But it is also possible that there is a higher prevalence of asthma in urban and semi-urban districts32 (mostly served by paediatricians) that has given rise to higher levels of prescribing in those districts, although that would not explain the qualitative differences in the type of prescription. It is unlikely that the variability between districts is due to differences in socioeconomic or health-care factors (higher number of rural districts in some areas than in others, different ratio of inhabitants per paediatrician, age of the prescribing doctors, etc.). However, there are insufficient data available to enable us to analyse this.
Some research studies have revealed discrepancies in habits of treatment and prescribing between paediatricians and general practitioners.20,33 In asthma, specifically, they report a greater capacity to resolve cases on the part of paediatricians. There are no studies on prescribing to the paediatric population by different medical professionals in Spain. In Castilla-León, a local study reveals those differences in two health districts,24 finding greater use of systemic bronchodilators and oral corticosteroids in the rural district, served by general practitioners, and greater use of maintenance therapy in semi-urban districts, served by paediatricians.
As for annual variability, the changes were not very significant. It is striking that a pattern of consumption apparently out of line with recommendations should have been maintained, despite the fact that the guidelines and consensus documents published in this period on asthma11–14 and on bronchiolitis and wheezing in viral infectious diseases15–17 did not advise it and that numerous training activities organised by institutions and learned societies were held to foster a more rational use of these drugs. Temporal variability has also been observed in other studies in Spain. In Andalusia,27 for example, a reduction in the use of ICS was detected, with an increase in combined β2 and in montelukast. In Palencia, 2 studies carried out in a health district in 199934 and 200725 showed a reduction in the percentage of asthmatic schoolchildren with maintenance therapy (from 80 to 24%) and replacement of cromones, long-acting β2-agonists and ketotifen by ICS, antileukotrienes and β2 in combination. Internationally, studies show greater use of ICS,35–37 a reduction in long-acting β2-agonists and an increase in their use in combination with ICS. As for antileukotrienes, their consumption is variable and has increased in countries like the United Kingdom,35 Australia37 and the USA.36
Finally, we should comment on some limitations of this study. One of these is that it analyses data from computerised prescriptions to children under the age of 14 in the public health system outside hospitals, dispensed in pharmacies. It therefore does not include hospital prescriptions (6% of total prescriptions in this period), nor manual prescriptions in primary care (20% of those issued), nor those through private insurance (10%–15% of medical consultations in less than 15 years in Spain),38 nor anti-asthmatics purchased without a prescription (2.5%).38 On these figures, the data studied probably represent 65% of the anti-asthmatics consumed in Castilla-León in this period.
Another limitation is that there is no connection between the pharmaceutical information system and the electronic medical records, which means that we do not know the clinical conditions for which the drugs were prescribed.
A final limitation is the unit of measurement used. Since we had no data from medical records, we estimated the doses for each active ingredient according to the child's age and weight or the concentration of each drug. Thus the prescribed daily doses (PDDs) calculated are theoretical doses, although they are probably very close to those actually recommended, given that the sources of information used to estimate them are those most often used by Spanish paediatricians.39
In conclusion, this study has made it possible to discover the geographical and temporal pattern of consumption of anti-asthmatics in the paediatric population of Castilla-León. It shows considerable geographical variability in prescribing and high use of certain active ingredients, especially montelukast. Knowing the pattern of consumption enables us to detect areas for improvement and may be useful for reducing variability in prescription. As medical professionals we should reflect, together with health care administrators, on our styles of medical practice and on how to evaluate and improve that practice. Management guidelines for asthma and related conditions are probably known but are not put into practice,40 and we therefore need to identify the existing barriers in order to implement appropriate and effective training interventions.
Conflicts of interestThe authors have no conflicts of interest to declare.
We would like to thank Judit Ceruelo, Julia Rodríguez and Alejandra Ortiz, pharmacists in the Sacyl Pharmacy Technical Department, and Marcelino Galindo, Head of Service of the Primary Care Technical Department of Sacyl, for their valuable help.
Please cite this article as: Casares Alonso I, Cano Garcinuño A, Blanco Quirós A, Pérez García I. Prescripción pediátrica de fármacos antiasmáticos en atención primaria en Castilla y León. Variabilidad geográfica. An Pediatr (Barc). 2015;83:191–200.
This article was previously presented as an “oral communication” at the Spring Meeting of the SCCALP, Palencia 12–13 April 2013, where it was awarded a prize as one of the two best oral communications.