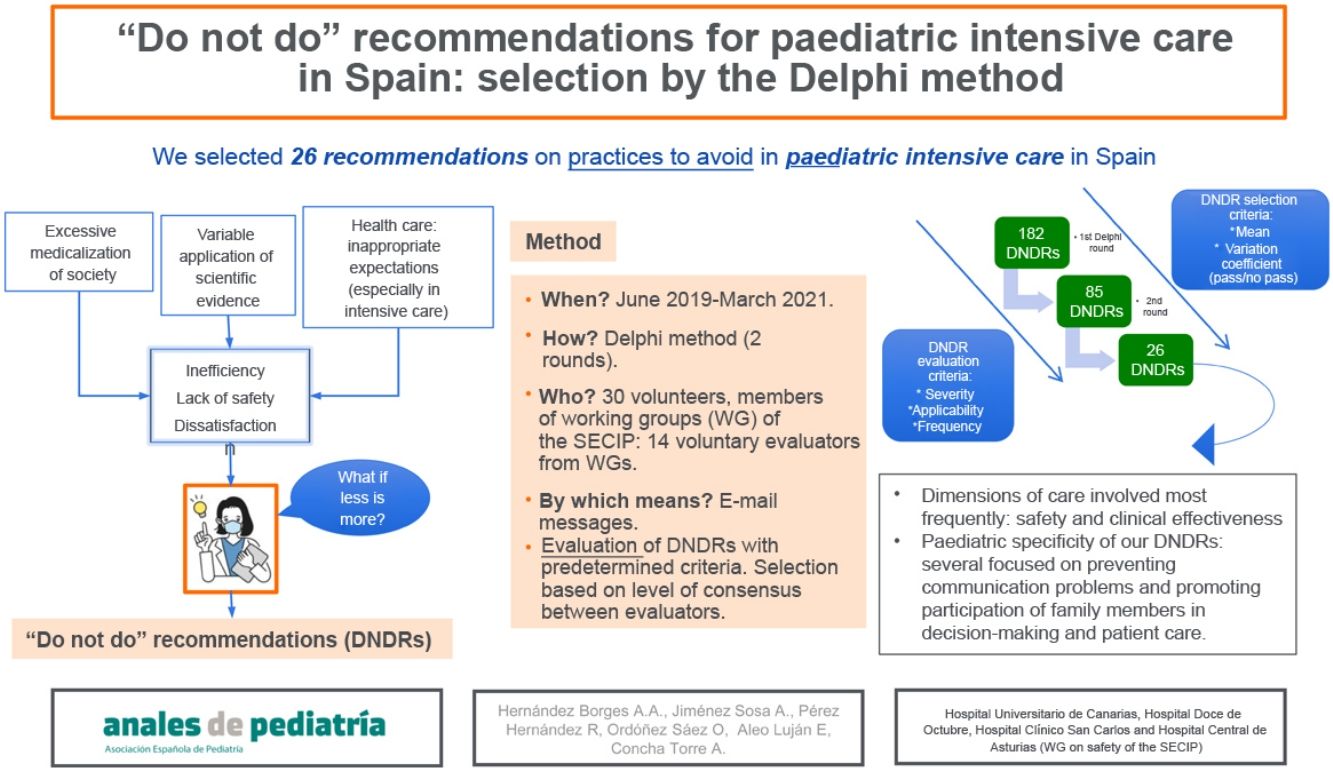
Health care is not free of ineffective, unsafe or inefficient diagnostic and therapeutic practices. To address this, different scientific societies and health authorities have proposed ‘do not do’ recommendations (DNDRs). Our goal was the selection by consensus of a set of DNDRs for paediatric intensive care in Spain.
Material and methodThe research was carried out in 2 phases: first, gathering potential DNDRs; second, selecting the most important ones, using the Delphi method, based on the prevalence of the practice to be modified, the severity of its potential risks and the ease with which it could be modified. Proposals and evaluations were both made by members of working groups of the Sociedad Española de Cuidados Intensivos Pediátricos (SECIP, Spanish Society of Paediatric Intensive Care), coordinated by email. The initial set of DNDRs was reduced based on the coefficient of variation (<80%) of the corresponding evaluations.
ResultsA total of 182 DNDRs were proposed by 30 intensivists. The 14 Delphi evaluators managed to pare down the initial set to 85 DNDRs and, after a second round, to the final set of 26 DNDRs. The care quality dimensions most represented in the final set are clinical effectiveness and patient safety.
ConclusionsThis study allowed the selection by consensus of a series of recommendations to avoid unsafe, inefficient or ineffective practices in paediatric intensive care in Spain, which could be useful for improving the quality of clinical care in our field.
La asistencia sanitaria no está exenta de prácticas diagnósticas y terapéuticas poco efectivas, inseguras o ineficientes. Como reacción han sido propuestas recomendaciones de 'no hacer' por diferentes sociedades científicas y autoridades sanitarias. Nuestro objetivo fue seleccionar y consensuar un grupo de recomendaciones de 'no hacer' (RNH) en cuidados intensivos pediátricos en España.
Material y métodoEsta investigación se desarrolló en dos fases: primera, recopilación de posibles RNH; segunda, selección por método Delphi de las más importantes según prevalencia de la práctica a modificar, gravedad de sus potenciales riesgos, y facilidad con la que podría ser modificada. Tanto las propuestas como las evaluaciones fueron realizadas por miembros de grupos de trabajo de la Sociedad Española de Cuidados Intensivos Pediátricos (SECIP) coordinados por correo electrónico. El listado inicial de RNH fue reduciéndose en base al coeficiente de variación (<80%) de sus evaluaciones.
ResultadosFueron propuestas 182 RNH por 30 intensivistas. Los 14 evaluadores del Delphi lograron reducir el set inicial a 85 RNH y tras una segunda ronda se llegó a la selección final de 26 RNH. Las dimensiones de calidad más representadas en nuestro set final son la efectividad clínica y la seguridad de pacientes.
ConclusionesNuestro trabajo ha permitido seleccionar y consensuar una serie de recomendaciones para evitar prácticas inseguras, ineficientes o inefectivas en intensivos pediátricos en España, lo que podría ser útil para mejorar la calidad de nuestra actividad clínica.
At present, there is a certain overmedicalization of society that at times results in diagnostic and therapeutic interventions that are poorly supported by evidence that may entail risks and discomfort for patients excessive health care costs and unrealistic health care expectations. Thus, a significant proportion of health care interventions yield little benefit to the patient and may even cause harm. Berwick1 declared that clinical practices of little value may account for 25%–33% of health care expenditures in every country in the world. Similarly, Graham et al.2 established that between 20% and 25% of performed diagnostic and therapeutic procedures are not based on evidence, and therefore may have a deleterious impact on the health of the patient.
Thus, it is no surprise that strategies have been developed to curtail unsafe, ineffective or inefficient practices, such as the “do not do” recommendations of the National Institute for Health and Care Excellence in the United Kingdome or the “Choosing Wisely” initiative in the United States, aiming to promote a more effective and responsible use of health care resources3,4.
In this context, in 2013, the Ministry of Health of Spain, the GuíaSalud national guideline system within the national health system and the Sociedad Española de Medicina Interna (SEMI, Spanish Society of Internal Medicine)5 launched the Commitment for Quality in Spanish Scientific Associations project with the participation of several scientific societies in Spain with the aim of reducing unnecessary health care interventions. In the framework of this project, each scientific society proposed 5 “do not do” recommendations for their corresponding fields. The initial round of the project involved 12 scientific and medical societies, but many more have joined since, including the Asociación Española de Pediatría (Spanish Association of Pediatrics)6.
In the field of intensive care, the Sociedad Española de Medicina Intensiva Crítica y Unidades Coronarias (SEMICYUC, Spanish Society of Critical Intensive Medicine and Coronary Units) published a set of 65 “do not do” recommendations applicable to patients admitted to intensive care units7.
While this issue has been addressed separately in the intensive care and paediatrics fields, there are currently no “do not do” recommendations for patients requiring admission to a paediatric intensive care unit (PICU) in Spain.
The aim of the study was the identification and selection by a group of experts of a set of “do not do” recommendations (DNDRs) for paediatric intensive care in Spain in a consensus-based process.
Material and methodsThe study was organised in 2 phases: the first devoted to gathering potential recommendations, and the second to developing the DNDRs. The project was coordinated by the working group on safety of the Sociedad Española de Cuidados Intensivos Pediátricos (SECIP, Spanish Society of Paediatric Intensive Care) and was conducted entirely by electronic mail between the participants.
The 2 phases of the study developed from June 2019 as follows:
- 1 -
Collection of potential recommendations (9 meses). The coordinators of the 12 working groups of the SECIP disseminated information about the project and received and handled the DNDRs submitted by members regarding any area of paediatric intensive care (PIC). The coordinators asked for proposals to be based on the highest possible level of evidence and to be accompanied by an explanation of the rationale supporting the proposed DNDR. The goal, as detailed in the Commitment for Quality in Spanish Scientific Associations project,5 was to identify “unnecessary interventions, either because there is no evidence of their efficacy, their effectiveness is low or questionable, they are not cost-effective or they are not a priority” in the field of PIC.
Participants entered their proposals in an Excel spreadsheet designed for the purpose. The initial collection of DNDRs also included the recommendations that the SEMICYUC had established in each of its knowledge areas, since the recommendations issued by this association for intensive care in adults could guide and enrich the work at hand.
- 2 -
Evaluation, selection and draft of the recommendations (12 months). After potential recommendations had been collected, a group of members of the working groups of the SECIP who volunteered to collaborate evaluated them to make the final selection. The recommendations were selected by the classic Delphi method.
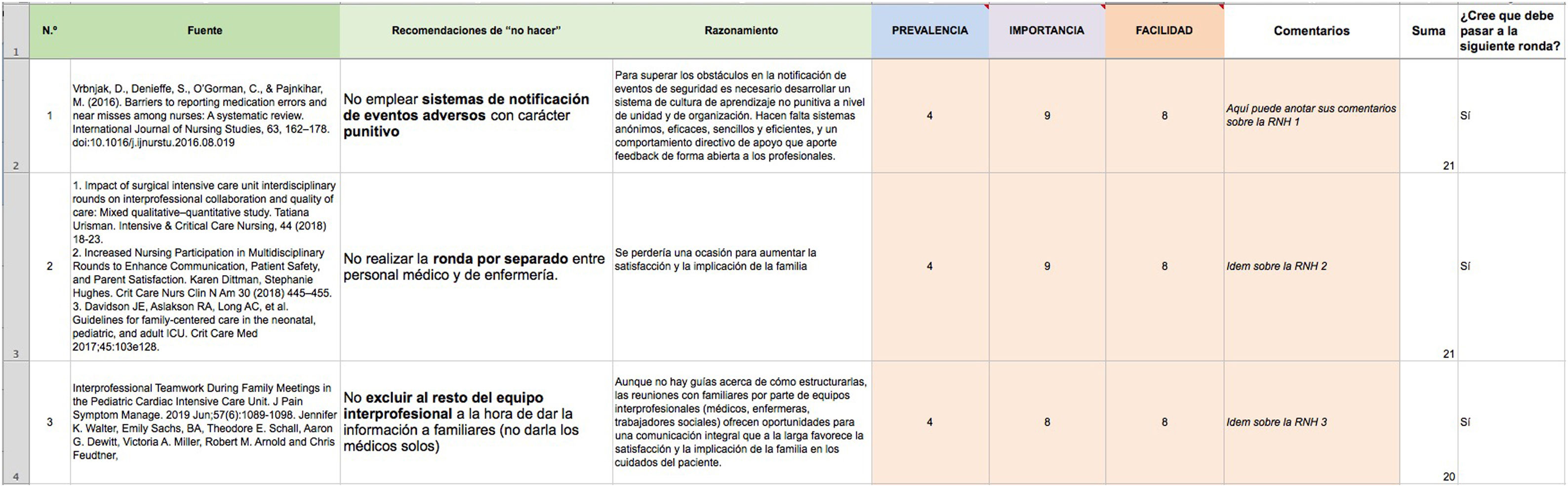
In the second phase, the basic working tool continued to be the Excel spreadsheet, in which the necessary information to describe each DNDR was added to facilitate the assessment of each proposed recommendation: wording of each DNDR, rationale accounting for the care practice that it aims to change and bibliographic references on which the recommendation is based.
The evaluators applied 3 evaluation criteria: the prevalence of the practice the recommendation sought to modify, the severity of the potential effects of the practice, and the ease with which the practice could be modified. Each evaluator rated each of these criteria on a scale of 1–9 for each DNDR based on their knowledge and experience. For example, if a DNDR referred to a very infrequent practice, 1 or 2 points could be given; if the consequences of the practice were very severe, the recommendation could receive 8 or 9 points, and if it appeared that the practice would be very difficult to change or eradicate, 1 or 2 points could be assigned. The greater the sum total of these ratings, the greater the priority assigned to the DNDR.
Evaluators were encouraged to write comments supporting their assessment of each DNDR. All the comments were provided to the evaluators in the second round so that they could finetune their assessments in successive rounds.
If evaluators wished to provide supplementary bibliographic references, they could add them to the spreadsheet in a column devoted to that purpose.
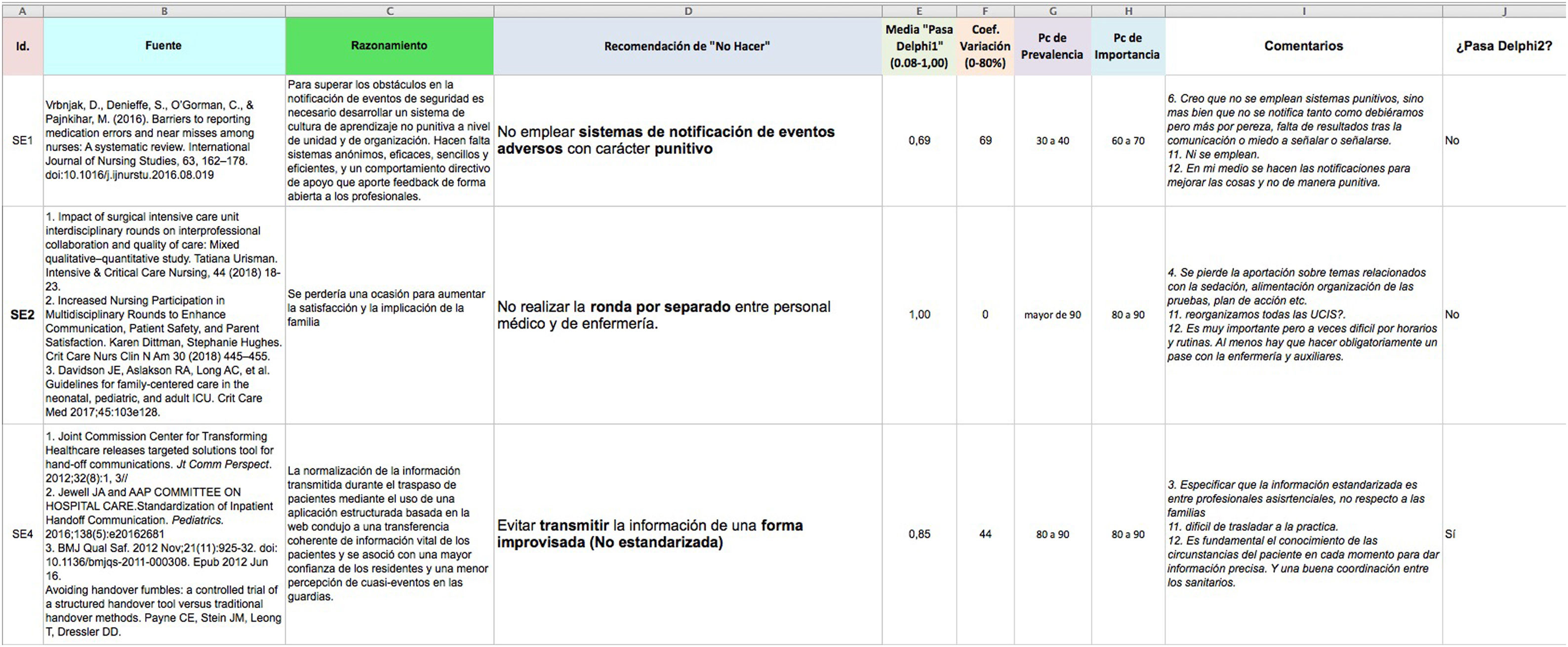
Thus, in the second round of the Delphi process, each evaluator was able to review the ratings of each criterion (expressed as means and percentiles) and the comments of other evaluators in order to make any necessary adjustments to his or her own ratings.
Last of all, for each DNDR, evaluators have to state whether they considered that the recommendation should pass to the next round or be eliminated (“pass” or “not pass” variable, rated as 1 or 0, respectively) (Fig. 1).
Whether DNDRs passed from one round to the next in the Delphi process was decided based on the mean value of the pass/no pass variable and the corresponding coefficient of variation (CV), which was considered acceptable if it was less than 80%. Those that passed were added to the Excel spreadsheet for the DNDRs to be considered in the second round of the Delphi process, which also included the anonymised comments of the raters (Fig. 2).
ResultsThe first phase of the study yielded a total of 182 DNDRs submitted by 30 members of SECIP working groups. Only one working group (Cardiology) did not actively participate by submitting proposed recommendations. The distribution of proposed recommendations by area of knowledge was heterogeneous (Table 1).
Number of DON’T recommendations proposed by area of knowledge in each phase of the study.
| Area of knowledge | Before 1st Delphi round | Before 2nd Delphi round | Final set of DNDRs of the SECIP (excluding the SEMICYUC recommendations) |
|---|---|---|---|
| Cardiology | 6 | 2 | – |
| Ultrasound | 10 | 6 | 2 |
| Infectious disease | 27 | 14 | 2 |
| Ethics | 15 | 7 | 3 |
| Nutrition/Gastrointestinal | 22 | 8 | 3 |
| Polytrauma | 13 | 6 | 3 |
| Resuscitation | 9 | 3 | 2 |
| Respiratory | 32 | 12 | 1 |
| Kidney and internal environment | 11 | 5 | 2 |
| Sedation/analgesia | 13 | 6 | 2 |
| Transport | 14 | 9 | 3 |
| Safety | 10 | 7 | 3 |
The evaluation with the Delphi method was conducted on a voluntary basis by 14 members of the SECIP in different regions of Spain, most of who had already participated in the first phase. The work experience of these evaluators varied widely (ranging from 2 to 24 years in PIC), and all were staff physicians except for 2 section chiefs. Their evaluations reduced the initial set of recommendations to 85 DNDRs (Table 1), and after the second round, the definitive selection included a total of 32 DNDRs, 6 of which were SEMICYUC recommendations (Table 2).
List of the 6 DON’T recommendations obtained from the SEMICYUC that made it through the 2 Delphi rounds.
| Area of knowledge | Wording |
|---|---|
| Cardiology | Do not delay initiation of mechanical circulatory support in patients with cardiogenic shock refractory to vasoactive drugsDo not prescribe adrenergic drugs to normalise isolated haemodynamic parameters without taking into account the clinical situation and signs of low cardiac output or postoperative vasoplegia |
| Infectious disease | Do not maintain invasive devices when they are not necessary |
| Ethics | Do not discontinue life support measures in a patient after brain death without checking whether organ donation is possible |
| Sedation/analgesia | Do not administer sedation without establishing individualised therapeutic goals fitting the clinical situation by means of validated scalesDo not prescribe prolonged neuromuscular blockade until deep sedation and adequate analgesia have been achieved and verified |
Table 3 presents the final set of DNDRs of the SECIP selected after the second Delphi round, excluding the 6 recommendations of the SEMICYUC. For each of them, the table includes the mean pass/no pass value, CV and the rational and bibliographic references that support it.
Final list of 26 DON’T recommendations of the SECIP, ordered by level of consensus (the greater the mean and the lower the coefficient of variation, the greater the agreement). We present the mean value of the “pass/no pass” variable (range, 0-1), the coefficient of variation (CV, %) and elements defining the DON’T recommendations (rationale and references).
| Recommendation | Order | Mean | CV | Rationale | Reference |
|---|---|---|---|---|---|
| Do not use hypotonic maintenance intravenous fluids in paediatric critical patients | 1 | 0.93 | 28.8 | There is evidence of a higher incidence of hyponatraemia in critically ill paediatric patients in association with the use of 0.2% and 0.45% saline solution. This is probably due to antidiuretic hormone elevation in these patients. | 8 |
| Do not delay initiation of enteral nutrition if there are no contraindications | 2 | 0.93 | 28.8 | Based on data from observational studies, enteral nutrition is recommended as the preferred mode of nutrition delivery in critically ill paediatric patients, as it is considered feasible and safe. However, at present, the most common barriers to the use of enteral nutrition of patients in the PICU include delayed initiation, interruptions due to perceived intolerance, and prolonged fasting around procedures. Strong recommendation to minimise delays or interruptions to enteral nutrition in an effort to achieve nutrient delivery goals by the enteral route. | 9 |
| Do not prolong antibiotherapy beyond the recommended duration | 3 | 0.92 | 28.8 | Some studies (such as the PISA study) have found an inadequate duration of antibiotherapy in most analysed cases | 10,11 |
| Do not discharge patients who have undergone procedural sedation from clinical supervision until they have returned to baseline status | 4 | 0.86 | 42.4 | Certain drugs can delay the complete return of the patient to baseline status and therefore call for longer periods of observation. This is particularly important in infants and toddlers transported in strollers or car seats, as resedation leading to airway obstruction has been described in this age group. | 12 |
| Do not delay establishment of intraosseous access in patients in cardiac arrest or at risk of imminent arrest due to insert a central venous catheter with ultrasound guidance | 5 | 0.85 | 44.4 | Intraosseous vascular access is very useful in emergencies in which intravenous access may be difficult to establish, and it is quicker to establish than central vascular access, so time should not be wasted in ultrasound-guided central line placement. | 13 |
| Do not transport paediatric patients until they have been optimally stabilized optimally at the sending hospital | 6 | 0.79 | 54.2 | Transport should not be initiated until the child is in the best possible clinical condition. There is evidence that initiating transport before previous stabilization has a significant impact on morbidity and mortality. | 14 |
| Do not routinely bar the presence of the parents during invasive procedures in children | 7 | 0.79 | 54.2 | Keeping parents away eliminates an opportunity to increase family involvement and satisfaction. | 15 |
| Do not perform medical and nursing rounds separately | 8 | 0.79 | 54.2 | Errors in communication are frequently identified in the root cause analysis of sentinel events. Active participation of nursing staff in multidisciplinary rounds improves communication. It can also contribute to increasing family involvement and satisfaction. | 16,17 |
| Do not delay initiation of continuous renal replacement therapy until the patient has oliguria with fluid overload and urea and creatinine elevation | 9 | 0.79 | 54.2 | In the cited source, fluid overload, the indication for initiation of continuous renal replacement therapy, the severity of disease at the time of ICU admission and an active oncologic diagnosis were independent predictors of mortality. In the survival analysis, the mortality was higher in late initiators (>5 days) compared to early initiators (≤5 days) with a hazard ratio of 1.56 (95% CI, 1.02−2.37). Early initiation of continuous renal replacement therapy was associated with a decreased mortality in this cohort of critically ill children. | 18 |
| Do not delay administration of tranexamic acid more than 3h in trauma patients with significant bleeding | 10 | 0.79 | 54.2 | Administration in the first 3h has been found to be associated with a decreased mortality. Tranexamic acid significantly increased overall survival in bleeding patients. Delayed treatment decreased the benefits of treatment. Immediate treatment improved survival by more than 70%. From then, the increase in survival declined by 10% with each additional 15-minute delay until 3h, after which there were no benefits of treatment. | 19 |
| Do not administer supplemental oxygen in procedures requiring sedation in children in the absence of desaturation or underlying respiratory disease | 11 | 0.77 | 57.0 | Prophylactic use of O2 has been associated with hypoventilation due to undetected prolonged respiratory depression (in these instances, desaturation would be delayed due to increased oxygen reserves). If administration of oxygen is required, capnography should be used (possibly with nasal prongs), as CO2 levels change minutes before O2 saturation and increases in CO2 help detect apnoea. | 12 |
| Do not delay nutrition assessment in paediatric critical patients past 48h post admission | 12 | 0.71 | 65.6 | Observational studies have found that malnutrition is associated with adverse clinical outcomes, including longer duration of ventilation, increased risk of nosocomial infection, increased length of stay in both PICU and hospital and increased mortality. Therefore, we recommend for paediatric critical patients admitted to the PICU to undergo a thorough nutrition assessment within 48h of admission. In addition, given the risk of these patients to experience nutrition deterioration during hospitalization, which can adversely affect clinical outcomes, we suggest re-evaluating their nutrition status at least weekly during the hospital stay. | 9 |
| Do not routinely perform pelvic radiography in children with multiple trauma with a Glasgow coma score greater than 13 without pain or apparent injury to the pelvis, abdomen or lower extremities | 13 | 0.71 | 65.6 | Recent studies in paediatric patients with multiple trauma suggest that pelvic fracture can be ruled out reliably if there is no injury to the lower extremities and the pelvic examination is normal, especially in young children. If performance of an abdominal CT scan is required, an abdominopelvic CT scan can be performed instead. Thus, pelvic radiography can be eliminated from the imaging evaluation of children with multiple trauma aged less than 8 years with no clinical evidence of pelvic injury and in any child requiring an abdominal CT scan. | 20 |
| Do not perform landmark-guided cannulation for central vascular access if ultrasound-guided cannulation is possible | 14 | 0.69 | 69.4 | In both adult and paediatric patients, ultrasound devices and qualified staff should be available whenever central vascular access needs to be established. Ultrasound guidance reduces the risk of internal complications intrinsic in vascular access, shortens the time to successful catheter insertion and reduces overall costs. A recent consensus document established that when ultrasound is available, it should be used routinely for internal jugular central venous catheter insertion (unless there is an emergency or another unusual situation) and any other vascular access procedures (peripheral venous/arterial) in challenging patients. Ultrasound guidance makes many steps safer, including the evaluation of potential insertion sites and the identification of vascular abnormalities; it also avoids the use of wire guides, allows verification of wire guide or catheter placement, provides information on the position of the catheter tip and allows the detection of certain complications. | 21,22 |
| Do not prolong perioperative antibiotic prophylaxis longer than recommended for the type of surgery and patient | 15 | 0.69 | 69.4 | Surgical prophylaxis protocols diverge substantially from current recommendations: for instance, one study found that the duration of antibiotic prophylaxis was greater than recommended in as many as 58.9% of analysed cardiac surgery patients. | 23,24 |
| Do not measure the gastric residual volume to use as an indicator of feeding tolerance or the risk of aspiration | 16 | 0.69 | 69.4 | Although there is not a clear definition of feeding intolerance in paediatric critical patients, this is the most commonly cited reason in the collective of PICU clinicians to discontinue, delay or not initiate enteral nutrition. Despite the lack of support for it, the gastric residual volume is the parameter most frequently used to define feeding intolerance.Feeding intolerance assessments, particularly those based on the gastric residual volume, do not predict delayed gastric emptying or the rate of enteral nutrition advancement. | 9,25 |
| Do not improvise the handoff of patient information during care transitions (vs standardised handoff practices) | 17 | 0.64 | 77.3 | It is estimated that communication errors are involved in 80% of serious medical errors. There is previous evidence that the standardization of information transmitted during patient handoffs through the use of a structured, web-based application leads to consistent transfer of vital patient information and is associated with improved resident confidence and fewer perceived near-miss events on call. | 26,27 |
| Do not transport an intubated paediatric patient without first verifying the correct position of the endotracheal tube | 18 | 0.64 | 77.3 | The position should be verified with at least 2 methods (radiography, capnography, auscultation …). Periodically verify that the ETT tube has not become displaced during transport. Adverse events associated with endotracheal tubes, while infrequent in absolute terms, are among the most severe potential adverse events and are usually reported among the analysed adverse events in published case series. | 28 |
| Do not transport a paediatric patient with respiratory disease only with supplemental oxygen if the patient can benefit from non-invasive ventilation. | 19 | 0.64 | 77.3 | Take into account the limitations of NIV, especially in young children, and always verify its effectiveness before initiating transport. | 14 |
| Do not maintain non-invasive ventilation in patients with acute respiratory distress syndrome with a P/F ratio <150 or an S/F ratio <200 | 20 | 0.64 | 77.3 | Although there is evidence that the use of CPAP in patients ARDS can improve outcomes and reduce intubation rates, the need of intubation continues to be high and, although there are no specific predictors, worsening respiratory rate, O2 requirements, a decrease of the PaO2/FiO2 ratio, an increase in PaCO2 or altered mental status can signal worsening of disease. | 29 |
| Do not use high-flow nasal cannula in patients with moderate to severe acute respiratory failure | 21 | 0.64 | 77.3 | The first cited study30 concluded that in young infants with moderate to severe bronchiolitis, initial treatment with HFNC with a flow rate of 2L/kg corresponded to a lower success rate than use of nasal CPAP at 7cm H2O. The second source31 found a higher mortality in children under 5 years with pneumonia with the use of HFNC compared to CPAP | 30,31 |
| Do not routinely preclude the presence of family members of paediatric critical patients during resuscitation (a staff member should be allocated to support the family) | 22 | 0.64 | 77.3 | In surveys performed in Western societies, most parents want to be present during the resuscitation of their child. Parental presence has neither been perceived as disruptive nor stressful for the staff. Parents witnessing their child's resuscitation believe their presence to be beneficial to the child. Allowing parents to be at the side of their child helps them to gain a realistic view of the attempted resuscitation and the child's death. Furthermore, they may have the opportunity to say goodbye to their child.Parental presence in the resuscitation room may help healthcare providers maintain their professional behaviour, whilst helping them to see the child as a human being and a family member. | 32 |
| Do not routinely obtain CT scans more than 24h after admission unless there is evidence of neurological deterioration or increasing intracranial pressure | 23 | 0.64 | 77.3 | Repeat head CT scans are not clinically useful except in the absence of neurologic improvement, if there is evidence of neurologic deterioration or if there is no other way to assess neurologic status of the patient (use of sedatives or paralytic agents) | 33 |
| Do not perform laboratory tests routinely without previously assessing their need | 24 | 0.64 | 77.3 | Up to half of laboratory tests performed routinely in adult ICUs have normal results, which calls into question the relevance of this practice in decision-making, and evinces the need to consider the potential complications of testing (discomfort to patients, increase in transfusions, risk of infection due to catheter handling) and its economic cost.Similar results have been found in postoperative patients in the PICU setting, with a reduction of 87% in the number of complete blood counts requested in the 6 months that followed quality improvement cycles based on education, auditing and feedback.Similar results have also been obtained in paediatric postoperative cardiac patients in the PICU setting. | 15 |
| Do not restrict the presence or participation in care of parents and caregivers in PICUs | 25 | 0.64 | 77.3 | There are many arguments in support of facilitating the presence of family members in ICUs. Continuous communication makes it easier to keep families informed, and family members can contribute to the patient’s recovery and become part of the intensive care team. Furthermore, children have the right to be accompanied by their parents as much time as possible. The presence of parents and other relatives decreases stress, fear and anxiety in children, reduces the need of sedation and analgesia, improves patient-ventilator synchrony, decreases cardiac stress and shortens the length of stay in the PICU. Parental participation in patient care reduces parental anxiety and worry, which in turn has a positive impact on the recovery of the child. Similarly, it can decrease the duration of nursing care procedures. Family members have the right and the responsibility to be involved in end-of-life care. Lastly, this is beneficial for ICU staff, as it improves the perception of the provided care and interpersonal interactions. | 34,35 |
| Do not maintain broad-spectrum antibiotherapy if de-escalation is possible | 26 | 0.64 | 77.3 | De-escalation is supported by the fact that maintenance of unnecessary antibiotherapy is associated with the development of health care-associated infections and antimicrobial resistance. In addition, de-escalation helps decrease adverse events, health care costs and hospital lengths of stay. | 36,37 |
ARDS, acute respiratory distress syndrome; CPAP, continuous positive airway pressure; CT, computed tomography; ETT, endotracheal tube; FiO2, fraction of inspired oxygen; HFNC, high-flow nasal cannula; ICU, intensive care unit; NIV, non-invasive ventilation; PaO2, partial pressure of oxygen in arterial blood; PICU, paediatric intensive care unit.
The health care quality dimensions addressed most frequently by the final recommendations were clinical effectiveness and patient safety.
DiscussionIn this study, we developed a set of “do not do” recommendations for the field of paediatric intensive care in Spain through the collaboration of a large number of paediatric intensive care specialists throughout the country. To do this, we used the Delphi method, commonly applied to quality control studies, to establish the general opinion of a group of experts following a consensus process, thereby completing a project of the SECIP, which defined a set of quality indicators a few years ago with a similar methodology38. The study also provided an overall of PIC in Spain, which is very useful given the different levels of care that PICUs offer in Spain, among which only a minority manage certain conditions (transplantation, cardiac surgery, etc.). In addition, although originally the Delphi method was very costly on account of the successive gatherings of experts it required, in recent years it has been used by groups of experts that are geographically distant11, which is particularly practical in certain times, such as the present period, in which the SARS-CoV-2 pandemic precluded any scientific gathering.
We ought to highlight the diversity of the professional profiles of the experts who participated in the study. Rather than considering it a drawback, we think that it reflects the reality of our scientific society (the SECIP), a particularly young society the scope of which sometimes overlaps with other fields of paediatric care.
On the other hand, we believe that this study offers contributions genuinely focused on paediatric care as regards what “not to do”. Not only did we not simply adopt the DNDRs of the SEMICYUC7, as evinced by the fact that only 6 of them made it to the last phase of the study, but the final set includes DNDRs that are truly innovative or pioneered in PIC. Two examples are the recommendations not to conduct medical and nursing rounds separately or not to impose strict or restricted hours for family visits. These are practices that are being implemented in intensive care as part of the effort to deliver more humane care in this specialty.
Something worth highlighting is that the dimensions predominantly addressed in the selection of DNDRs were patient safety and clinical effectiveness. This probably reflects the nature of intensive care, which seeks to solve problems without creating additional ones. This can be seen in measures taken to avoid iatrogenicity due to the use of hypotonic saline solutions, to avoid malnutrition during the PICU stay, to prevent the irrational use of antibiotics or to avoid delaying initiation of renal replacement therapy when indicated, to provide a few examples of the DNDRs with the highest agreement and which refer to situations that may still be too frequent in Spanish PICUs.
Another aspect worth mentioning is that some of the recommendations seek not only to reduce risk, but also to increase the efficiency of our work, for instance, avoiding routine laboratory testing or head computed tomography (CT) scans in patients with traumatic head injury showing no signs of deterioration.
Equally interesting is the “paediatric nature” of this set of DNDRs, which focus not only on the patient but also on the close environment, for instance, the recommendation not to routinely make parents leave when invasive procedures are going to be performed or the recommendation to avoid conveying information in an improvised or non-standardised manner. In fact, we found some overlap in the recommendations made from different areas of expertise, such as the recommendation to not hinder the presence of family members during procedure issued from the areas of resuscitation, ethics and safety. We chose to keep all such proposals because we believed that they reflected efforts from different subspecialties of intensive care toward the same goal, which is to facilitate the presence of parents and caregivers in our units, perhaps, as noted above, a practice not as extended as would be ideal in paediatric intensive care.
We also observed recurrent proposals from different sources of DNDRs meant to improve communication and information in the PICU (joint rounds, presence of family members, standardised handoff practices…), which could contribute to the prevention of adverse events in Spanish PICUs, given how frequently communication problems are involved in the development of adverse events in inpatient units39.
Our study is not free of limitations, some of them intrinsic to its methodology, such as the heterogeneity in the professional experience of the participants or the variable involvement of members of different working groups over time. In addition, the expert opinions were limited by the current evidence supporting the proposed recommendations, which also varied across the set of recommendations obtained in the study. Thus, this work reflects a specific time and particular circumstances. Lastly, the method itself, based on the asynchronous exchange of information by electronic mail as opposed to in-person gatherings, obstructed the process in some instances and resulted in delays relative to the deadlines originally established, which posed a challenge to the coordinators of the study.
We believe that this study underscores both undesirable practices that ought to be corrected in Spanish PICUs as well as practices that have yet to be generalised and whose implementation could help improved the safety and quality of paediatric intensive care in Spain. This set of recommendations could be a care quality improvement tool, helping reduce variability in paediatric intensive care in Spain, prevent the iatrogenic effects of unnecessary interventions and promote adequate and responsible use of health care resources as well as the search for care practices that are efficient and satisfactory for our patients and their families.
FundingThis research did not receive any external funding.
Conflicts of interestThe authors have no conflicts of interest to declare.
We are thankful for the disinterested collaboration of a large number of paediatric intensive care colleagues members of working groups of the Sociedad Española de Cuidados Intensivos Pediátricos (SECIP). We want to particularly thank some of them for their especial involvement in submitting proposals or evaluating DNDRs: María Teresa Alonso, Francisco José Cambra, Santiago Mencía, Raúl Borrego, José Luis de Unzueta, Alba Palacios, Alberto Salas, Julio Parrilla, Juan Carlos de Carlos, Sylvia Belda, Silvia Redondo, María José Solana, Rafael González, Mario Sánchez, Susana Reyes, Natalia Ramos, Artur Sharluyan, María Dolores Calvo, Reyes Fernández, José Luis López Prats, and the entire working group on safety of the SECIP.
Previous presentation: This study was presented at the XXXV Congress of the Sociedad Española de Cuidados Intensivos Pediátricos (SECIP), held remotely, May 17–21, 2021.