The aims of this article are to analyse the neuropsychological changes in the medium–term in children subjected to aortic arch surgery using selective cerebral perfusion (SCP), as well as to detect any modifiable factors in the surgical technique that may contribute to minimising the subsequent neurological involvement.
Material and methodsInclusion criteria were established as: aortic arch disease operated on using SCP during the first year of life, between 10 August 2004 and 24 May 2016, biventricular physiology, and gestational age greater than 31 weeks. In the absence of a chromosomal disease, they were classified, from a neurological point of view, using the Rankin score. Children over 4-years of age were subjected to intelligence studies, including attention level, development, and psycho-lingual skills.
ResultsThe study included a total of 82 patients with a mean age of 1.8 months. The mean SCP flow was 32ml/kg/min. The mean time of SCP was 31min. The overall mortality of the series was 14.8%. Neurological dysfunction was observed in 35.9% of patients, and the following were detected as risk factors: surgery in patients less than 10-days-old, duration of SCP greater than 40min, and the time required for the cooling down and/or warming-up. Attention deficit was diagnosed in 35.2% of patients greater than 5-years-old.
ConclusionsPatients operated on using SCP in in the first year of life required a neuropsychological follow-up, and there are modifiable surgical factors that may have an influence on neurological development.
Los objetivos son analizar las alteraciones neuropsicológicas a medio plazo de los niños intervenidos del arco aórtico mediante perfusión cerebral selectiva (PCS) y detectar posibles factores modificables en la técnica quirúrgica que pueden ayudar a minimizar la afectación neurológica posterior.
Material y métodosSe establecieron como criterios de inclusión: patología del arco aórtico intervenida mediante PCS durante el primer año de vida, entre el 10 de Agosto de 2004 y el 24 de Mayo de 2016, fisiología biventricular y edad gestacional mayor de 31 semanas. En ausencia de cromosomopatía se clasificaron desde el punto de vista neurológico siguiendo el modified Rankin score. En mayores de 4 años se realizaron estudios de inteligencia, nivel de atención, maduración y aptitudes piscolingüisticas.
Resultados82 pacientes se incluyeron, cuya edad media en el momento de la cirugía fue de 1,8 meses. El Flujo medio en PCS fue de 32ml/kg/min. El tiempo medio de PCS fue de 31 minutos. La mortalidad global de la serie fue de 14,8 %. Con disfunción neurológica se observaron un 35,9 % y se detectaron como factores de riesgo: cirugía en menores de 10 días de edad, duración de PCS mayor de 40minutos y la duración del enfriamiento y/o calentamiento. Un 35,2 % de los pacientes mayor de 5 años fueron diagnosticados de déficit de atención.
ConclusionesLos pacientes intervenidos en el primer año de vida con PCS precisan un seguimiento neuropsicológico y hay factores modificables quirúrgicos que pueden influir en el desarrollo neurológico.
Congenital heart defects (CHDs) affecting the proximal and medial aortic arch that require surgical repair have traditionally been managed with a median sternotomy under deep hypothermic circulatory arrest (HCA). This technique can be used to set up a bloodless operating field to perform the repair, but it is not free of potential complications and it offers a window of approximately 40min after which the incidence of neurodevelopmental abnormalities increases exponentially.1 In the late 1990s, the technique of selective cerebral perfusion (SCP) was developed, and its use has since become widespread in the management of severe aortic arch disease in place of HCA.2,3 This approach consists in selectively maintaining cerebral perfusion through the supra-aortic vessels while the rest of the body is subjected to total ischaemia. In theory, SCP is more advantageous from a neurologic perspective compared to HCA, although the published evidence on the subject is scarce. Selective cerebral perfusion offers a longer “safe” window for surgical repair and is associated with fewer short-term complications, but there are no data on the likely neurologic complications in the medium and long terms.4,5
The aim of this study was to analyse neuropsychological abnormalities in the medium term in children that underwent aortic arch repair under SCP and identify potential modifiable factors in the SCP protocol that could contribute to minimising future neurologic impairment.
Material and methodsWe conducted an observational descriptive study in patients with aortic arch anomalies that underwent surgical repair via median sternotomy under SCP.
The inclusion criteria were aortic arch anomaly repaired under SCP in the first year of life between August 10, 2004 and May 24, 2016, two-ventricle physiology and gestational age greater than 31 weeks.
The indication for surgery in case of obstruction at the aortic arch level was established based on the presence of symptoms of heart failure, hypertension in the upper extremities and left ventricle hypertrophy or dilatation. The obstruction was considered significant in case of detection on echocardiography of a mean blood pressure gradient of 20mmHg or greater at the level of the aortic arch with diastolic prolongation.
The indication for surgical repair in the neonatal period was the presence of symptoms or the need for prostaglandin (PGE) infusion to maintain the blood flow to the descending aorta through the ductus arteriosus. In asymptomatic infants that do not require PGE, surgery was performed after 1 month of life, applying the aforementioned criteria.
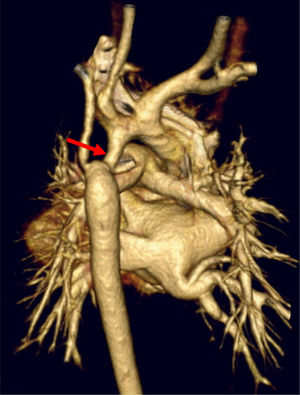
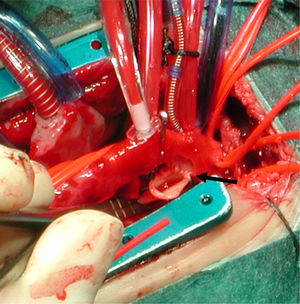
The surgical approach was a median sternotomy with extracorporeal circulation (ECC) and SCP. The narrowing of the aortic arch was repaired via median sternotomy in case of hypoplasia of the proximal or medial arch, interrupted aortic arch or association with a cardiac defect requiring concomitant surgery with a midline approach (Figs. 1 and 2).
We collected data on demographic, preoperative, perioperative and postoperative variables. The follow-up of patients included evaluations in the paediatrics, paediatric neurology, paediatric cardiology and paediatric cardiac surgery departments. Children aged more than 5 years also underwent evaluations in the Paediatric Psychology department.
We made a general classification of patients by neurologic status applying the modified Rankin score (mRS),6 categorising patients as having “neurologic disability” if they had a mRS score of 2 or higher. Neurologic disability was defined as the patient requiring help with some daily activities, with both the physician and the patient or family agreeing on the presence of neurologic impairment. We also established a category of patients with severe neurologic disability characterised by the need for assistance in attending to bodily needs and performing daily activities. We excluded patients with chromosomal disorders. Patients aged 5 or more years were evaluated in the paediatric psychology department, including administration of the Kaufman Brief Intelligence Test (KBIT), assessment of attention (Children Sustained Attention Task [CSAT], Rey, Evaluation of Deficit of Attention and Hyperactivity scale [EDAH] and Diagnostic and Statistical Manual of Mental Disorders, 5th Edition [DSM-V]), Pascual graphomotor test and Illinois Test of Psycholinguistic Abilities (ITPA).
At the outset, we informed the patients or family about the study and obtained specific informed consent, and the study adhered at all times to current low on data protection. The study was approved by the clinical ethics committee. We collected the data in a database and performed the analysis using the software SPSS version 20 (IBM®). We considered differences statistically significant if the probability of a type I error was less than 5% (P<.05).
ResultsA total of 82 patients met the inclusion criteria, of who 81 agreed to participate in the study. Thirty-five were aged more than 5 years and underwent a psychological evaluation, 36 (43.9%) were female and 26 (31.7%) had an associated severe CHD (dextro-transposition of the great arteries, truncus arteriosus, severe aortic stenosis or Shone complex). In 53 patients (64.6%), the systemic circulation dependent on the patency of the ductus arteriosus. The mean age at the time of surgery was 1.8 months, with a median of 0.5 months (range, 0.1–32 months).
Cardiac surgery with SCP took place before 10 days post birth in 22 cases (26.8%). The mean flow rate used in SCP was 32mL/kg/minute. The mean duration of SCP was 31min, with a median of 30 and a range of 16−66min. The mean cooling time was 31min (8–60) and the mean rewarming time 43min (15–90).
The overall mortality in the sample was 14.8%, with an in-hospital mortality of 12.3% and a mean duration of follow-up of 48 months. The factors significantly associated with mortality were association with complex heart disease and surgery before 15 days post birth (Table 1).
Comorbidities, time and cause of death.
| Patient | Type of aortic arch defect | Associated heart defect | Death after surgery |
|---|---|---|---|
| 1 | IAA-type A | TGV-VSD. PRN: 1.580 g | + 1 day |
| 2 | IAA-type A | Truncus arteriosus | + 1 day |
| 3 | Hypoplastic aortic arch | Complete AV canalSevere AV valve regurgitation | + 1 day |
| 4 | Hypoplastic aortic arch | VSD. Severe PHTN grave | + 2 monthsSevere neurologic damage. Withholding of treatment |
| 5 | Hypoplastic aortic arch | TGV. Taussig Bing | + 4 daysECMO |
| 6 | Hypoplastic aortic arch | Sever Shone complex | + 6 months. Multiple percutaneous procedures. Ross-Konno procedure |
| 7 | Hypoplastic aortic arch | TGV. Taussig Bing | + 1 day |
| 8 | Hypoplastic aortic arch | Shone complex | + 28 days. Bronchiolitis by RSV. ECMO |
| 9 | Hypoplastic aortic arch | Truncus arteriosus | + 8 days. ECMO. |
| 10 | Hypoplastic aortic arch | Severe PHTN | + 7 days |
| 11 | Hypoplastic aortic arch | Severe Shone complex | + 3 years. Late mortalitySeveral surgeries (Ross-Konno. Mitral valve replacement) |
| 12 | Hypoplastic aortic arch | VSD | + 2 years. Late mortalityGoldenhar syndrome associated with severe respiratory illness |
AV, atrioventricular; BW, birth weight; ECMO, extracorporeal membrane oxygenation; IAA, interrupted aortic arch; PHTN, pulmonary hypertension; RSV, respiratory syncytial virus; TGV, dextro-transposition of great vessels; VSD, ventricular septal defect.
Recoarctation occurred in 20.7% of patients, out of which 76.4% required percutaneous transluminal balloon dilation angioplasty.
There was evidence of neurologic impairment in 35.9% (23 patients) of the total of 64 patients under study. The risk factors for neurologic impairment identified in the study were surgery before 10 days post birth, duration of SCP greater than 40min, cooling time of less than 15min or greater than 40min during ECC and rewarming time of more than 40min during ECC (Table 2).
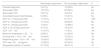
Univariate analysis of the association between different variables and risk factors with neurologic impairment.
| Neurologic impairment | No neurologic impairment | P | |
|---|---|---|---|
| Prenatal diagnosis | 5 (21%) | 12 (26%) | Ns |
| Associated VSD | 16 (70%) | 26 (56%) | Ns |
| Associated TGV | 2 (8.7%) | 3 (6.5%) | Ns |
| Associated severe heart disease | 6 (26%) | 10 (21%) | Ns |
| SCP at < 10 days post birth | 11 (47%) | 8 (17%) | .009 |
| SCP at < 30 days post birth | 17 (73%) | 28 (60%) | Ns |
| SCP at > 30 days post birth | 7 (33%) | 14 (66%) | Ns |
| SCP at 15−30 days post birth | 5 (17%) | 19 (37%) | .06 |
| SCP > 40min | 11 (47%) | 7 (15%) | .04 |
| Minimum temperature > 23°C | 8 (34%) | 21 (45%) | Ns |
| Cooling time < 15 or > 40min | 10 (44%) | 10 (21%) | .05 |
| Rewarming time < 15 or > 40min | 15 (65%) | 18 (40%) | .04 |
| SCP rate > 35mL/kg/min | 12 (52%) | 25 (54%) | Ns |
| Reoperation before 12 months | 21 (75%) | 46 (51%) | .07 |
Data expressed as n (%). Statistical significance defined as P< .05.
Prenatal diagnosis includes patients with a definitive diagnosis of cardiac defect in a prenatal ultrasound examination. Associated severe heart disease includes great vessel transposition, truncus arteriosus and severe aortic stenosis.
Ns, not significant; SCP, selective cerebral perfusion; TGV, transposition of the great vessels; VSD, ventricular septal defect.
During the follow-up, 18 (35.2%) of the 51 patients assessed by the child psychologist and the paediatric neurology department received a diagnosis of attention-deficit hyperactivity disorder (ADHD).
Out of the total sample of 64 patients, 13 (20.3%) were classified as having severe neurologic disability. The factors significantly associated with severe neurologic impairment were surgery before 10 days post birth, a SCP flow rate greater than 35mL/kg/minute, cooling time of less than 15min or more than 40min, rewarming time of more than 40min, a preoperative haematocrit greater than 30%, an intraoperative base excess of 2 mEq/L, presence of ventricular septal defect (VSD) and early recoarctation and reoperation with ECC in infants aged less than 12 months.
On the other hand, surgery performed between 15 and 30 days post birth appeared as a protective factor against severe neurologic impairment.
Thirty-five patients aged more than 5 years without chromosomal disorders underwent a psychological evaluation, and 13 (37.1%) received a diagnosis of ADHD. The mean score in the test that assessed maturity in drawing (Pascual graphomotor test) was 85, with a standard deviation of 18. The Pascual graphomotor test was administered to 35 children, yielding a mean score of 85 with a standard deviation of 18.
We did not find statistically significant differences in the level of intelligence of these patients compared to the general population. However, the ITPA did detect significant abnormalities in psycholinguistic abilities, especially in the processing of information (auditory association and memory).
DiscussionThe published case series of patients operated for correction of the aortic arch under SCP in the first year of life report an overall mortality of 7%–15%.7,8 The mortality decreases to around 3% in patients with isolated anomalies of the aortic arch,9 and the mortality in this specific subset in our series was of 1.8%.
The goals of surgical management for coarctation of aorta are not limited to resolving the current problem, as efforts should be made to prevent future recoarctation and the need of additional surgical or percutaneous catheter interventions.10 In recent years, there has been a generalised trend toward the use of medial sternotomy and repair with aortic arch advancement techniques and SCP, especially in patients with hypoplastic aortic arch. Some studies in large samples, such as the study by Sakurai et al. in Birmingham (United Kingdom), suggest that the incidence of coarctation of the aorta associated with hypoplasia of the aortic arch has been increasing from 12% in the past decade to 20%–25% in current times,11 with an increase in the use of sternotomy and SCP for surgical management. From a haemodynamic standpoint, SCP is associated with improved outcomes and a reduced frequency of reoperation, but there are no medium- to long-term studies of neurologic outcomes exploring whether the increased safety in the performance of anastomosis and repair of associated defects could be offset by a negative impact in subsequent neurodevelopment.12
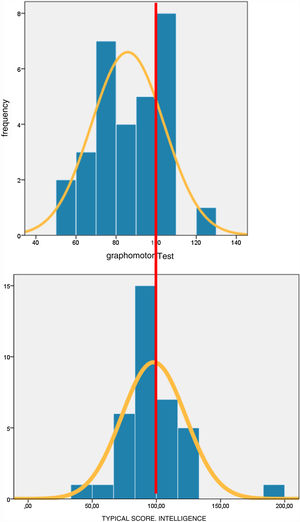
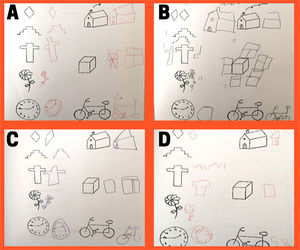
Study of risk factors for neurologic impairmentAn instrument that has proven very useful in neurologic screening is the Pascual graphomotor test, which assesses the maturity of drawing in children.13 The tasks performed in the test involve visual perception, integration of visual information, hands-on reasoning and fine motor skills. This test focuses on nonverbal intelligence. Compared to the histogram of the scores in the KBIT used to assessed intelligence, the histogram corresponding to the Pascual graphomotor test scores was skewed to the left (Fig. 3).
The histogram of the scores (Fig. 3) shows that in our sample, the distribution was skewed left compared to the general population.
The graphomotor test is an instrument validated in the healthy population and individuals with different neurodevelopmental disorders.14–16 It is easy to administer; in our study, the child made the drawings required for the test while the paediatric neurologist interviewed the parents (Fig. 3). We found that a score below 70, which corresponded to a z-score of –1 in our sample, was associated to severe neurologic impairment and disability. If we increased the threshold to 80, corresponding to a z-score of –1 in the reference population in which the test was validated, lower scores were associated significantly not only with neurologic impairment, but also with the presence of ADHD and special education needs. This is a valuable screening tool in our paediatric patients because it offers a simple means to assess nonverbal intelligence, visual integration, fine motor skills and the probability of requiring learning support during schooling.
When we studied the distribution of the intelligence quotient z-scores in our sample (Fig. 3), we found that it was similar to the distribution in the general population, and did not find a skewing to the left, which suggests that the attention deficits observed in our patients were not related to intelligence (Fig. 4).
Assessment of graphomotor skills through drawing. Pascual graphomotor test. A) Age 7 years. Test score: 100. Normal neurodevelopment, no ADHD. B) Age 6 years. Test score: 127. No neurologic impairment. High level for age. C) Age 7 years. Test score: 74. Neurologic impairment, no ADHD. D) Age 6 years. Test score: 66. Neurologic impairment, ADHD.
ADHD, attention-deficit hyperactivity disorder.
When we performed a subgroup analysis of the patients that eventually received a diagnosis of ADHD, we did not find an association between this disorder and the potential risk factors for neurologic impairment described in previous sections (age at date of surgery, duration of SCP, abnormal cooling or rewarming, severe cardiac comorbidity). This suggests that the pathophysiological mechanism involved in the development of ADHD is multifactorial (environmental and genetic and other type of factors) and does not depend solely on the presence of a CHD and the surgical management.
From a neurologic perspective, what is the best time to conduct surgery with SCP in children with severe aortic arch anomalies?The ideal timing of surgery in this group of patients is difficult to determine. It is important to find the right balance between allowing the child to mature as much as possible and avoiding delays in managing the clinical condition leading to significant deterioration before surgery. It is fair to assume that if the infant is clinically stable, ventricular function is good, the left ventricle is not enlarged or excessively hypertrophic, tissue perfusion is adequate and PGE is well tolerated, surgery could be delayed a few days, but how many days exactly is unknown. If the hypoplastic aortic arch is associated with a complex cardiac disease, the window for performing surgery narrows to a minimum.
The univariate analysis identified performance of aortic arch repair with SCP before 10 days post birth as a risk factor for future neurologic impairment. Another variable that was close to being statistically significant in the analysis (P =0.058) was surgery between 15 and 30 days post birth, which was associated with a decrease in overall neurologic impairment, and surgery in this time range was significantly associated with a lower incidence of severe neurologic impairment (P =0.04). This finding may be helpful in guiding the selection of an optimal time frame for surgery in terms of neurologic outcomes, corresponding approximately to 15–30 days post birth. We did not find evidence of an improvement in neurologic outcomes or a reduction in mortality in children operated after 30 days post birth.
Are there any other intraoperative modifiable risk factors?Other risk factors that could affect neurodevelopmental outcomes and that were statistically significant in the univariate analysis were a duration of SCP greater than 40min, very rapid cooling (< 15min) or very slow cooling (> 40min) and very slow rewarming.
One of the reasons that SCP has displaced HCA for neuroprotection during aortic arch surgery was the narrow time window of the latter. There are studies in the literature that demonstrate that after 30min of HCA, the probability of a negative impact on neurodevelopment is considerable. But it seems that time is also a concern in SCP. Some studies have suggested thresholds of 50−70min,17 but in our patients we found that neurologic impairment increased considerably starting from 41min of SCP.
When it comes to complex procedures with uncertain repercussions, it is difficult to establish a causal relationship between the procedures themselves and the complications that develop afterward. There is no question that multiple variables are at play in these patients, overall and in relation to the use of SCP. We know that if these children do not undergo surgery, their life expectancy is negligible, but also that SCP is not entirely harmless.18,19 To attribute the complications associated with SCP merely to the duration of surgery is to grossly oversimply this very complex matter. Other variables that stood out in our statistical analysis were the cooling time and the rewarming time. We were unable to determine the ideal target temperature in the statistical analysis, probably because the lowest temperature achieved was pretty homogeneous in the sample. What our findings did suggest was that cooling or rewarming that were abnormal by being either too quick (< 15min) or too slow (> 40min) were associated with moderate neurologic impairment, affecting our patients’ ability to perform daily activities and take care of their own needs.
In the analysis of patients with severe neurologic impairment, defined as those that required near-constant assistance in everyday living, we identified the following risk factors: a flow rate greater than 39mL/kg/minute in SCP, surgery before 10 days post birth, cooling or rewarming time of less than 15min or more than 40min, VSD, early recoarctation and need for reoperation with ECC before age 2 months. All of the above suggests that the immaturity of the brain in the early stages of life is an important determinant in the neurodevelopmental outcomes of these children with CHDs.
The first studies in the literature that analysed a medium- to long-term outcomes in patients that had been subjected to HCA found few significant differences between these patients and the general population in intelligence, motor skills and learning outcomes.20
The Boston circulatory arrest trial21,22 found a clear association between HCA and poorer outcomes in language skills, and the comparison of low-flow cardiopulmonary bypass (which is not exactly the same as SCP) and HCA revealed a higher incidence of ADHD and poorer impulse control in the long term in children operated with low-flow cardiopulmonary bypass (in this case, for correction of dextro-transposition of the great arteries).
It is possible that the areas of the brain responsible for impulse control may be affected by changes in perfusion during a surgical procedure with an impact on the development of attention and learning abilities in the child. It is likely that the more immature the brain is, the greater the child is at risk of neurologic impairment in future development.
Do children operated for correction of an aortic arch anomaly require neuropsychological follow-up?Follow-up including a comprehensive neuropsychological evaluation is important in children that have undergone surgery with SCP early in life. Early diagnosis and treatment of neurologic disorders, such as ADHD, can have a significant impact on the child’s life.23,24 Preventive early intervention strategies in the preschool period may improve future academic performance and help parents better understand the behaviour of their children. We are aware that at present there are no alternatives to SCP for surgical repair, but we believe that early detection of sequelae and appropriate care may help mitigate its impact and optimise quality of life.
Limitations of the studyThe findings of the study may be limited by the absence of a control group not subjected to SCP and the delivery of care by different providers that may have been a source or variability (5 surgeons and 2 perfusionists).
ConclusionsPatients with aortic arch anomalies that underwent surgical repair with SCP in the first year of life require neuropsychological follow-up in addition to cardiological follow-up to ensure early detection of abnormalities associated with learning disorders and initiate treatment as needed. The management of patients with aortic arch anomalies operated in the first year of life under SCP includes modifiable factors that could have an impact on future neurodevelopmental outcomes, such as the timing of surgery, the flow rate used in SCP, the duration of SCP, the cooling time and the rewarming time during cardiac surgery.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Pérez RS, Requero PT, López LP, Lois JR, Ramchandani BR, Silva LG et al. Evolución neurológica y resultados de la cirugía pediátrica del arco aórtico mediante perfusión cerebral selectiva. An Pediatr (Barc). 2020;93:305–312.