SARS-CoV-2, coronavirus that causes coronavirus disease 2019 (COVID-19), was first detected in Spain on 31 January 2020. On 14 March 2020, a state of emergency was declared in Spain in a bid to control the spread of the COVID-19 pandemic in the country. The aim of our study is to analyze the impact on emergency medicine attendance after the national lockdown, as well as the clinical presentation and the management of patients with suspected COVID-19 in the Paediatric Emergency Department.
Patients and methodsThis retrospective observational study included children and adolescents under the age of 18, attended in our Paediatric Emergency Department during the period March 14 to April 17, 2020.
ResultsA total of 1666 patients were attended during the study period, 65.4% less than in the same period of 2019. Just over half (51.2%) were males, and mean age was 5.4 years. In triage, 39.9% were high priority levels, 6.5% more than 2019. Most frequent reasons for consultation at the Paediatric Emergency Department were fever (26.5%), respiratory symptoms (16.1%), and trauma (15.2%). A total of 218 patients (13%) received a diagnosis of possible COVID-19, with SARS-CoV-2 infection confirmed in 18.4%, and 23.8% (52/218) were hospitalised. At discharge, 44% (96/218) were diagnosed with lower, and 33.9% (74/218) with upper respiratory infection.
ConclusionsDuring the SARS-CoV-2 outbreak, the demand for urgent paediatric care decreased, with the proportion of cases with high priority triage levels increasing. Most of the patients with suspected or microbiological confirmation of COVID-19 had mild respiratory symptoms.
SARS-CoV-2, responsable de la enfermedad por coronavirus 2019 (COVID-19), fue detectado por primera vez en España el 31 de enero de 2020. El 14 de marzo fue declarado el estado de alarma con el objetivo de controlar la pandemia. El objetivo de este estudio es analizar las consecuencias de esta crisis sanitaria sobre el patrón de demanda asistencial, así como el manejo y las características de los pacientes con sospecha de COVID-19 en el Servicio de Urgencias Pediátricas.
Pacientes y métodosEstudio retrospectivo observacional en niños y adolescentes menores de 18 años, atendidos en nuestro Servicio de Urgencias Pediátricas durante el periodo comprendido desde el 14 de marzo hasta el 17 de abril de 2020.
ResultadosDurante el periodo de estudio se atendieron 1.666 pacientes, un 65,4% menos que en el mismo periodo de 2019. La edad media fue de 5,4 años y el 51,2% eran varones. El 39,9% fueron clasificados con niveles de alta prioridad, un 6,5% más que en 2019. Los principales motivos de consulta fueron fiebre (26,5%), síntomas respiratorios (16,1%) y traumatismos (15,2%). Un total de 218 pacientes (13%) fueron diagnosticados de posible COVID-19, confirmándose la infección en el 18,4%. El 44% (96/218) fueron diagnosticados de infección respiratoria inferior y el 33,9% (74/218), superior. El 23,8% (52/218) fueron hospitalizados.
ConclusionesDurante el brote epidémico SARS-CoV-2 disminuyó la demanda de asistencia pediátrica urgente, aumentando la proporción de casos con niveles de triaje de alta prioridad. La mayoría de los pacientes con sospecha o confirmación microbiológica de COVID-19 cursaron con clínica respiratoria leve.
An outbreak of infection by the coronavirus currently known as SARS-CoV-2, which causes coronavirus disease 2019 (COVID-19), was first reported in the city of Wuhan (China) on December 31, 2019. On January 30, 2020, the World Health Organization declared it to the public health emergency of international concern, and on March 11, the outbreak was officially declared a pandemic.
Spain is one of the most affected countries, and one of the regions most affected within it is the Autonomous Community of Madrid (ACM), considered an area of community spread of SARS-CoV-2 since March 12. The declaration of the state of alert by the Spanish government (Royal Decree 463/2020 of 14 March) included population-wide confinement measures to limit the spread of infection.
As the pandemic overwhelmed emergency care units and adult inpatient wards, a restructuring of paediatric care delivery became necessary in the ACM, with paediatric care being diverted and consolidated into 2 specific facilities during the pandemic, one of which is our hospital. However, some hospitals in the ACM have continued to offer paediatric emergency care services to the extent possible and, to a lesser extent, paediatric inpatient care.
The data currently available show that only 2% of affected individuals are aged less than 18 years.1–3 The main symptoms are fever, dry cough and fatigue. There are atypical presentations with gastrointestinal symptoms and few respiratory manifestations. Although most paediatric cases are mild, there have also been severe cases in this age group, with such cases having the potential to rapidly progress to respiratory distress syndrome, septic shock, refractory metabolic acidosis, coagulopathy and multiple-organ failure, and even some deaths have been reported in China and other countries. As occurs in adults, there is evidence of asymptomatic cases and that children may be a source of transmission, as they may shed virus in the stool for more than 1 month.4–8
The aim of our study was to analyze the impact of the pandemic and the declaration of the state of alarm by the Spanish government on the pattern of health care use, and also the characteristics of patients with suspected COVID-19 and their management in the paediatric emergency care setting.
Patients and methodsStudy design and sampleWe conducted a retrospective observational study in children and adolescents aged less than 18 years managed at the paediatric emergency department (PED) of a tertiary care children's hospital in the ACM in the first 35 days since the state of alarm was declared. We compared the demand for health care services, the presenting complaints and the distribution by level of triage compared to the same period in the previous year (2019). The diagnosis of “suspected COVID-19” was based on the judgement of the physician in charge of the patient. The study was approved by the Research Ethics Committee of our hospital.
Inclusion criteria- •
Patients aged less than 18 years, managed in our PED between March 14 and April 17 of 2019 and 2020.
- •
Patients aged more than 18 years with chronic disease followed up in our hospital that received emergency care in the same time periods.
- •
Patients aged more than 18 years that were not being followed up in our children's hospital.
- •
Patients that left the PED before receiving care.
We used the software IBM® SPSS® Statistics 20. We have expressed qualitative data as absolute and relative frequencies and quantitative data as mean and standard deviation (SD) or median and range. We compared groups using the Student t test and the chi square test.
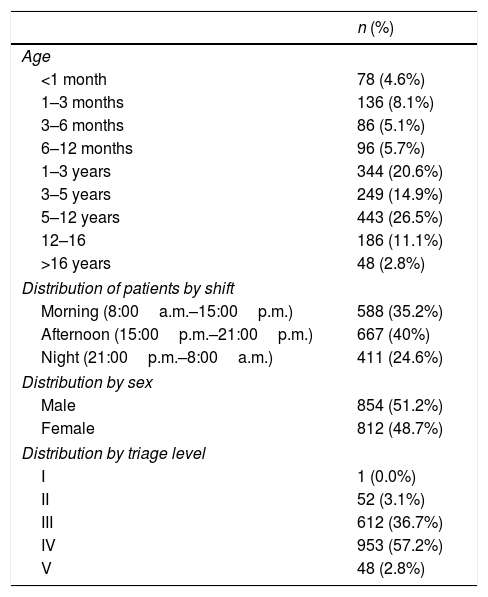
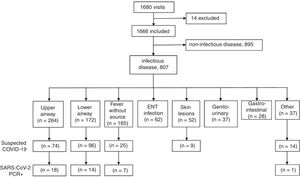
ResultsIn the period under study, our PED received 1680 visits, of which 1666 met the inclusion criteria (compared to 4813 in the same period in 2019, there was a decrease of 65.4%). The PED managed a total of 1429 patients, with a mean of 1.1 visits per patient (range, 1–7 visits/patient); 12.8% made 2 or more visits. The mean number of daily visits was 47.6 (range, 17–76 PED visits/day). Patients stayed in the PED for a mean of 3h and 21min (range, 10min to 22h and 29min) and the rate of hospital admission was 15.1%. The mean age of patients was 5.4 years (SD, 5), and the median was 3.7 years; 51.2% were male (Table 1). Of the total visits, 39.9% were classified as high priority (triage levels i-iii of the paediatric Canadian triage and acuity scale), compared to 33.4% in 2019.
General characteristics (n=1666).
| n (%) | |
|---|---|
| Age | |
| <1 month | 78 (4.6%) |
| 1–3 months | 136 (8.1%) |
| 3–6 months | 86 (5.1%) |
| 6–12 months | 96 (5.7%) |
| 1–3 years | 344 (20.6%) |
| 3–5 years | 249 (14.9%) |
| 5–12 years | 443 (26.5%) |
| 12–16 | 186 (11.1%) |
| >16 years | 48 (2.8%) |
| Distribution of patients by shift | |
| Morning (8:00a.m.–15:00p.m.) | 588 (35.2%) |
| Afternoon (15:00p.m.–21:00p.m.) | 667 (40%) |
| Night (21:00p.m.–8:00a.m.) | 411 (24.6%) |
| Distribution by sex | |
| Male | 854 (51.2%) |
| Female | 812 (48.7%) |
| Distribution by triage level | |
| I | 1 (0.0%) |
| II | 52 (3.1%) |
| III | 612 (36.7%) |
| IV | 953 (57.2%) |
| V | 48 (2.8%) |
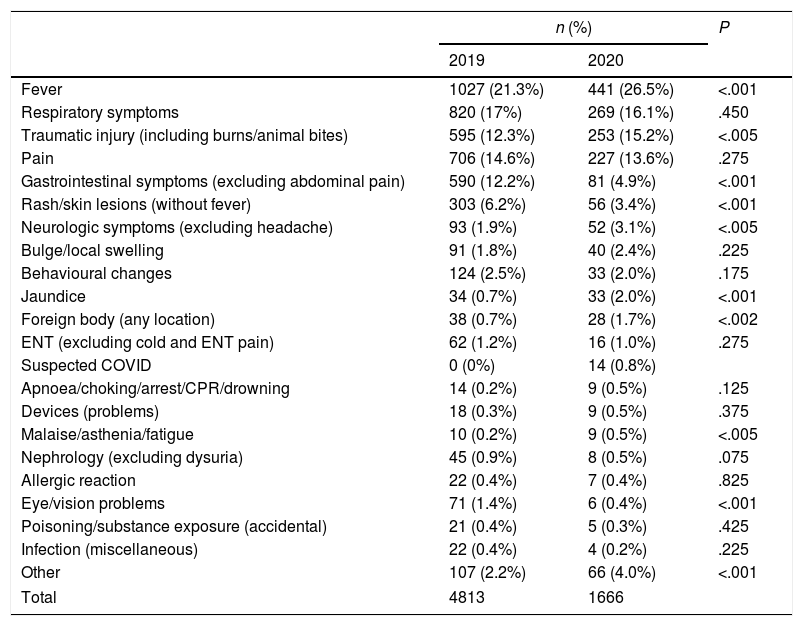
As can be seen in Table 2, the most frequent presenting complaints in the period under study were the same as the previous year, although in some cases the percentage corresponding to some of them increased significantly compared to 2019 (fever, traumatic injury, jaundice, foreign body and fatigue). On the other hand, gastrointestinal symptoms, cutaneous complaints in absence of fever and ophthalmological complaints were less frequent.
Reason for emergency visit (March 14–April 17).
| n (%) | P | ||
|---|---|---|---|
| 2019 | 2020 | ||
| Fever | 1027 (21.3%) | 441 (26.5%) | <.001 |
| Respiratory symptoms | 820 (17%) | 269 (16.1%) | .450 |
| Traumatic injury (including burns/animal bites) | 595 (12.3%) | 253 (15.2%) | <.005 |
| Pain | 706 (14.6%) | 227 (13.6%) | .275 |
| Gastrointestinal symptoms (excluding abdominal pain) | 590 (12.2%) | 81 (4.9%) | <.001 |
| Rash/skin lesions (without fever) | 303 (6.2%) | 56 (3.4%) | <.001 |
| Neurologic symptoms (excluding headache) | 93 (1.9%) | 52 (3.1%) | <.005 |
| Bulge/local swelling | 91 (1.8%) | 40 (2.4%) | .225 |
| Behavioural changes | 124 (2.5%) | 33 (2.0%) | .175 |
| Jaundice | 34 (0.7%) | 33 (2.0%) | <.001 |
| Foreign body (any location) | 38 (0.7%) | 28 (1.7%) | <.002 |
| ENT (excluding cold and ENT pain) | 62 (1.2%) | 16 (1.0%) | .275 |
| Suspected COVID | 0 (0%) | 14 (0.8%) | |
| Apnoea/choking/arrest/CPR/drowning | 14 (0.2%) | 9 (0.5%) | .125 |
| Devices (problems) | 18 (0.3%) | 9 (0.5%) | .375 |
| Malaise/asthenia/fatigue | 10 (0.2%) | 9 (0.5%) | <.005 |
| Nephrology (excluding dysuria) | 45 (0.9%) | 8 (0.5%) | .075 |
| Allergic reaction | 22 (0.4%) | 7 (0.4%) | .825 |
| Eye/vision problems | 71 (1.4%) | 6 (0.4%) | <.001 |
| Poisoning/substance exposure (accidental) | 21 (0.4%) | 5 (0.3%) | .425 |
| Infection (miscellaneous) | 22 (0.4%) | 4 (0.2%) | .225 |
| Other | 107 (2.2%) | 66 (4.0%) | <.001 |
| Total | 4813 | 1666 | |
The most frequent reason for visiting the PED was fever, followed by respiratory symptoms and injuries. We included abdominal pain (6.7% of visits), orofacial pain/ear-nose-throat (ENT) complaints (1.7%), genital pain/nephrological or urological complaints (1.3%) and headache (0.8%) in the “pain” category of presenting complaints. The “behavioural changes” category included episodes of anxiety or agitation (including a suicide attempt) and other complaints such as irritability or food refusal in infants and toddlers.
“Suspected COVID” usually implied the presence of mild symptoms or absence of symptoms in patients with household contacts with confirmed infection.
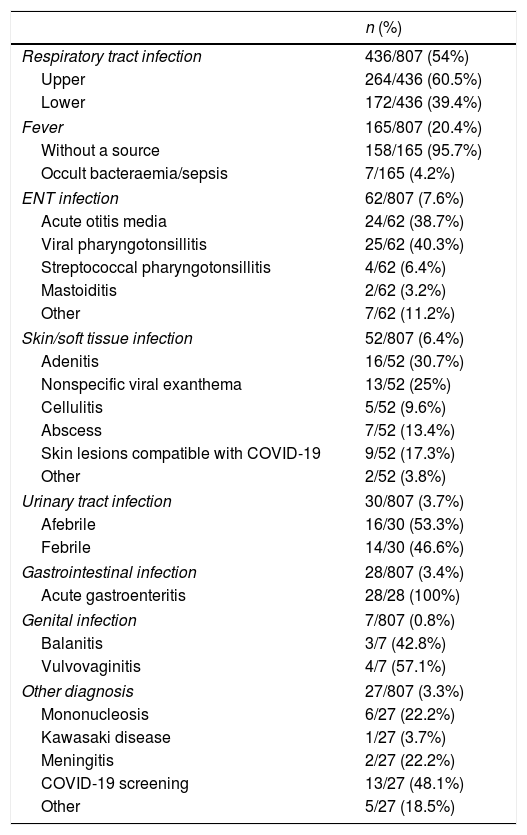
Analysis of discharge diagnosesThe discharge diagnosis was an infectious disease in 48.4% (807/1666) of PED visits (Table 3). In this group, 54% were cases of respiratory tract infection (60.5% of the upper airway and 39.4% of the lower airway) and 20.4% of fever without a source.
Discharge diagnoses: infectious disease (n=807/1666).
| n (%) | |
|---|---|
| Respiratory tract infection | 436/807 (54%) |
| Upper | 264/436 (60.5%) |
| Lower | 172/436 (39.4%) |
| Fever | 165/807 (20.4%) |
| Without a source | 158/165 (95.7%) |
| Occult bacteraemia/sepsis | 7/165 (4.2%) |
| ENT infection | 62/807 (7.6%) |
| Acute otitis media | 24/62 (38.7%) |
| Viral pharyngotonsillitis | 25/62 (40.3%) |
| Streptococcal pharyngotonsillitis | 4/62 (6.4%) |
| Mastoiditis | 2/62 (3.2%) |
| Other | 7/62 (11.2%) |
| Skin/soft tissue infection | 52/807 (6.4%) |
| Adenitis | 16/52 (30.7%) |
| Nonspecific viral exanthema | 13/52 (25%) |
| Cellulitis | 5/52 (9.6%) |
| Abscess | 7/52 (13.4%) |
| Skin lesions compatible with COVID-19 | 9/52 (17.3%) |
| Other | 2/52 (3.8%) |
| Urinary tract infection | 30/807 (3.7%) |
| Afebrile | 16/30 (53.3%) |
| Febrile | 14/30 (46.6%) |
| Gastrointestinal infection | 28/807 (3.4%) |
| Acute gastroenteritis | 28/28 (100%) |
| Genital infection | 7/807 (0.8%) |
| Balanitis | 3/7 (42.8%) |
| Vulvovaginitis | 4/7 (57.1%) |
| Other diagnosis | 27/807 (3.3%) |
| Mononucleosis | 6/27 (22.2%) |
| Kawasaki disease | 1/27 (3.7%) |
| Meningitis | 2/27 (22.2%) |
| COVID-19 screening | 13/27 (48.1%) |
| Other | 5/27 (18.5%) |
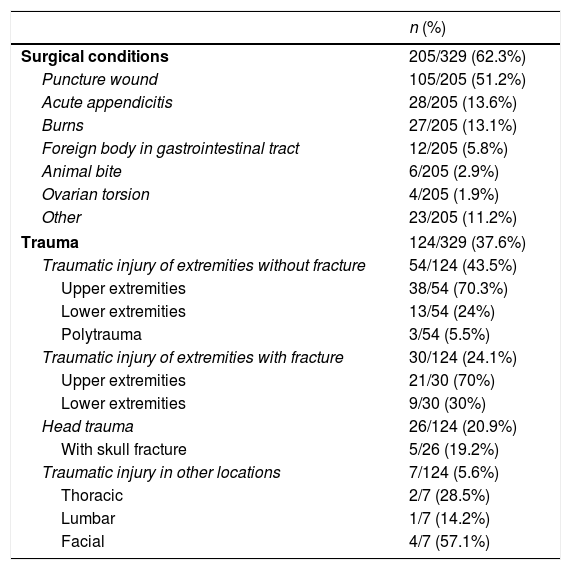
General surgical emergencies (205/1666) and traumatic injuries (124/1666) amounted to 19.7% of the total, with puncture wounds and traumatic injury of an extremity without fracture being the most frequent diagnosis in each of these categories, respectively (Table 4).
Discharge diagnoses: surgical conditions and trauma (n=329/1666).
| n (%) | |
|---|---|
| Surgical conditions | 205/329 (62.3%) |
| Puncture wound | 105/205 (51.2%) |
| Acute appendicitis | 28/205 (13.6%) |
| Burns | 27/205 (13.1%) |
| Foreign body in gastrointestinal tract | 12/205 (5.8%) |
| Animal bite | 6/205 (2.9%) |
| Ovarian torsion | 4/205 (1.9%) |
| Other | 23/205 (11.2%) |
| Trauma | 124/329 (37.6%) |
| Traumatic injury of extremities without fracture | 54/124 (43.5%) |
| Upper extremities | 38/54 (70.3%) |
| Lower extremities | 13/54 (24%) |
| Polytrauma | 3/54 (5.5%) |
| Traumatic injury of extremities with fracture | 30/124 (24.1%) |
| Upper extremities | 21/30 (70%) |
| Lower extremities | 9/30 (30%) |
| Head trauma | 26/124 (20.9%) |
| With skull fracture | 5/26 (19.2%) |
| Traumatic injury in other locations | 7/124 (5.6%) |
| Thoracic | 2/7 (28.5%) |
| Lumbar | 1/7 (14.2%) |
| Facial | 4/7 (57.1%) |
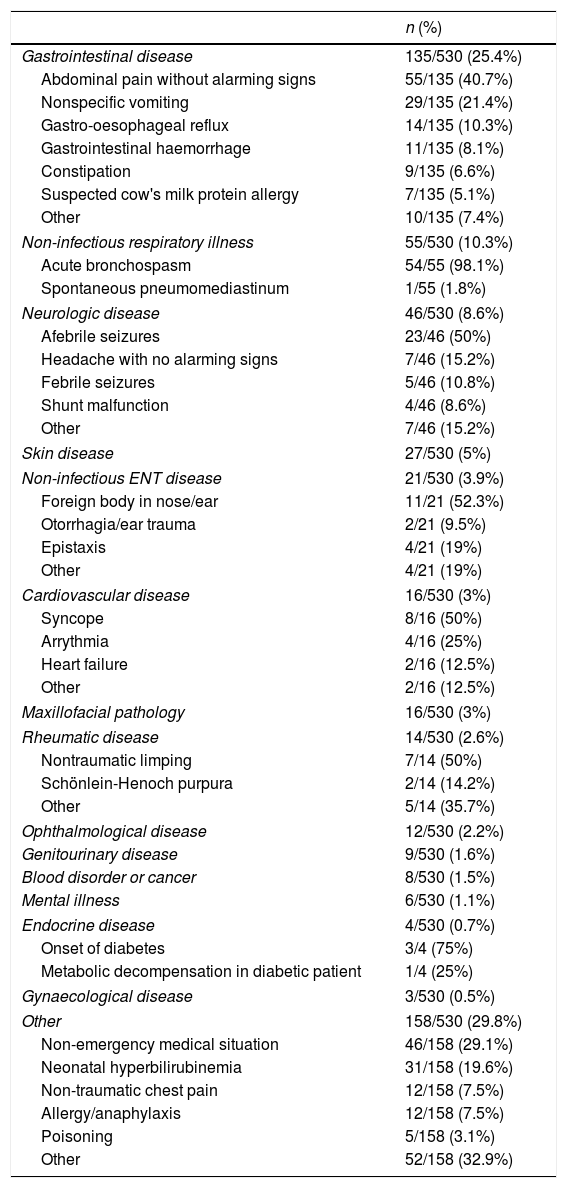
Other frequent diagnostic categories were gastrointestinal disease and non-infectious respiratory disease (Table 5). There was one case of suspected sexual abuse.
Discharge diagnoses other than infectious disease (n=530/1666).
| n (%) | |
|---|---|
| Gastrointestinal disease | 135/530 (25.4%) |
| Abdominal pain without alarming signs | 55/135 (40.7%) |
| Nonspecific vomiting | 29/135 (21.4%) |
| Gastro-oesophageal reflux | 14/135 (10.3%) |
| Gastrointestinal haemorrhage | 11/135 (8.1%) |
| Constipation | 9/135 (6.6%) |
| Suspected cow's milk protein allergy | 7/135 (5.1%) |
| Other | 10/135 (7.4%) |
| Non-infectious respiratory illness | 55/530 (10.3%) |
| Acute bronchospasm | 54/55 (98.1%) |
| Spontaneous pneumomediastinum | 1/55 (1.8%) |
| Neurologic disease | 46/530 (8.6%) |
| Afebrile seizures | 23/46 (50%) |
| Headache with no alarming signs | 7/46 (15.2%) |
| Febrile seizures | 5/46 (10.8%) |
| Shunt malfunction | 4/46 (8.6%) |
| Other | 7/46 (15.2%) |
| Skin disease | 27/530 (5%) |
| Non-infectious ENT disease | 21/530 (3.9%) |
| Foreign body in nose/ear | 11/21 (52.3%) |
| Otorrhagia/ear trauma | 2/21 (9.5%) |
| Epistaxis | 4/21 (19%) |
| Other | 4/21 (19%) |
| Cardiovascular disease | 16/530 (3%) |
| Syncope | 8/16 (50%) |
| Arrythmia | 4/16 (25%) |
| Heart failure | 2/16 (12.5%) |
| Other | 2/16 (12.5%) |
| Maxillofacial pathology | 16/530 (3%) |
| Rheumatic disease | 14/530 (2.6%) |
| Nontraumatic limping | 7/14 (50%) |
| Schönlein-Henoch purpura | 2/14 (14.2%) |
| Other | 5/14 (35.7%) |
| Ophthalmological disease | 12/530 (2.2%) |
| Genitourinary disease | 9/530 (1.6%) |
| Blood disorder or cancer | 8/530 (1.5%) |
| Mental illness | 6/530 (1.1%) |
| Endocrine disease | 4/530 (0.7%) |
| Onset of diabetes | 3/4 (75%) |
| Metabolic decompensation in diabetic patient | 1/4 (25%) |
| Gynaecological disease | 3/530 (0.5%) |
| Other | 158/530 (29.8%) |
| Non-emergency medical situation | 46/158 (29.1%) |
| Neonatal hyperbilirubinemia | 31/158 (19.6%) |
| Non-traumatic chest pain | 12/158 (7.5%) |
| Allergy/anaphylaxis | 12/158 (7.5%) |
| Poisoning | 5/158 (3.1%) |
| Other | 52/158 (32.9%) |
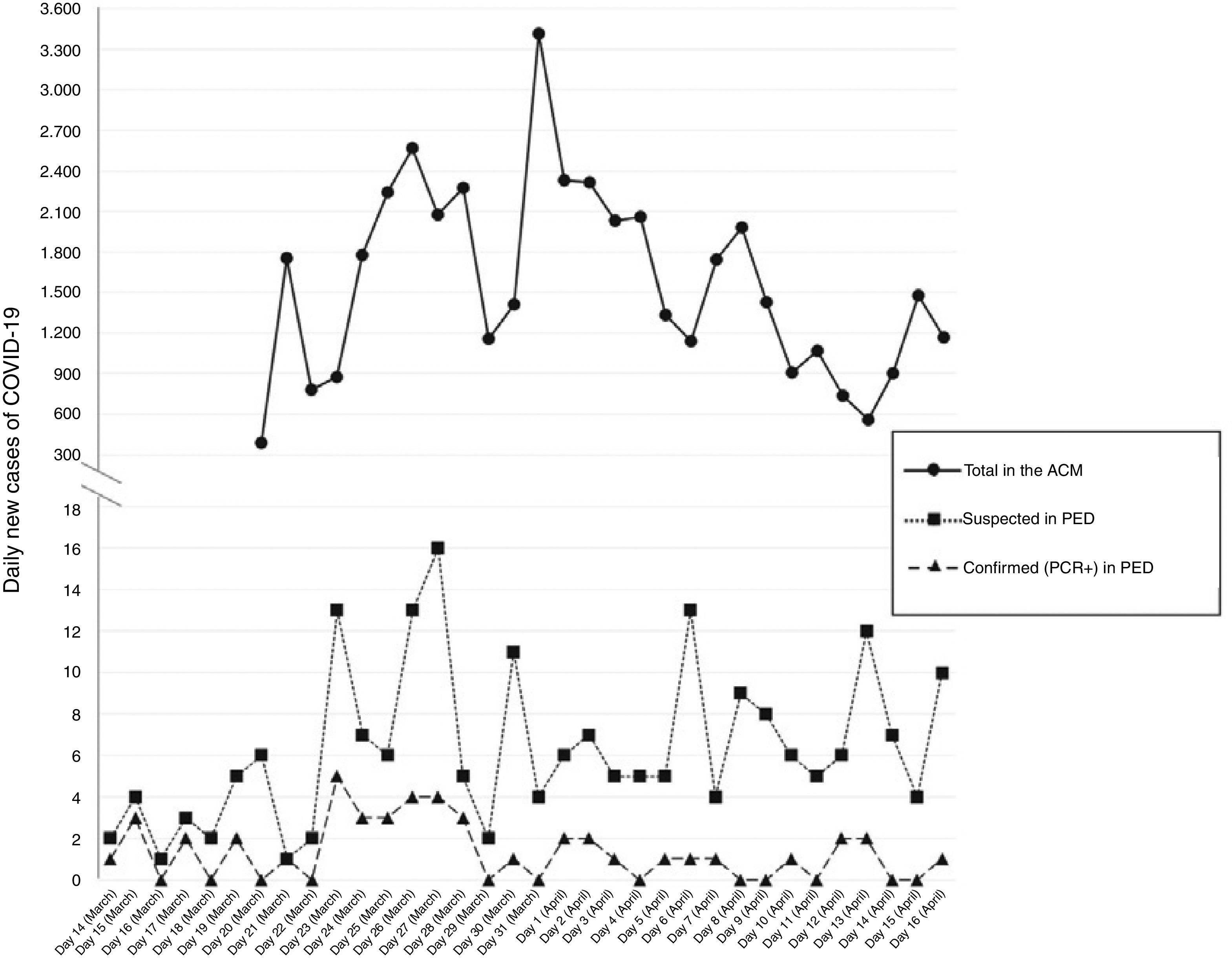
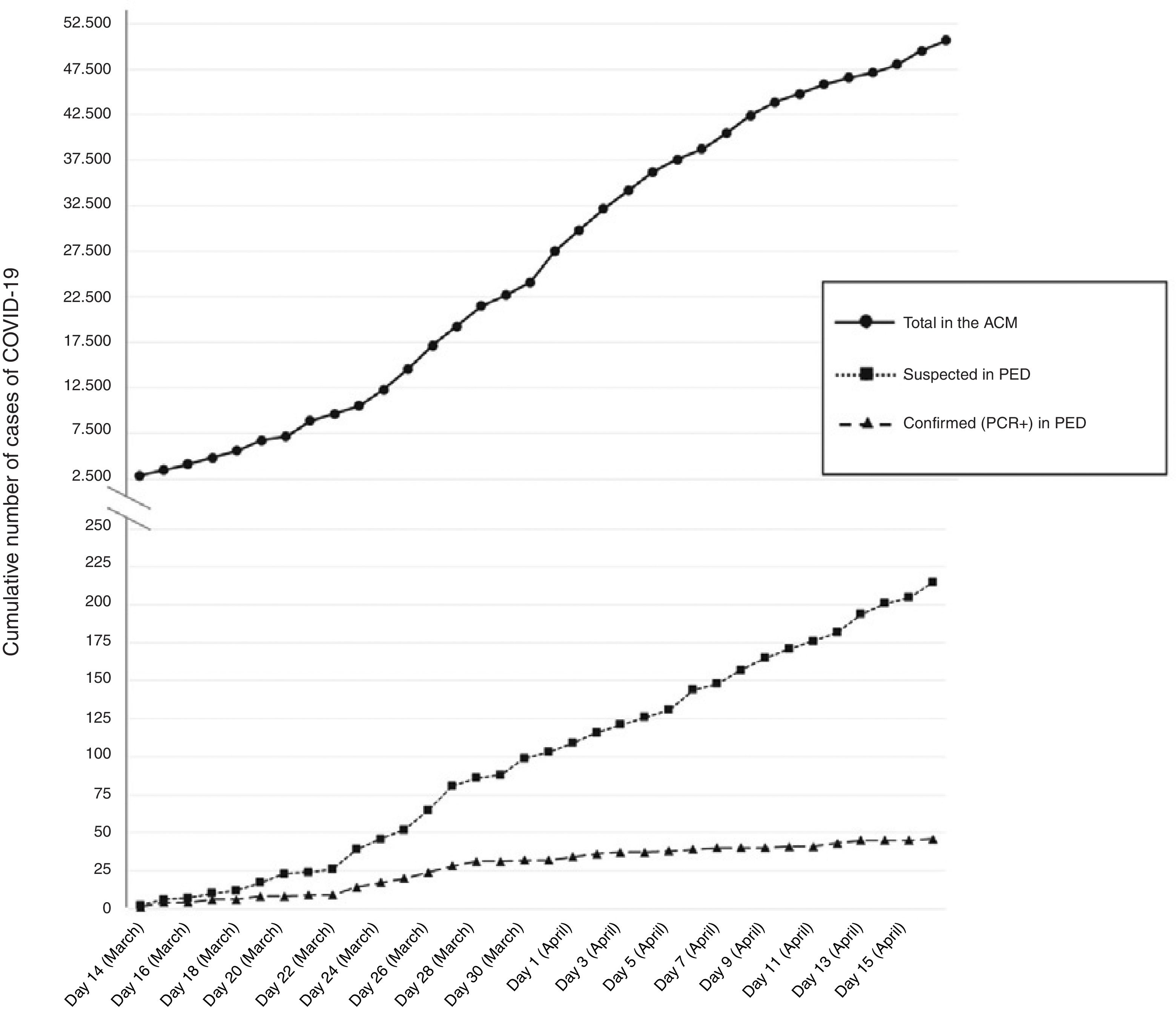
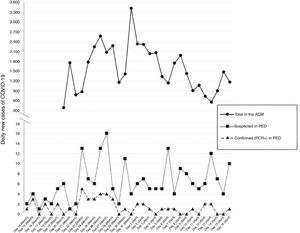
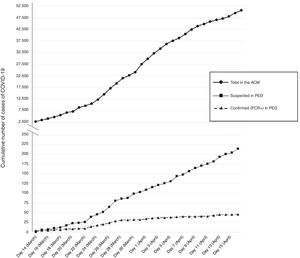
The daily incidence of suspected/confirmed cases of COVID-19 in our PED throughout the study period followed similar trends to those observed in the ACM overall (Fig. 1). The temporal trend in the cumulative number of new cases was consistent with the overall trend in the ACM (Fig. 2), although from week 2 in the period under study there was a slowing down in the number of confirmed cases in the PED (although not in the number of suspected cases).
Daily number of new cases of COVID-19 (suspected and confirmed by PRC) diagnosed at the paediatric emergency department and correlation to the reported daily confirmed cases in the Autonomous Community of Madrid (ACM) in the first 35 days following the declaration of the state of alarm. Source of data for the ACM: Spanish Ministry of Health, Social Welfare and Equality.
Cumulative frequency of new COVID-19 cases (suspected and confirmed by PCR) diagnosed at the paediatric emergency department and correlation to the reported cumulative number of confirmed cases in the Autonomous Community of Madrid (ACM) in the first 35 days following the declaration of the state of alarm. Source of data for the ACM: Spanish Ministry of Health, Social Welfare and Equality.
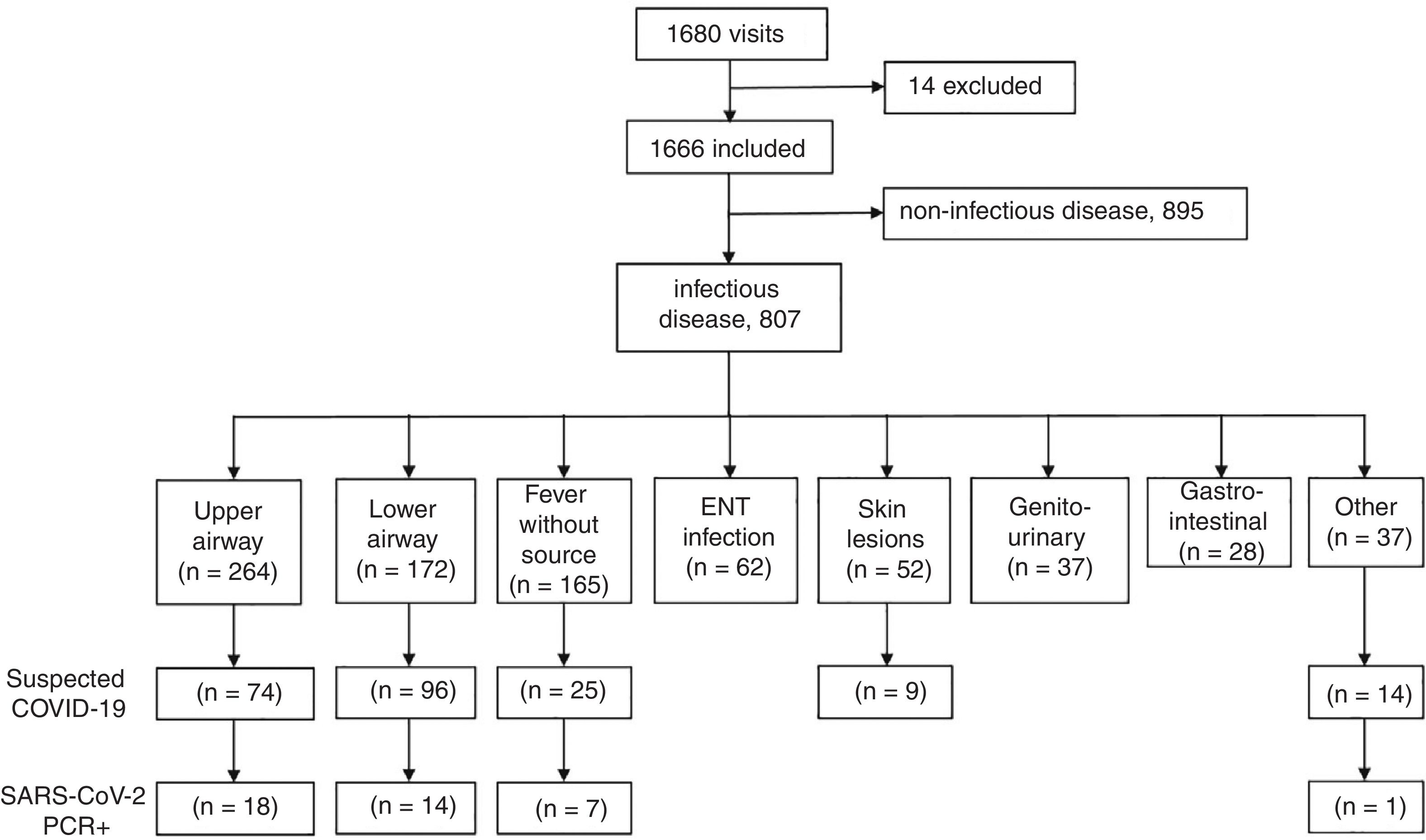
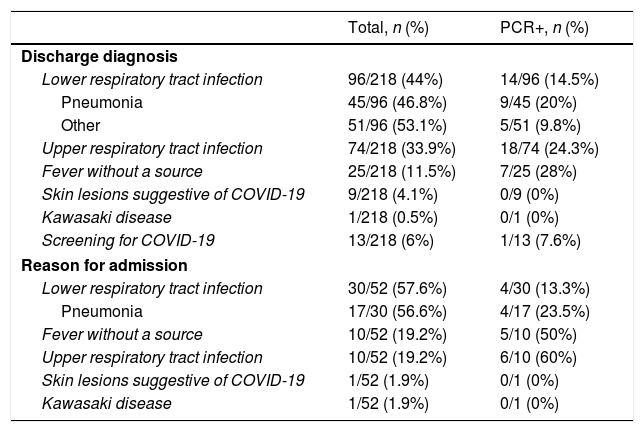
Fig. 3 presents a flowchart of the patients with a discharge diagnosis of infectious disease and suspected COVID-19. A total of 218 patients (13%) received a diagnosis of possible COVID-19. We did not find significant differences in the sex distribution of this group compared to the rest of the sample (52.3% male vs. 51.2% male; P=.770). This subset of patients was slightly older, with a mean age of 6.7 years (SD, 5.3) years compared to 5.2 years (SD, 4.9) (P<.001).
The most frequent discharge diagnosis was lower respiratory tract infection (96/218; 44%), followed by upper respiratory tract infection (74/218; 33.9%), fever without a source (25/218; 11.4%), cutaneous manifestations associated with suspected COVID-19, usually chilblain-like lesions in distal locations (9/218; 4.1%) and Kawasaki disease (1/218; 0.4%). The rest of cases (13/218; 5.9%) corresponded to asymptomatic patients referred to the emergency department for COVID-19 screening (Table 6).
Description of cases diagnosed as possible COVID-19 (n=218).
| Total, n (%) | PCR+, n (%) | |
|---|---|---|
| Discharge diagnosis | ||
| Lower respiratory tract infection | 96/218 (44%) | 14/96 (14.5%) |
| Pneumonia | 45/96 (46.8%) | 9/45 (20%) |
| Other | 51/96 (53.1%) | 5/51 (9.8%) |
| Upper respiratory tract infection | 74/218 (33.9%) | 18/74 (24.3%) |
| Fever without a source | 25/218 (11.5%) | 7/25 (28%) |
| Skin lesions suggestive of COVID-19 | 9/218 (4.1%) | 0/9 (0%) |
| Kawasaki disease | 1/218 (0.5%) | 0/1 (0%) |
| Screening for COVID-19 | 13/218 (6%) | 1/13 (7.6%) |
| Reason for admission | ||
| Lower respiratory tract infection | 30/52 (57.6%) | 4/30 (13.3%) |
| Pneumonia | 17/30 (56.6%) | 4/17 (23.5%) |
| Fever without a source | 10/52 (19.2%) | 5/10 (50%) |
| Upper respiratory tract infection | 10/52 (19.2%) | 6/10 (60%) |
| Skin lesions suggestive of COVID-19 | 1/52 (1.9%) | 0/1 (0%) |
| Kawasaki disease | 1/52 (1.9%) | 0/1 (0%) |
A polymerase chain reaction (PCR) test for detection of SARS-CoV-2 in pharyngeal exudate samples was performed in 180/218 patients (82.6%), which turned out positive in 40/180 (22.2%). In 11 patients (6.1%) the results of PCR testing were inconclusive. The mean age of the patients with a positive PCR test was 6.5 years (SD, 5.9; range, 18 days to 17 years), with a predominance of male patients (67.5%). We did not find significant differences in age (P=.780) or sex (P=.101) compared to the group of with negative PCR results (we excluded cases with inconclusive PCR results from this comparison).
Positive PCR results for COVID-19 were most frequent in the group of patients with a diagnosis of upper or lower respiratory tract infection, although considering the actual proportion of positive results in each diagnostic group, the group with the highest positivity rate corresponded to the patients with fever without a source (7/25; 28%), followed by patients with upper respiratory tract infection (18/74; 24.3%) and patients with lower respiratory tract infection (14/96; 14.5%) (Table 6). There were no PCR-positive cases among patients with suggestive cutaneous manifestations, and a boy aged 5.8 years that was eventually given a diagnosis of Kawasaki disease also tested negative.
The frequency of hospital admission in patients with a possible COVID-19 diagnosis was 23.8%. The most frequent diagnosis at admission was lower respiratory tract infection (57.6%); in this group, there were only 4 cases with a positive PCR test result, all of which occurred in patients in who the chest radiograph evinced the presence of lung consolidation. The highest percentage of confirmed positive cases was found in patients admitted with a diagnosis of upper respiratory tract infection (6/10; 60%). The patients admitted with fever without source and a positive PCR test were 4 patients aged less than 2 months (mean age, 31.5 days; range, 18–52 days) and a female adolescent aged 13 years admitted with fever of 14 days’ duration. Of all hospitalised patients, 17.3% (7 with lower respiratory tract infection and 1 with an upper respiratory tract infection) had respiratory difficulty or hypoxaemia (SatO2<92%). The PCR test was positive in only 2 of these patients.
DiscussionThe declaration of the state of alarm by the Spanish government combined with the imposed measures of population confinement and the perception of risk of health care users have led to a significant drop in the demand for care in our PED compared to 2019, despite the consolidation of paediatric emergency care services in a limited number of hospitals. The suspension of in-person schooling at every level of education in the ACM and the mild presentation of COVID-19 in children6 have also contributed significantly to the decline in the volume of paediatric emergency visits observed since the beginning of this public health crisis.
At the same time, in line with other European countries,9–11 we observed an increase in the complexity of emergency visits, as we found that compared to the same time period in 2019, there was a greater proportion of patients whose triage level on arrival to the PED was in the high-priority range.
The presenting complaints in the study period continued to be the usual reasons for visiting the PED, with fever, respiratory complaints and accidental injuries at the top of the list.12,13 In this sense, we ought to highlight that despite confinement to the home (during the study period, children could not leave the home except in case of demonstrated need), traumatic injuries continued to rank third, once again confirming that the home is a frequent setting of accidents in children.14,15
The low disease activity in paediatric patients, with mild or non-existent symptoms, posed a challenge to the early detection of possible cases at the time of triage. Thus, it was necessary to exercise standard precautions with most patients, treating all of them as potential cases, which involved a significant allocation of time and resources.16 The initial ignorance of the disease, the scarcity of data on paediatric cases, which did not suffice to determine how to manage paediatric patients with complex disease, immunosuppression, etc., and the additional time required to protect the health care staff are factors that unquestionably contributed to increasing the mean duration of the stay in the emergency room (in the case of our PED, 13% greater compared to the same period in the previous year). Had there not been a decline in the volume of patients managed in the department, the duration of the stay may have increased even more, which could have had a deleterious impact on the quality of care.
We share the concern expressed by other authors17 about the reluctance of some parents and caregivers to seek health care, probably motivated by a fear of exposure to coronavirus and by the current limitations in the access to primary care services, as this may result in delayed diagnosis of potentially severe diseases (peritonitis, ketoacidosis, pyelonephritis).9–11 In this regard, some authors have also reported an increase in cases of child abuse and neglect; in our case series, there was only 1 documented case of child sexual abuse.18
As for the temporal distribution of COVID-19 diagnoses in our PED, Figs. 1 and 2 evince the similar trends in the cumulative case number and in the number of new suspected and PCR-confirmed cases in our PED and in the overall ACM. A possible interpretation is that infection in the paediatric population has occurred in parallel to infection in the adult population, with transmissions occurring in the household, as schools were shut down on March 11, 3 days before the declaration of the state of alarm. Performance of population-based studies with serological testing could help confirm household transmission of infection, which, on the other hand, is a very likely phenomenon.
Although in our sample children with a suspected COVID-19 diagnosis were significantly older compared to the rest of the patients in the sample, they were younger compared to the age reported in the study by Dong et al. (median of 7 years in suspected cases and 10 years in confirmed cases)6 or by the Centers for Disease Control and Prevention (CDC) of the United States.19 In contrast, in comparison to other studies in neighbouring regions, patients with suspected COVID in our sample were slightly older compared to the cases in the CONFIDENCE study carried out in Italia or to the cases in 30 health care facilities in the ACM in the first 2 weeks of March 2020 reported by Tagarro et al. (3 years in both cases).1,20
Although in our sample there was a slight predominance of male patients in the cases with confirmed by a SARS-CoV-2 PCR test, we did not find statistically significant differences in the sex distribution of this subset compared to the rest of the sample, which was consistent with previously published case series in China or the United States.6,19
Consistent with the case series of the Wuhan Children's Hospital,21 the most frequent diagnosis in the emergency department was lower respiratory tract infection (pneumonia, bronchiolitis), followed by upper respiratory tract infection, with the 2 combined amounting to nearly 80% of suspected COVID-19 cases. That is, the evidence continues to show that most symptomatic patients have respiratory symptoms.
Although the recent literature includes reports of cutaneous involvement associated with infection by coronavirus as well as cases compatible with Kawasaki disease, we were unable to find a causal relationship in patients in our sample that presented with these symptoms, as microbiological tests in these patients were negative.
The positivity rate for the PCR test for SARS-CoV-2 in our sample (22%) was similar to the rates reported in other studies (34% in the case series in China published by Dong et al.6), although it is important to take into account the limited sensitivities reported for the different tests available (65%–77%) in making interpretations about the actual prevalence of infection in patients with suspected COVID-19.22
In our series, 23.8% of patients with suspected COVID-19 were admitted to hospital. In a fourth of these patients, the suspected infection by SARS-CoV-2 was confirmed by a positive PCR test, a subset that amounted to 35% of the total patients that had a positive PCR result. This percentage is strikingly lower compared to the percentages reported by Parri et al. in Italy20 and Tagarro et al. in Spain1 (in both cases, 60% of cases with a positive test were hospitalised). This difference may be explained by, in the case of the former study, because 25% of the patients were admitted to be quarantined while being asymptomatic, something that was not done in our hospital, and in the case of Spanish study, because in our hospital, in adherence with the directives of the ACM, we tested patients that required admission for any reason or patients with comorbidities that were at greater risk for complications. Since our hospital serves a considerable number of complex patients with many comorbidities, many of them underwent PCR testing for SARS-CoV-2 as part of a more thorough followup, but they were discharged home if they did not have any clinical manifestations that justified admission.
The most frequent reason for hospital admission in patients with suspected COVID-19 was lower respiratory tract infection. Only 2 of the patients with confirmed COVID-19 met the criteria for severe disease proposed by Dong et al.,6 which amounted to 5% of all confirmed cases, a percentage that was identical to the one reported by these authors. Half of the patients admitted with fever without a source had a positive SARS-CoV-2 PCR test result. Of these 10 patients, 6 were aged less than 1 month and another less than 3 months, which may have motivated their admission despite having mild cases of disease based on the definition of Dong et al.
There are several limitations to this study. Firstly, the reorganization of emergency care in the ACM, with reductions or a complete shutdown of paediatric services in many hospitals, makes it difficult to interpret the actual impact of the pandemic on the demand for paediatric emergency care in the department. Another significant limitation is that we were unable to perform a subsequent followup with additional microbiological tests (repeat PCR SARS-CoV-2 test or antibody test) in patients with suspected COVID-19 and negative results of the PCR test performed in the PED. On the other hand, given the policies concerning microbiological testing in the early weeks of the outbreak, it is possible that some patients with low clinical suspicion for COVID-19 or that did not met the criteria for admission were discharged from the PED with alternative diagnoses and were not investigated as possible cases of COVID-19. For the same reason, we were unable to analyze the prevalence of asymptomatic carriage of SARS-CoV-2 in patients that consulted due to close contact with cases of infection in the household and other reasons.
ConclusionsThe SARS-CoV-2 pandemic has led to a decrease in the demand for paediatric emergency care in our population, accompanied by an increase in the proportion of cases corresponding to a high triage level.
Most paediatric patients with suspected or confirmed COVID-19 presented with respiratory symptoms, usually mild, or fever without a source.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Molina Gutiérrez MÁ, Ruiz Domínguez JA, Bueno Barriocanal M, de Miguel Lavisier B, López López R, Martín Sánchez J, et al. Impacto de la pandemia COVID-19 en urgencias: primeros hallazgos en un hospital de Madrid. An Pediatr (Barc). 2020. https://doi.org/10.1016/j.anpedi.2020.06.021