Necrotising fasciitis is an infectious disease associated with a high morbidity and mortality1; the most frequent causative agent is Streptococcus pyogenes,2 and early diagnosis and treatment requires a high index of suspicion.3
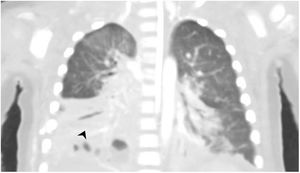
Clinical caseA boy aged 13 months with an unremarkable history was admitted due to toxic shock refractory to amines and respiratory distress syndrome secondary to necrotising pneumonia with empyema (Fig. 1) caused by S. pyogenes. The findings of the evaluation were suggestive of multiple organ failure, with ventricular dysfunction, liver and kidney failure and severe metabolic acidosis with hyperlactataemia, with the patient requiring venoarterial extracorporeal membrane oxygenation (VA-ECMO) for 10 days.
As the disease advanced, he developed distal ischaemia in the extremities (Fig. 2), with proximal progression and hard necrotic plaques. The CT angiogram evinced necrotising fasciitis in the right upper extremity with patchy myositis and extensive ischaemia in the extremities and trunk requiring escharotomy and debridement, in addition to diffuse enterocolitis with intestinal perforation (Fig. 3). At 23 days of admission, in a multidisciplinary meeting, the decision was made to withdraw life-sustaining treatment due to the need of disarticulation, extensive bowel resection and amputation of all four extremities.